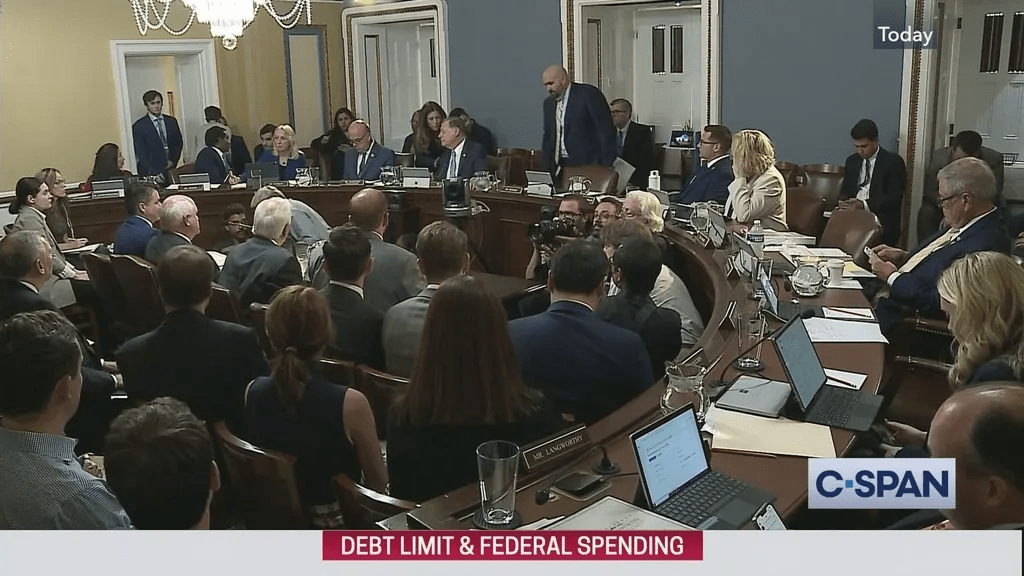
This week, all eyes will be on the U.S. Congress as the clock ticks toward a potential government shutdown. Whether lawmakers reach agreement on a continuing resolution to extend funding for30 to 60 days or the government shuts down at midnight this Saturday, it will have direct negative impact on consumer activities and spending in healthcare.
Background:
A shutdown alone is not apocalyptic for consumers: they’ve weathered 20 shutdowns averaging 8 days each since 1976 and recovered productivity shortfalls within 3-6 months. What’s complicating and most problematic for healthcare is its concurrence with equally threatening events and trends inside and outside healthcare:
- The resumption of Student Loan debt payments starting in October 1 impacting 900,000 Americans– 90% say they can’t!
- The probability the Federal Reserve will increase its federal borrowing rate by 25 basis points to 5.50 thus increasing interest costs and consumer prices.
- The slowdown in GDP growth and increase in fuel costs projected by economists and regulators.
- Increased workforce-management tension resulting in strikes, walkouts and slowdowns in labor-intense settings like auto manufacturing, nursing homes and hospitals.
- Medical inflation: technological advancements, increased demand, rising drug prices, expensive medical equipment, and increased administrative costs are contributors. According to the U.S. Bureau of Labor Statistics, prices for medical care are 5,274.47% higher in 2023 vs. 1935 (a $52,744.67 difference in value). Between 1935 and 2023, medical care experienced an average inflation rate of 4.63% per year, but in that period, working-age consumers who are privately insured paid a disproportionate and growing share projected to exceed 10% in 2023.
The health system’s economics are partially protected from shutdowns since funding for the Medicare and Medicaid is somewhat protected. That’s the status quo.
But the confluence of growing bipartisan Congressional antipathy toward the industry vis a vis regulatory reforms (i.e. price transparency, site neutral payments, DOJ-FTC consolidation constraints et al), high profile congressional investigations (i.e. PBMs and drug prices, role of private equity ownership), administrative orders from the White House and Governors (i.e.medical debt, value initiatives, organ procurement et al) and negative publicity challenging community benefits, CEO compensation and fraudulent activities erode the industry’s good will and expose it to unprecedented consumer risks.
Evidence in support of this assessment is substantial as illustrated in the sections that follow. There are no easy solutions. The U.S. health industry status quo is a B2B2P2C (business to business to physician to consumer) industry in which most decisions impacting what consumers ultimately spend for healthcare products and services are made for them, not by them. The direct costs associated with supply chain, technologies, facilities and R&D are closely guarded secrets. Indirect costs, administrative overhead, off balance sheet activities, partnerships and alliances even more.
What’s clear is that every sector in healthcare will be subject to scrutiny through an uncomfortable lens—the consumer. Prices matter. Service matters. Integrity matters. Transparency matters. Ownership matters. Purpose matters. And whether accurate or not, fair or not, comfortable or not, information accessible to consumers is readily accessible.
The shutdown over the debt limit might happen or be diverted. What will not be diverted is growing discontent with the medical system that the majority of consumers believe wasteful, expensive and self-serving. How the status quo is impacted is anyone’s guess, but it’s a good bet its future is not a cut-and-paste version of its past.

