Coronavirus and Healthcare Reform

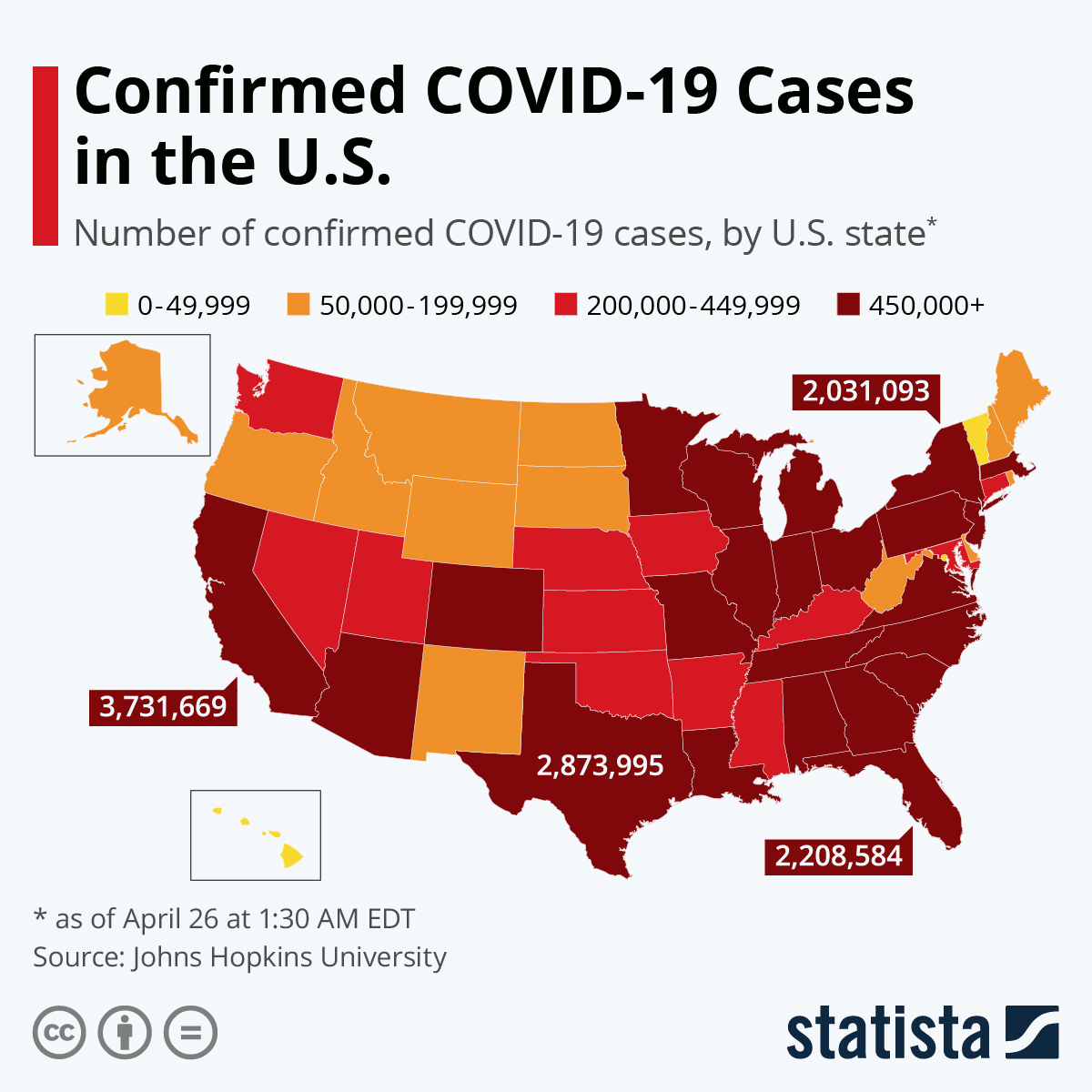
At this writing, the number of COVID-19 cases worldwide has reached 100,000 with 3,500 deaths. These numbers will be higher by tomorrow.
What does this have to do with U.S. healthcare reform? A lot.
Two current background articles drive home the point that a well-functioning public health system is critical for responding to a pandemic like 2019 coronavirus disease (COVID-19), especially in its early phases. And it means that the healthcare system – including a robust public health infrastructure — should be about health, not just about profit and greed.
