Even though most of the candidates have committed to some form of universal health care, the Democratic primary is turning into a debate about the future of the country’s health care system. Presidential hopefuls have proposed policies ranging from an ambitious four-year plan to transform Medicare into a universal single-payer system, in which the government pays for everyone’s health care and private insurance plans are effectively eliminated, to a more modest scheme that would leave the existing health care system intact but create a government-administered public insurance plan people could choose to purchase. But some of the candidates have been light on policy specifics, so it’s likely that health care will be a big topic at the debates and beyond.
In the abstract, focusing on health care makes a lot of political sense for Democrats. It was a top issue among Democratic voters in the 2018 midterms, and the Trump administration recently renewed its efforts to strike down the Affordable Care Act in the courts, which means the law could be hanging in the balance throughout the primaries and into the general election. A recent ABC News/Washington Post poll also found that Americans, by a 17-point margin, say that President Trump’s handling of health care makes them more likely to oppose him than to support him in 2020. By a similar margin, an Associated Press/NORC poll found that Americans trust Democrats more than Republicans on health care.
All of this means that Democrats are heading into the 2020 election cycle with a serious edge on an issue that has the potential to mobilize their base. But if the candidates pitch big, sweeping changes to the health care system without addressing voters’ concerns about cost and access, that advantage won’t necessarily hold up. And trying to sell Americans on a completely new system carries risks, even in the primaries.
Why do people care about health care so much?
First, it’s important to understand how health care has morphed over the past decade from just another issue to one of the issues voters care most about. In the 2018 exit polls, 41 percent of voters said health care was the most important issue facing the country, up from 25 percent in 2014 and 18 percent in 2012. (It wasn’t asked about in 2016.) And although Democrats are more likely to prioritize health care than Republicans, a Pew Research Center poll from January found that a majority of Republicans say health care costs should be a top priority for Congress and the president.
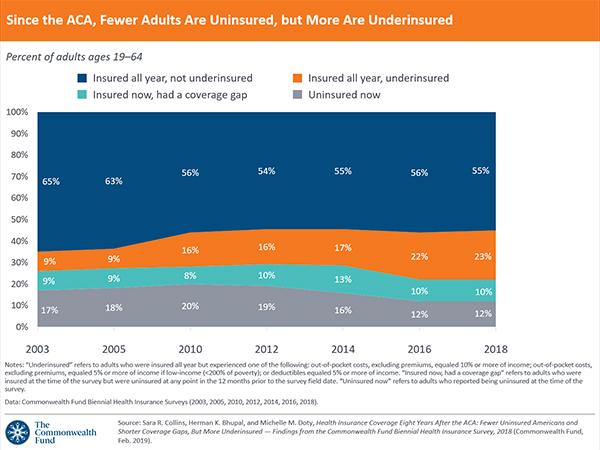
The reason? Health care is becoming more of a financial burden, according to Mollyann Brodie, executive director for public opinion and survey research at the Kaiser Family Foundation. Specifically, Americans’ out-of-pocket health care costs have risen significantly over the past decade, even for workers who get insurance through their jobs. In an economy that by many measures is doing well, health care — rather than something like taxes — is becoming one of voters’ most important pocketbook issues, she said. “If you’re worried about whether you or your loved ones can afford your next health care bill, that’s really a matter of life or death, so you can understand why this issue is moving to center stage politically.”
And Americans are increasingly likely to say that the government has an important role to play in ensuring access to health care. In November, Gallup found that 57 percent of Americans said they think it’s the federal government’s responsibility to ensure that everyone has health care coverage, up from a low of 42 percent in 2013. Support for the Affordable Care Act rose over the same period, too. But, notably, support for government intervention in the health care system was even higher before President Obama was elected and the ACA passed — in 2006, 69 percent of Americans thought the government should guarantee health care coverage.
While support for government involvement in health care is rebounding, it’s not clear how much change voters are really asking for. “The average American is first and foremost concerned about the financial problems facing their family,” said Robert Blendon, a professor of health policy and political analysis at Harvard. “They’re less worried about system-level concerns like health care spending and inequality. They want their existing coverage to be better and more affordable.”
What do voters want politicians to do?
Americans aren’t opposed to the idea of government-run health care, but there’s not a lot of consensus on what that would mean. For example, a recent Kaiser Family Foundation poll found that a majority (56 percent) of Americans favor a national “Medicare for All” plan. But according to a March Morning Consult poll, Americans are more likely to favor a plan that offers some kind of public option — a government-sponsored health insurance plan available in addition to existing private plans — over a system where everyone is enrolled in the same plan.
But this apparent contradiction makes sense, according to Brodie, because Americans are risk-averse when it comes to health care, and the switch to single-payer would affect far more people than the ACA did. Tens of millions of previously uninsured people received coverage under the ACA, but that number would be dwarfed by the 156 million people who get their insurance through their employers and could see their coverage change if the country switched to a single-payer plan. “Even if the current system isn’t working, transitions are scary,” Brodie said. “And people aren’t necessarily aware of what a national plan really means. When you start telling people that there might not be any more private insurance companies, that’s actually not a popular position.” For example, a January Kaiser Family Foundation poll found that support for a national Medicare for All plan dropped significantly when respondents were told it would mean eliminating private insurance companies.
