In my report June 10, I wrote: “The major sources of physician discontent are administrative hassles and unwelcome clinical oversight that create dissonance. They conflict with a false sense of autonomy that the majority of physicians imagined when choosing medicine. Cuts to reimbursement, participation in alternative payment models and medical inflation are manifestations of a system in which ‘suits’ are intruders who make rules, exact handsome salaries, generate corporate profits and distance physicians from patient care purposely… “
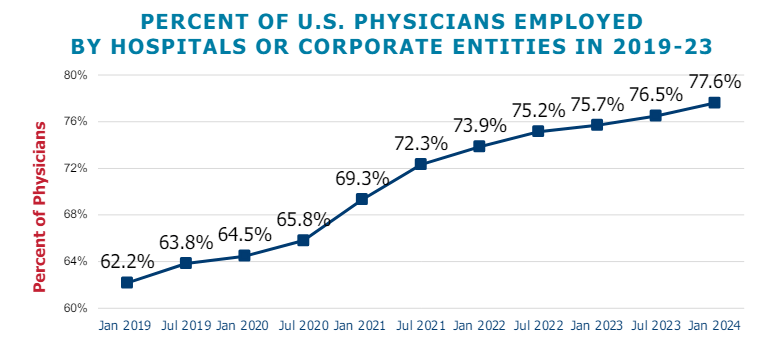
This assessment remains true today. Discontent among physicians is palpable and it’s magnified by a growing sense of financial despair among many clinicians. And it poses a unique challenge to hospitals that now employ more than half of America’s physician workforce.
In the “good ole days”, hospitals provided a place for physicians to ply their trade. They were credentialled to practice their chosen specialty, granted special parking, food and amenities and treated as the hospital’s most welcome customer. Made sense: physicians controlled most patient decisions about the hospital services they use. Physicians controlled the hospital’s revenue, sustainability and bonuses earned by administrators. Insurers brought privately-insured patients to doctors who charged them 1.6-2.5 times what Medicare paid and physician income was not threatened. That was then. This is now.
Today, insurers play a larger role. Consumer expectations have changed. Policymakers are paying more attention. And demand has shifted from inpatient services to outpatient, home and office settings for health and wellbeing services in addition to acute care. And the current forecast by CMS through 2032 predicts spending for hospitals will increase at a compound rate of 5.7% vs. 5.6% for physicians adding more hospital-physician financial tension to the system. Both well-above inflation and CDP growth prompting heightened pressure to spend less.
In anticipation, consolidation of hospitals into multi-hospital systems has been a staple in recent years: only 1 in 5 hospitals is independent these days, and most of these are small, rural or otherwise destined to independence for their uncertain future. Whether public, investor-owned or not-for-profit (or tax exempt as some prefer), the economic realities of running hospitals coupled with the regulatory constraints imposed by state and federal law forced all to re-think their future. And, for most, employing physicians directly was a means to an end of staying alive while the dust settles.
But the unintended consequence of physician employment is soured relationships between the employed physicians and their hospital:
their financial and emotional security has become tangled up by interactions with hospital leaders and former peers appointed to oversee their work.
And their views about their hospital have morphed to negativity based on four underlying beliefs:
- Hospitals spend too much on overhead and executive salaries and not enough on direct patient care.
- Hospitals are run poorly: we could run them better but they don’t listen to us.
- Hospitals get rate increases from Medicare and physicians get screwed.
- Hospitals need us more than we need them. But they don’t understand that.
On March 9, 2024, President Biden signed the Consolidated Appropriations Act, 2024, which included a 2.93% update to the CY 2024 Physician Fee Schedule (PFS) Conversion Factor (CF) for dates of service March 9 through December 31, 2024. But physicians saw that as not enough since their overhead increased even more. And for 2025, CMS is proposing to reduce average payment rates under the MPFS by 2.93% compared to the average amount reimbursed for these services in CY 2024 based on CY 2025 MPFS conversion factor decrease of $0.93 (or 2.8%) from the current CY 2024 conversion factor.
Understandably, physicians are upset. They’re not delusional that private insurers will make up the difference nor imagining hospitals will divert funds their way from brick, stick and tech priorities. But they’re speaking out expressing their views to anyone who’ll listen.
For hospitals that employ physicians, the issue of their financial anxiety requires urgent attention–not as one of many alongside 340B, site neutral payments and others but as the one at the top of the list. The issue is not whether physician income relative to other professions and average households is high. The issue is about managing physician expectations about their livelihood realistically and practically while improving their clinical acumen as professionals.
The core beliefs held by employed physicians about their hospitals may not be fair, objective or accurate, but they’re no less deeply felt and impactful. Hospital boards and C suite leaders would be well-served to refresh plans accordingly.

