https://www.forbes.com/sites/robertpearl/2018/07/16/drug-companies/#72ce13501e41

If you’re a powerful American drug company, then you’ve had a strange couple of months. In that time, you’ve experienced a rainbow of emotions: fear, relief and, now, confusion and anxiety.
The roller-coaster ride, as you recall, began in mid-May when President Trump stood alongside HHS Secretary Alex M. Azar, in the Rose Garden of the White House, in front of a sign reading “Lower Drug Prices for Americans.”
As the president approached the mic, you watched with bated breath, remembering Trump’s campaign promise to drive down prescription drug prices to below a penny on the dollar. You always knew that’d be impossible but, then again, you thought, is anything really impossible?
Things started off poorly that morning. Almost immediately, Trump began denouncing the actions of drug manufacturers who, he said, were contributing to a “broken system.” He then urged all U.S. pharma companies to drop their prices, before deriding pharmacy benefits managers (PBMs) as “middlemen” who are getting “very, very rich” off the same broken system as you.
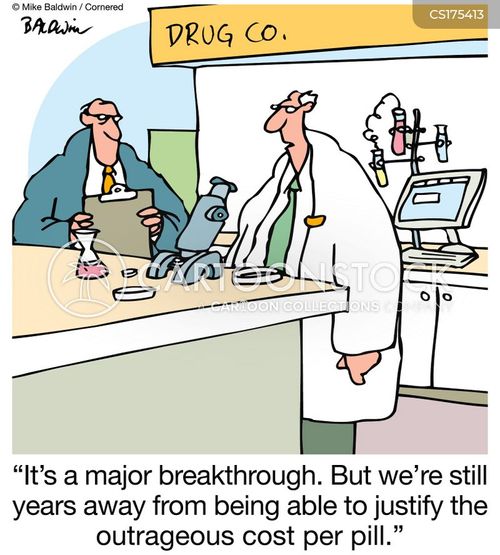
But when his speech ended, relief washed over you. After all, President Trump made no mention of his previous promise to negotiate lower drug prices for seniors enrolled in Medicare. He didn’t revive his vow to allow the importation of prescription medications, either. He didn’t discuss the popular notion of shortening pharmaceutical patents, nor that idea about requiring drug-companies to justify the price of new medications.
Granted, all these promises would be incredibly difficult to legislate. And, like most drug companies, you know that most of these ideas wouldn’t severely damage your bottom line anyway. But had the president committed to even one of them in his Rose Garden speech, he would have sent a clear message that this is not business as usual.
Instead, you and your colleagues took solace in his words. By late afternoon, the nation’s pharmaceutical, biotech and PBM stocks were up, not down. In the following weeks, drug companies interpreted Trump’s comments the same way drag-racers look at a stop signs—as more of a request than a rule.
Now, in fairness, President Trump and Secretary Azar had no intention of revealing a final, comprehensive set of proposals, rules or regulations on May 11. They set their sights on Tuesday, July 16—the official deadline for interested parties to comment on Secretary Azar’s blueprint Q&A. That’s when the real policy-making is set to begin. And, until early this month, most of the drug industry had been bracing for incremental, not radical, change.
But on July 1, Pfizer learned that it’s not safe to wake a sleeping bear. Thinking they had a clear runway, Pfizer’s corporate executives went ahead and raised list prices on more than 100 prescription drugs.
He followed that Tweet with a phone call and, within 24 hours, Pfizer had rolled back its price increases. Just like that, Trump had the drug industry’s full attention.
It stands as a public relations win for Trump in the lead up to the 2018 midterm elections. With recent polls indicating that 22% to 30% of Americans say healthcare is their top voting issue, Trump and the Republican party are wise to appear tough on rising drug prices (even if Pfizer is merely deferring its price hikes until later in the year).
Uncertainty and confusion, once again, permeate the drug industry. If the polls are even remotely accurate at predicting voter behavior this November, Trump and his cabinet will have good reason to take action.
I personally hope they have the courage to do so.
Unfortunately, the ideas Trump and Azar presented in the Rose Garden won’t be enough. They aren’t going to flatten the rapid rate of drug-price inflation or dramatically impact future price escalation.
So, alongside the administration’s proposed ideas, I offer four alternative policies that could make a real difference:
Leading idea No. 1: Take out the “middlemen”
In his May 11 address, the president went after PBMs, those insurance-company intermediaries between drug manufacturers and patients. At present, consumers know nothing about the prices these intermediaries negotiate or the size of the rebates/kickbacks they keep for themselves. Revenue for PBMs is determined as a percentage of all Rx drugs sold, which means there’s virtually no incentive to drive prices lower or replace the high-margin, brand-name drugs on PBM formularies with new, lower-cost alternatives. Federal legislation could require PBMs to operate transparently and work to lower out-of-pocket costs and drug prices for patients. However, there are way too many “ifs” with this approach to expect major change on the horizon.
