September 2025 marks a significant shift in U.S. health policy, especially its approach to the public’s health.
- On September 9, the Make America Healthy Again (MAHA) Commission issued its first report pursuant to Executive Order 1421 which included 128 recommendations focused on reducing childhood chronic disease prevalence involving nutrition, chemical exposure, “over-medicalization” in pediatric care and more.
- On September 19, the newly-appointed CDC Advisory Committee on Immunization Practices (ACIP) issued new guidance on MMRV, Hep B and Covid vaccines for the coming season.
- On September 22, the FDA announced label updates for acetaminophen (Tylenol) during pregnancy urging caution. In response, the Blue Cross Blue Shield Association (BCBSA) and America’s Health Insurance Plans (AHIP) said they would not modify their coverage from prior guidance.
- On September 26, HHS and the Food and Drug Administration (FDA) announced enforcement actions against misleading DTC prescription drug advertisements aimed at protecting consumers by increasing transparency and accuracy in drug marketing.
All these as Congress faces a federal government shutdown Tuesday where debate centers on the President’s proposed FY2026 budget that cuts CDC funding by 53% compared to FY2024, eliminates over 100 public health programs and elevates readiness risks for outbreaks (e.g., measles) and more. Neither side wants a shutdown. Both see political advantage in staying their courses:
- Republicans enjoy strong MAGA support for federal spending cuts.
- Democrats enjoy voter majority support for extending ACA subsidies and maintaining health programs like SNAP with eligibility/program improvements.
But neither party is trusted by the majority of voters. The public’s distaste for the political system is palpable. Confidence in Congress is at an all-time low (Gallup), and trust in the Centers for Disease Control has plummeted:
“KFF polls have shown a steady decline in the share of the public saying they trust the CDC to provide reliable information about vaccines and other topics, from a high of 85% at the onset of the COVID-19 pandemic to 57% in our latest poll in July. This drop was largely driven by Republicans, among whom the share trusting the CDC dropped from 90% in March 2020 to 40% in September 2023 before rebounding somewhat following President Trump’s 2024 election victory and Kennedy’s appointment as HHS Secretary. While trust among Democrats remained high throughout Joe Biden’s presidency, it began to decline in President Trump’s second term just as Republicans showed signs of increasing trust. As of July, Democrats remained more trusting of the CDC than Republicans, but it’s unclear how recent events might affect trust among partisans going forward.”
In June 2024, Jonathan Samet, Colorado School of Public Health) and Ross C. Brownson (Washington University) offered this view:
“Public health system” is an optimistic misnomer in the United States, as it is used in reference to a fragmented and loosely connected set of entities. Moreover, the public health system, which is itself not readily delimited, is part of a system of systems that encompasses at least governmental public health; community-based organizations; the health care sector; and the education, training, and research of the academic public health and medical enterprises. The organization, policies, and politics of public health in the United States present opportunities and challenges. In the current decentralized model of public health, governance and are distributed across more than3,300 state and local health departments. “
My take:
Public health is a vital part of the U.S. health system but a stepchild to its major players. In reality, the U.S. operates a dual system: one that serves those with insurance (public and private) and another for those without. Public health programs like SNAP, HeadStart, Federally Qualified Health Centers et. al., serve lower income and under-insured populations and integrate with local delivery systems emergency services and during mass-events like pandemics, mass-casualties and disease outbreaks. Funding for public health programs is 2-5% of total health spending shared between local, state and federal governments.
Studies show food, housing and income insecurity—areas targeted by public health– correlate to chronic disease prevalence and health costs. Unlike most developed systems of the world which operate at a lower cost and produce better population-health outcomes, our system perpetuates a structural divide between healthcare and public health. Integrating the two is a necessary strategy for system transformation, but a difficult task given entrenched animosity toward “the system” held by public health leaders and funding pressures. The bridge between public health and the healthcare delivery systems is a two-lane road with lots of potholes at the federal level, and sometimes better in local communities. But funding seems to be an afterthought unless local communities deem it vital.
Public health is an opportunity for industry leaders to demonstrate pursuit of the greater good. Most public health programs are under-funded and dependent on a patchwork of local, state and federal appropriations (sometimes augmented by philanthropy) to keep their doors open. A particular opportunity exists for not-for-profit hospitals and health systems who enjoy tax exemptions to pursue integration as the core community benefits strategy, offering community leaders a sensible basis for eliminating duplicative services, expanding preventive health services and reducing demand for unnecessary hospitalizations resulted from uncoordinated care.
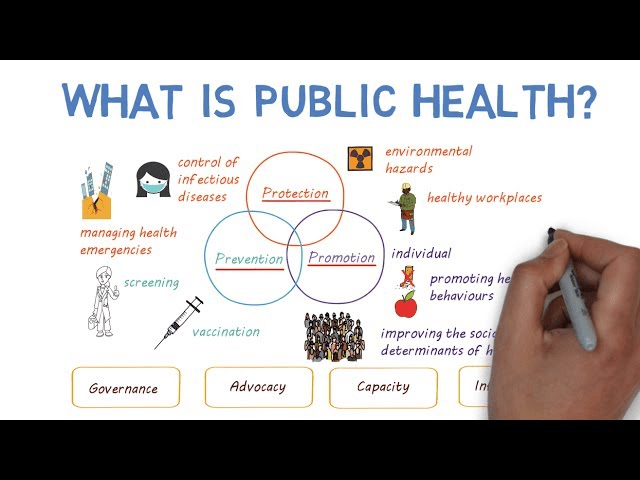
As the federal shutdown is addressed this week in DC, public health officials will be watching closely. As noted on the American’s Public Health Association website (www.apha.org) “The health care industry treats people who are sick, while public health aims to prevent people from getting sick or injured in the first place. Public health also focuses on entire populations, while health care focuses on individual patients.” Both are necessary but responsibility and funding for the public’s health seems in limbo.

