https://mailchi.mp/9b1afd2b4afb/the-weekly-gist-december-1-2023?e=d1e747d2d8
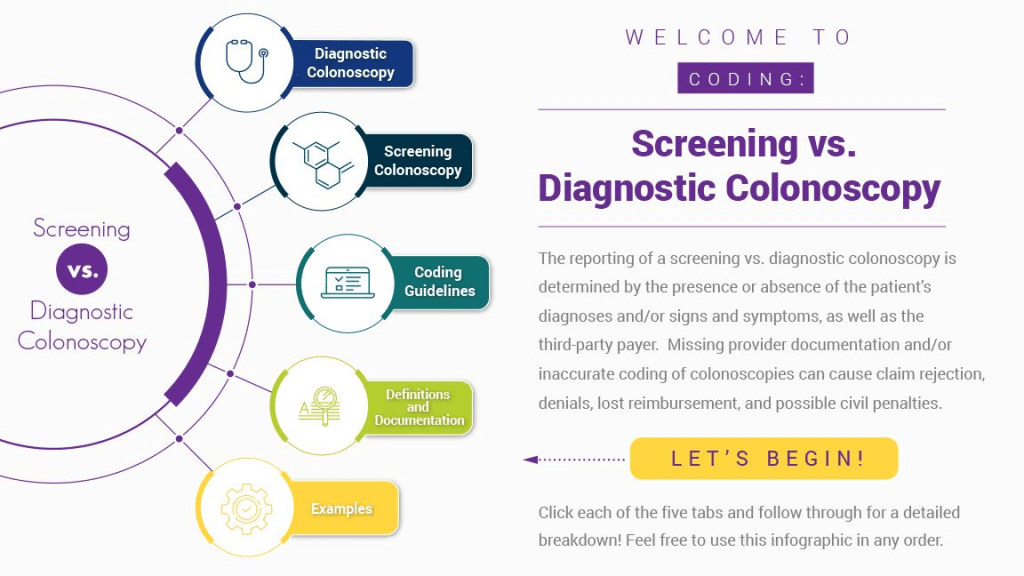
Published this week in Stat, this article explores the confusing payment landscape patients must navigate when receiving colonoscopies. While the Affordable Care Act requires that preventative care services be covered without cost-sharing, this only applies to the “screening” colonoscopies that low-risk patients are recommended to get every ten years.
But when procedures are performed at more frequent intervals for higher-risk patients, they are called “surveillance” or “diagnostic” colonoscopies, for which patients have no guarantees of cost-sharing protections, despite being essentially the same procedure, done for the same purpose.
If a gastroenterologist finds and excises one or more precancerous polyps during a screening colonoscopy, the procedure can leave the patient—especially one with a high deductible health plan—with a large, unexpected bill.
The Gist: Against the backdrop of a sharp rise in colorectal cancer rates among US adults under 65, articles like this are a frustrating demonstration of how insurance incentive structures can work against optimal care delivery.
Incentives should be carefully designed such that proven, preventative screenings—at the discretion of their doctor—are widely available to patients with minimal financial barriers. Surely, no one is “choosing” to have an “unnecessary” colonoscopy—as the procedure is notoriously disliked by patients.