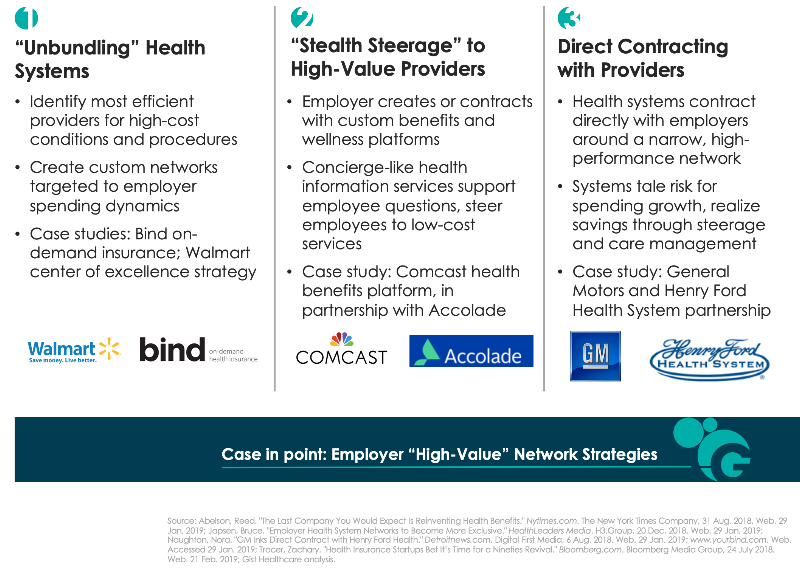
And when asked what health care policies they want Congress to prioritize, Americans don’t list Medicare for All first. Instead, according to a recent Kaiser Family Foundation poll, they want Congress to pass targeted measures that would lower prescription drug costs, continue the ACA’s protections for preexisting conditions and protect people from surprise medical bills. Only 31 percent of Americans say that implementing Medicare for All should be a top priority for Congress, compared to 68 percent who want lowering drug prices to be a top priority. Moreover, prioritizing Medicare for All is politically polarizing: Only 14 percent of Republicans support putting that kind of plan at the top of the to-do list, compared to 47 percent of Democrats.
Some health care issues get only one-sided support
Share of Republicans and Democrats who say each issue should be a top priority for Congress, and the difference between the parties
| Dem. | Rep. | Diff. | |
|---|---|---|---|
| Making sure the ACA’s preexisting condition protections continue | 82% | 47% | D+35 |
| Implementing a national Medicare for All plan | 47 | 14 | D+33 |
| Expanding government financial help for those who buy their own insurance coverage on the ACA marketplace to include more people | 36 | 18 | D+18 |
| Lowering prescription drug costs for as many Americans as possible | 77 | 66 | D+11 |
| Protecting people from surprise high out-of-network medical bills | 55 | 45 | D+10 |
| Repealing and replacing the ACA | 16 | 52 | R+36 |
However, smaller policy steps like lowering prescription drug costs and protecting people from surprise medical bills get more bipartisan support. Overall, Americans seem to be more concerned with fixing the current health care system than creating a sweeping new replacement — even if that replacement could address the issues they most want fixed in the current system.
What does this mean for the Democrats?
The complexity of Americans’ views on health care doesn’t change the fact that Democrats have a big advantage over Republicans on this issue, but it does mean that the individual candidates are in a tough spot because there’s no obvious unifying message they can adopt for the primary. And embracing a single-payer plan now could hand the GOP a weapon for the general election, allowing Republicans to frame the health care discussion around the Democrats’ controversial plan while glossing over Trump’s efforts to dismantle the ACA.
“The safest bet for a Democrat in the general election is to emphasize Trump’s track record on health care and say you’re going to make the ACA work,” Blendon said. The problem is that while that kind of argument might appeal to moderates, it’s likely to fall flat among a significant sector of the Democratic base that supports prioritizing a national Medicare for All plan over improving and protecting the ACA.
Democrats arguably still have an opening to make a case for a more ambitious health care overhaul, since voters still have relatively little information about what something like Medicare for All means. “It’s fine to support single-payer if you think that’s where the country needs to go, but you can’t just lean on principles like fairness or equality when you’re selling it,” said David Cutler, an economist at Harvard who advised Obama’s campaign on health care strategy. “You also have to tell voters, very specifically, what you are going to do to lower their costs and improve their coverage next year — not in 10 years.”
Even though Americans mostly prefer Democrats’ health care positions to the GOP’s, Democrats still risk alienating voters if they emphasize bumper-sticker slogans over concrete strategies for reducing the financial burden of health care. This is particularly important because their base of support for a single-payer system may be shallower than it appears, even within the party — especially when it comes to getting rid of private insurance. Big changes to the status quo are always politically challenging, but they may be especially risky when many Americans are concerned about losing the protections they already have.