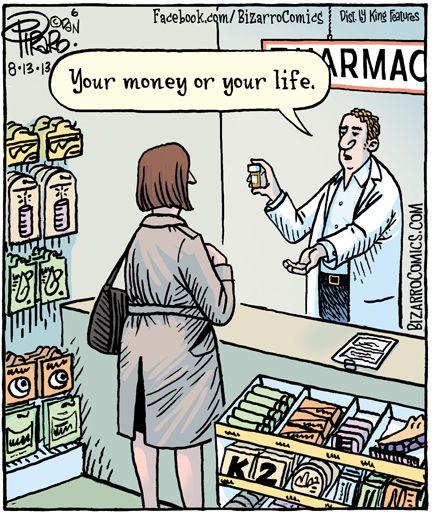
Everyone seems to want lower drug prices. 5 reasons why that hasn’t happened

Everyone seems to want lower drug prices. 5 reasons why that hasn’t happened.
Of all his campaign promises, President Trump’s vow to bring down drug prices was perhaps the most popular.
An assortment of interest groups spoke out loudly and passionately on the need for action, from hospitals to doctors to insurers to generic drug makers to patients themselves.
And in many ways, they seem to have the clout, and resources, to counter drug makers’ slick ad campaigns and lobbying firepower. Last year, the American Medical Association, America’s Health Insurance Plans, and the American Hospital Association together spent more than $45 million lobbying Congress, almost twice what the drug makers’ group, PhRMA, spent in the same time period.
Instead, congressional efforts to lower drug prices are at a total standstill. In interviews with STAT, lobbyists, lawmakers, and congressional staffers, Republicans and Democrats alike, said the most powerful health industry players conspicuously disagree about exactly how to move forward. Every group pushes its own priorities and strategies — a cacophony that makes it unlikely that crushing drug prices will change any time soon.
“They all say, ‘Yes, we should [lower drug prices], and someone else is responsible for it,’” Sen. Patty Murray of Washington, the top Democrat on the Senate Health, Education, Labor, and Pensions Committee, told STAT. “Everybody needs to come to the table and say what can my industry do, what can pharma do. … That will be how we solve this.”
Solving it, however, seems a stretch when just addressing it has gone nowhere. Despite President Trump’s insistence, on the campaign trail and in office, that he will lower drug prices, there has been no major federal effort to do so in the first year of his administration.
The disarray was on full display at a recent congressional hearing, when representatives from nearly every major trade group with any stake in the country’s drug prices — AMA, AHIP, and AHA included — spent almost an hour and a half testifying without more than a cursory discussion of how Congress could fix the problem. When they finally did talk solutions, outside of buzzy phrases like “increase transparency,” almost none of their answers matched.
So why can’t the broader health care industry agree on how to make drugs more affordable? Here are five factors.
1. Health care lobbyists are stuck playing defense.
When it comes to drug pricing, hospitals, insurers, and PBMs in particular have spent the last year fending off congressional inquiries into their own business practices — leaving little time to go on the offensive.
Meanwhile PhRMA has alternately pointed at hospitals, insurers, and PBMs as the profiteers in the current system.
It’s “lobbying 101, to muddy the waters,” according to Rep. Peter Welch (D-Vt.). And in the complicated world of drug pricing, it’s an effective strategy.
Drug makers’ efforts to vilify PBMs and to demand more transparency about their role in the supply chain are well-documented. The Washington Post earlier this year called pharma’s tactics against those players an effort to “start an industry war.”
They’ve opened a similar front against insurers, ramping up rhetoric and backing new patient groups that decry how higher deductibles and copays mean steeper costs for consumers, even when list prices don’t change much.
And they’ve accused hospitals of marking up the price of drugs and pocketing the difference, both in general and specifically as part of a push to overhaul the hot-button 340B drug discount program.
“That disarray you talk about, it’s not accidental,” Welch said. “The flames of that are fanned by pharma, [which] is doing everything they can to create confusion about what’s the right remedy,” he said.
The problem, according to Walid Gellad, who leads the University of Pittsburgh Center for Pharmaceutical Policy and Prescribing, “is that every part of the industry says things that are correct. It is correct that one of the reasons patients are feeling such high prices is because they have to pay coinsurance and big deductibles,” Gellad said, noting that pharma’s concerns with the PBMs and hospitals had some validity, too. “And it’s true that pharma sets the list prices high. They do do that.”
PhRMA spokesman Robby Zirkelbach also said there was a reason for lawmakers’ interest in so many players: the validity of the concerns. He pointed to data that showed slowing growth of prescription drug prices and increasing copays and deductibles.
“There’s no wonder that people are continuing to dig into this issue, and what they’re realizing is that to really be able to address the drug pricing concerns that people have raised, you’ve got to address some of the misaligned incentives in the system,” he said. “This is a complicated system, and we’ve got to look at how money flows across the system.”
And the tactic has successfully diverted lawmakers’ attention. Republicans in both chambers of Congress have held hearings in the past year looking at the “supply chain” that goes into the cost of drugs — broadening their spotlight from the companies that set the price to the other actors that can impact it. And lawmakers on both sides of the aisle say they want to better examine the vast array of players before they make any sudden policy moves.
“There are some that zero in on just one piece of the cost curve, so what I’m trying to do on the committee is look methodically at every piece,” Rep. Greg Walden, the Oregon Republican who chairs the influential Energy and Commerce Committee, told STAT. “We’re going to look at PBMs, we’re going to look at hospital costs, we’re going to look at what insurance costs. We’re going to look top to bottom.”
