https://mailchi.mp/d29febe6ab3c/the-weekly-gist-august-25-2023?e=d1e747d2d8
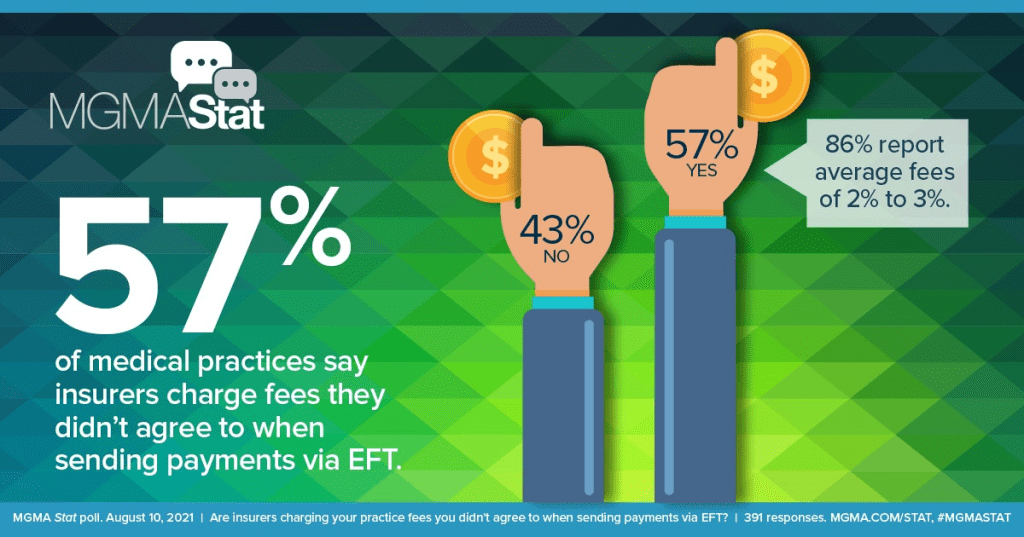
An investigative piece published this month by ProPublica documents how it came to be that nearly 60 percent of healthcare providers report being charged fees to receive electronic payments from insurers.
The fees, which can be as high as five percent of total reimbursement, were briefly forbidden by the Centers for Medicare and Medicaid Services (CMS), before the agency reversed its policy in 2018. The article follows one dogged physician’s efforts to uncover why CMS allows these fees. His voluminous stream of public records requests revealed a highly coordinated pressure campaign, mounted by the insurance industry through one particularly influential regulator-turned-lobbyist.
While the American Medical Association has urged the Biden administration to protect physicians from these fees, and the Veterans Health Administration is refusing to pay them, CMS is so far maintaining the position that electronic-payment claims-processing fees are permissible.
The Gist: Through partnerships with payment companies, who charge double the average fees of electronic bank transfers and share the spoils of their “virtual credit cards”, insurers are essentially using the same business model as credit card companies, skimming revenue from physician payments just as Visa and MasterCard do to merchants.
With the increasing consolidation of both insurers and claims processors, physicians are left with little recourse but to pay these fees, as nonelectronic payments come with infrastructure costs and payment delays.
While the shift to electronic payments spurred on by the Affordable Care Act was supposed to improve efficiency, this article offers yet another example of how efficiency gains can be captured by industry middlemen before they can be translated into provider and consumer benefits.