Let’s Put This in Context: Is COVID-19 “Just Another Flu”?
WHO reports that annual cases of influenza A and B worldwide range from 3 to 5 million, causing 290,000 to 650,000 respiratory deaths. That’s a lot more than COVID-19, at least so far. So what’s the big deal?
The big deal is that, This Is Not a Competition, not an either-or between influenza virus and coronavirus. Otherwise this would be like asking, Would you rather be killed by an airplane crash, by tobacco-related cancer, or by pollution-related pneumonia? The answer is, of course, none of the above.
What these types of deaths and illness have in common is being in part preventable by known public health measures, with different interventions needed for each one. Likewise, influenza A and B deaths are in part preventable. Prevention relies on the elaborate and sophisticated worldwide influenza vaccine program. It includes monitoring influenza strains alternating between Northern and Southern hemispheres, annual adjustment of vaccine components, production, distribution, and public messaging.
But unlike influenza, currently COVID-19 is not preventable, since vaccine development and testing will take a year or more. And WHO is modeling that COVID-19 is at best only partially containable by general non-pharmaceutical measures. For example, one worst-case model of the pandemic estimates that two-thirds of the world’s population could be infected, once it runs its course. This has epidemiologists scrambling to calculate the actual transmissibility and actual mortality rates so as to refine predictions more accurately and to help plans for mitigating its spread.
So, no, COVID-19 is not “just another flu,” as the President implied in a March 4 off-the-cuff interview. COVID-19 is to be sure, a “flu-like illness,” but it has unique (as yet not fully characterized) epidemiologic characteristics, and it requires a completely different public health strategy, at least in the short- and medium-term. The President is reckless to minimize either disease – both diseases are widespread and lethal — especially since proper public messaging is a key to rallying a coherent response by individuals, communities, and nations.
How Bad Could It Be? Comparison to 1918 Spanish Flu
Could the COVID-19 pandemic wreak the same devastation as the 1918 Spanish flu? Spanish flu eventually infected 500 million people worldwide, effectively 25 percent of the total global population. And it killed up to 100 million of them. “It left its mark on world history,” according to University of Melbourne professor James McCaw, a disease expert who mathematically modelled the biology and transmission of the disease, and who was quoted today by the Australian Broadcasting Company (ABC).
What SARS-CoV2 (severe acute respiratory syndrome-corona virus strain 2), the agent that causes COVID-19 disease, has in common with the H1N1/Spain agent is novelty, transmissibility, and lethality. Novelty means that it is antigenically new, so that no one in the world is already immune or even partially cross-immune. Transmissibility means it’s easily spread by aerosol (coughing) or surface contact (hand to nose). Lethality means its significant death rate.
On the one hand, Dr. McCaw hopes that public health measures against COVID-19 will be more effective than in 1918. For one, experts and the general public now know about viruses. In 1918, virology was in its infancy.
“We’re not going to see that sort of level of mortality, that mortality was driven by the social context of the outbreak,” predicts Dr. Kirsty Short, a University of Queensland virologist, also quoted by the ABC. “We had a viral outbreak, at the same time as the end of a world war.”
In addition, modern medicine means much better care is available now than it was then. “We’ve already got a lot of scientists working on novel therapies and novel vaccines to try to protect the general population,” Dr Short says.
Professor McCaw points to an apparent initial success in Wuhan Province. “What’s happened in China gives very clear evidence that we can get what’s called the ‘reproduction number’ under one. So at the moment in China, on average, each person infected with coronavirus is passing that infection on to fewer than one other person. If people hadn’t changed their behaviour, we would have expected somewhere around the millions of cases in China by now instead of the comparatively small number of around 100,000.” So, he says, it looks like the transmissibility of coronavirus can be significantly modified through social distancing and good hygiene.
On the other hand, best-case calculations from these Australian epidemiologists appear to discount other factors that could actually worsen the pandemic in 2020 compared with 1918 – rapid international travel and higher concentration of people in urban centers.
Both Dr. Short and Professor McCaw admit that in the early days of a pandemic accurate predictions remain difficult to make.
Nevertheless, they both make clear that in battling the coronavirus, the national and international public health systems – and the public’s trust in them – will be key.