2. Congress isn’t jumping to act.
Beyond hearings, Congress hasn’t actually shown great appetite to tackle drug pricing. And that lethargy can dampen lobbyists’ enthusiasm to throw their weight and resources behind a given campaign or piece of legislation.
One physician lobbyist called it a “chicken and the egg” problem, wondering whether it would be Congress or the industries to first signal their motivation to act.
Case in point: the so-called CREATES Act. It’s one of the few pieces of drug price legislation that has the support of hospitals, insurers, doctors and a whole host of other groups and companies. But it’s languishing on Congress’s to-do list.
The bill, like its counterpart, the Fast Generics Act, takes aim at what supporters call delay tactics that drug makers use to keep generic competitors off the market. The legislation would give generic manufacturers that are legitimately seeking product samples the right to sue the drug makers if they refuse to hand over those samples.
It’s a small but meaningful change — the Congressional Budget Office has estimated that the legislation could save Medicare, Medicaid, and other federal government health programs more than $3 billion over 10 years.
And industry has been pushing the legislation, albeit without the same urgency that’s animated other priorities. Together, many of the trade associations — along with some three dozen other groups and companies, including Walmart, CVS, and AARP — formed a coalition, the so-called Campaign for Sustainable Rx Pricing, to push the bill. They hired a handful of lobbyists who are largely focused on the issue, too, to the tune of $440,000 over 2017.
But as one supporter put it, “it’s kind of telling that it has to be such an egregious abuse for everyone to coalesce.”
So far, drug makers have blocked attempts to include the measure in the 21st Century Cures Act that passed in 2016 or in last year’s reauthorization of FDA user-fee agreements, a priority for the drug industry. They say the bill will weaken protections for patients and spur “meritless, wasteful litigation.”
Supporters were nonetheless optimistic about the path forward for the bill. Several lobbyists backing the effort, along with staffers in both the House and Senate, told STAT there is momentum on Capitol Hill to include the measure in an upcoming spending package since it could help offset some other spending.
3. Each industry has very different priorities, even when they do agree.
Even when they do agree — as on CREATES, for example — health industry lobbyists don’t always prioritize the same issues. Some may have spent 2017 more focused on the repeal and replace of the Affordable Care Act than drug pricing. Others might have they used their meetings with lawmakers to defend a tax credit. Or perhaps some argue for other, more important drug pricing policies that need to be tackled first.
“When you work with these other groups, they rank [policy proposals] differently. There are certain things they want first. So it’s not only about finding solutions you can agree on, but about which ones you want to do first,” one patient advocate told STAT.
Drug makers, on the other hand? Pricing is their primary concern.
Other groups “have their own fish to fry, their own priorities,” said David Mitchell, the founder of the patient group Patients for Affordable Drugs. For drug companies, “it’s their number one issue: drug pricing. All the rest of them have their own number one issues, and drug prices aren’t it.”
4. All the major players have a stake in the status quo.
Academics had another easy explanation for the lack of consensus — and the lack of concerted effort — from health care industry groups that profess an interest in lowering drug prices. They all profit from the current system.
Hospitals are paying more for drugs for patients admitted to the hospital, but on the flip side, at least some facilities are profiting from reimbursements for drugs in outpatient settings and in their own specialty pharmacies, according to Peter Bach, the director of Memorial Sloan Kettering’s Center for Health Policy and Outcomes. PBMs also earn bigger rebates if the list prices are higher. And doctors, too, make more money under Medicare rules if they administer a more expensive drug to a given patient.
“People are paying these bills and the pie is getting bigger. Everyone’s arguing about where the knife comes in and cuts the slices of pie,” he said. “Everybody thinks everybody else is getting an unfair share.”
Gellad agreed.
“Everyone is making a lot of money. No one’s gone broke. So they don’t want to change things,” he said. “And that’s why the industry is not going to all agree to do something [on drug prices], because they’d all have to agree to lose money. Why would anyone agree to do that?”
5. There’s no silver bullet.
It’s not as if there’s one easy solution, ripe for the picking, if only groups could agree on it, several trade association officials told STAT. The piecemeal approach — getting behind policies like CREATES and then turning to other, smaller issues — may be the best way to approach the issue, they argued.
Similarly, lawmakers said there’s no one fix.
“The reason you haven’t seen all of the groups coalesce around one proposal — it’s not really clear what the solution is at this point because it’s such an opaque process,” Rep. Diana DeGette (D-Colo.) told STAT. “It’s hard to see what one solution there would be.”
Mitchell, along with a spokesman for the Association of Accessible Medicines, which represents generic manufacturers, also pointed to growing consensus behind smaller, targeted policies that would keep branded drug manufacturers from “gaming the system” — policies like CREATES and other changes to the patent system that could garner broader support. They each noted, too, that newly confirmed Health and Human Services Secretary Alex Azar, himself a former drug company executive, had voiced support for those changes during confirmation hearings.
They also preached patience. Bach, a former senior adviser to the Centers for Medicare and Medicaid Services, likened the push to the decades of jockeying between various environmental groups over fossil fuel regulation.
“Environmental regulation is a classic example of this,” Bach said. “You have this broad array of interested parties that would like to see movement, but the flavor of the movement they want, the ranking of their priorities, it’s not ‘one and only,’ even if it’s top [priority] — against a highly concentrated entity that specifically has a single agenda counter to it, with deep influence. That is a very hard row to hoe.”
“We are making progress,” he added. “But we get there in fits and starts.”