A more frightening proposition for drug makers: Imagine if the U.S. government negotiated drug prices for all 55.5 million Medicare patients and made those costs publicly available so that everyone knew what price was fair and reasonable. Nearly all other nations do this. Why not the United States? Besides, Medicare already establishes prices for participating hospitals and doctors. Why not do the same for drug prices?
Leading idea No. 2: Make other nations pay more
Whether it’s NATO spending or wall-building, President Trump expects other nations to pony up for American interests. Most nations have made a habit of saying no. Now, rather than negotiating on behalf of Medicare for lower-cost medications (particularly Part B), the president has encouraged citizens of other countries to pay more for their prescriptions and, thereby, contribute an increased share of funding to drug-company R&D. Health ministers in other nations haven’t made this high priority for their 2019 healthcare agendas. They likely won’t. Even if drug prices were to rise in other countries, would drug manufacturers pass that added revenue on to American patients? Or to their shareholders? History suggests it’s the latter.
A more frightening proposition for drug makers: Require drug companies to document all the R&D dollars they spend in bringing a product to market. Further, force them to quantify and compare their drug’s efficacy to other drugs on the market. If pharmaceutical companies want generous patent protections (for products that often determine whether a patient lives or dies), their pricing can’t be capricious or simply what the market will bear. Prices should relate either to: (a) the cost of the drug’s R&D or (b) the superior clinical effectiveness of the medication.
Leading idea No. 3: Put prices in Rx ads
This is one of the most interesting concepts to come out of Trump and Azar’s blueprint. That’s because such a policy would, at least in theory, make it impossible for drug makers to hide their prices. USDA regulations already require companies to disclose possible side-effects in ads. Imagine if the administration also stipulated that pharmaceutical manufacturers must disclose their prices in ad copy, as well. For now, it’s unclear which costs the drug makers would need to disclose, given that patients and purchasers pay very different amounts for the same medications. Already, drug companies are using coupons and rebates, what critics deem to be clever schemes, to lower the advertised price for patients while simultaneously raising what they charge insurers—who ultimately pass those costs back to purchasers and patients through higher premiums.
A more frightening proposition for drug makers: Limit what U.S. pharmaceutical companies can charge. Period. American drug makers should be required to pay a penalty if they charge Americans more than 120% for the same medication as the 10 wealthiest nations pay on average. It’d be the same thing that happens when baseball teams exceed the salary cap. And when comparable medications exist at lower prices, TV ads would need to disclose that fact to viewers, as well.
Leading idea No. 4: Speed up generic medication approvals
This idea is a step in the right direction. Unfortunately, the president didn’t explain why generics currently undergo such lengthy delays for approval. The biggest hurdle is not government regulations, but drug company tactics. For most patented prescriptions, the generic versions have exactly the same chemical structure, and therefore, the same efficacy. As such, once a generic exists, there’s little or no reason to purchase the more expensive product. Knowing this, makers of the brand-name version use legal maneuvers to extend their patent protections before driving generic competitors out of business with their pricing and marketing leverage.
A more frightening proposition for drug makers: The government needs to change patent laws to protect patients first. Medications fall into two classifications. There are the small-molecule ones that often are available over-the-counter. With these, the generic version’s chemical structure is identical to that of the brand-name version. There also are the biologicals, so named because they are produced by living cells and organisms. Insulin is one example. Increasingly, this latter class of drugs has the highest price. These chemicals are too complex to be copied exactly, which is why the generic equivalents are labeled “biosimilars.” The solution here is to focus on the most expensive, large-molecule biologics first. In so doing, the government should force manufacturers to hand over drug samples to biosimilar companies 18 months before their patents end. This will speed up the development of biosimilars and fast-track the approval of lower-cost (but equally efficacious) medications. For patients with diabetes, this could lower the cost of life-saving insulin by 50% or more. Recent research from Yale shows up to 1 in 4 people with diabetes are injecting less insulin than they should simply because of the cost.
A Realistic Glimpse Into The Future Of Drug Pricing
Today, the pharmaceutical industry enjoys powerful patent protections and, thereby, monopolistic control over pricing. The consequence is that Americans are paying exorbitant prices for patented medications. The simplest solution is to strike a legislative balance that allows (a) drug companies to invent (and invest in) the next generation of breakthrough medication while (b) allowing the American people to afford the medications they need to stay healthy.
For most of the 20th century, the pharmaceutical world stayed within those guardrails. But over the past decade, profits have been way out of line with R&D and investment. The time has come to restore balance and reasonableness, regardless of what the national drug lobby wants.
Later this week, Secretary Azar will receive feedback on the administration’s blueprint and will begin drafting potential cost-cutting regulations. I encourage him and President Trump to use their authority to make drugs more affordable.
I suspect the pharmaceutical industry believes it will be business as usual, despite the campaign rhetoric and another Rose Garden event this coming fall. I hope the Secretary and the president have the courage to prove them wrong. The health of the American people depends on it.