Public Health Approach Is the Key
The importance of public health actions is underscored by a second report today by two experts from the Center for Strategic and International Studies, a Washington think tank.
Samuel Brannen and Kathleen Hicks write in Politico.com,
Last October, we convened a group of experts to work through what would happen if a global pandemic suddenly hit the world’s population. The disease at the heart of our scenario was a novel and highly transmissible coronavirus. For our fictional pandemic, we assembled about 20 experts in global health, the biosciences, national security, emergency response and economics at our Washington, D.C., headquarters. The session was designed to stress-test U.S. approaches to global health challenges that could affect national security. As specialists in national security strategic planning, we’ve advised U.S. Cabinet officials, members of Congress, CEOs and other leaders on how to plan for crises before they strike, using realistic but fictional scenarios like this one.
Here are their conclusions:
- Early and preventative actions are critical. They praise bipartisan Congressional support, including $50 million allocated to the CDC Infectious Diseases Rapid Response Reserve Fund, the passage of the 2019 Pandemic and All-Hazards Preparedness and Advancing Innovation Act, and the continuation of the Global Health Security Agenda.
- Communication is vital—but a decline in trust makes it harder. A critical ingredient for addressing pandemics is public order and obedience to protocols, rationing, and other measures that might be needed. Today, public trust in institutions and leaders is fragile, with routine evidence of intentional disinformation by foreign actors and elected officials alike. Misstatements about science are particularly damaging to the credibility of scientists and health officials seeking to guide response to the pandemic. Amid the hyperpartisanship of the current U.S. political environment in a presidential election year, politicization of the coronavirus outbreak could undermine public health efforts.
- International cooperation is also key. A virus knows no borders, as we have already seen with the real-world outbreak, and here a concerning change is heightened mistrust among countries. In the midst of trade tensions, fraying of international relationships, increased meddling by one country in the internal politics of another, and growing military tensions in hot spots around the globe, organizations such as the World Health Organization are increasingly caught in the middle, unable to play their intended neutral function.
- The private sector will be vital to managing the outbreak. There’s a good reason the President gathered pharmaceutical executives on Monday, March 2. The U.S. federal government is rightly at the center of the response to this likely pandemic, but it is the private sector that holds the bulk of the technological innovation to producing treatments and cures. One bit of good news on this front: There is already in place a highly effective public-private partnership structure in the Coalition for Epidemic Preparedness Innovations, which is making important contributions in the current race for a vaccine.
- The principal conclusion of our scenario was that leaders simply don’t take health seriously enough as a U.S. national security issue. Congress holds few hearings on the topic, especially in the defense committees, and the White House last year eliminated a top National Security Council position focused on the issue.
Healthcare Reform: We’re All in This Together
The impending epidemic of coronavirus in the U.S. also brings up important practical questions in the whole healthcare system, as reported in, for example, the New York Times and Kaiser Family Foundation.
Who will have access to testing? Who will pay? Will copays designed to keep patients with trivial illnesses from overutilizing the health system now backfire by delaying their testing and care? These kinds of questions are not at issue in countries with universal access.
However, even those countries will struggle to cope with the pandemic. For example, the United Kingdom faces a shortage of intensive care unit beds after a decade of downsizing its bed capacity.
This drives home the point that public health infrastructure is necessary but not sufficient for managing a pandemic. Namely, the U.K.’s bed shortage shows that public health is but one component of the broader task of maintaining a nation’s strategic risk preparedness. Calculating the surge capacity of inpatient beds for an unexpected pandemic emergency should not be left just to hospital administrators. This is also why the President should restore both bio-preparedness positions dropped by him in 2018 from the National Security Council and the Homeland Security Department.
Conclusion: Right, Privilege or, Rather, Social Contract?
Is healthcare a right or a privilege? The coronavirus tells us, Neither. Instead, this virus reminds us that healthcare is better framed as part of the social contract, the fundamental duty of governments to their citizens to defend them from clear threats, both currently present and foreseeable, not only military, but also economic, cyber, and in this case biological. Can Americans and their leaders put aside petty polemical bickering over healthcare reform and recognize the healthcare system for what it is, part of the backbone of a healthy, resilient nation?