https://www.commonwealthfund.org/blog/2019/can-states-fill-gap-preexisting-condition-protections

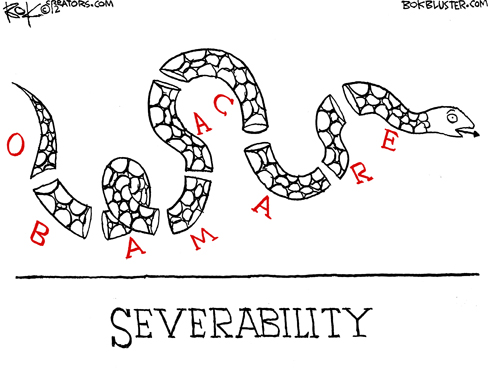
Once again, the Affordable Care Act (ACA) is under threat, this time in the form of Texas v. Azar, a federal lawsuit challenging its constitutionality. This litigation, now under consideration by the Fifth Circuit Court of Appeals, took an unexpected turn in March when the U.S. Department of Justice (DOJ) sided with the plaintiffs, urging the Court to strike the ACA down in its entirety.
On May 1, the administration filed a brief in support of this action. But even before this suit, DOJ had refused to defend key provisions that guarantee coverage of preexisting conditions. If the courts agree with the DOJ, it would invalidate every provision of the 2010 law.
As many as 20 million people nationwide would lose their coverage, while millions more could face insurance company denials, premium surcharges, or high out-of-pocket costs because of their health status.
ACA Protections for People with Preexisting Conditions
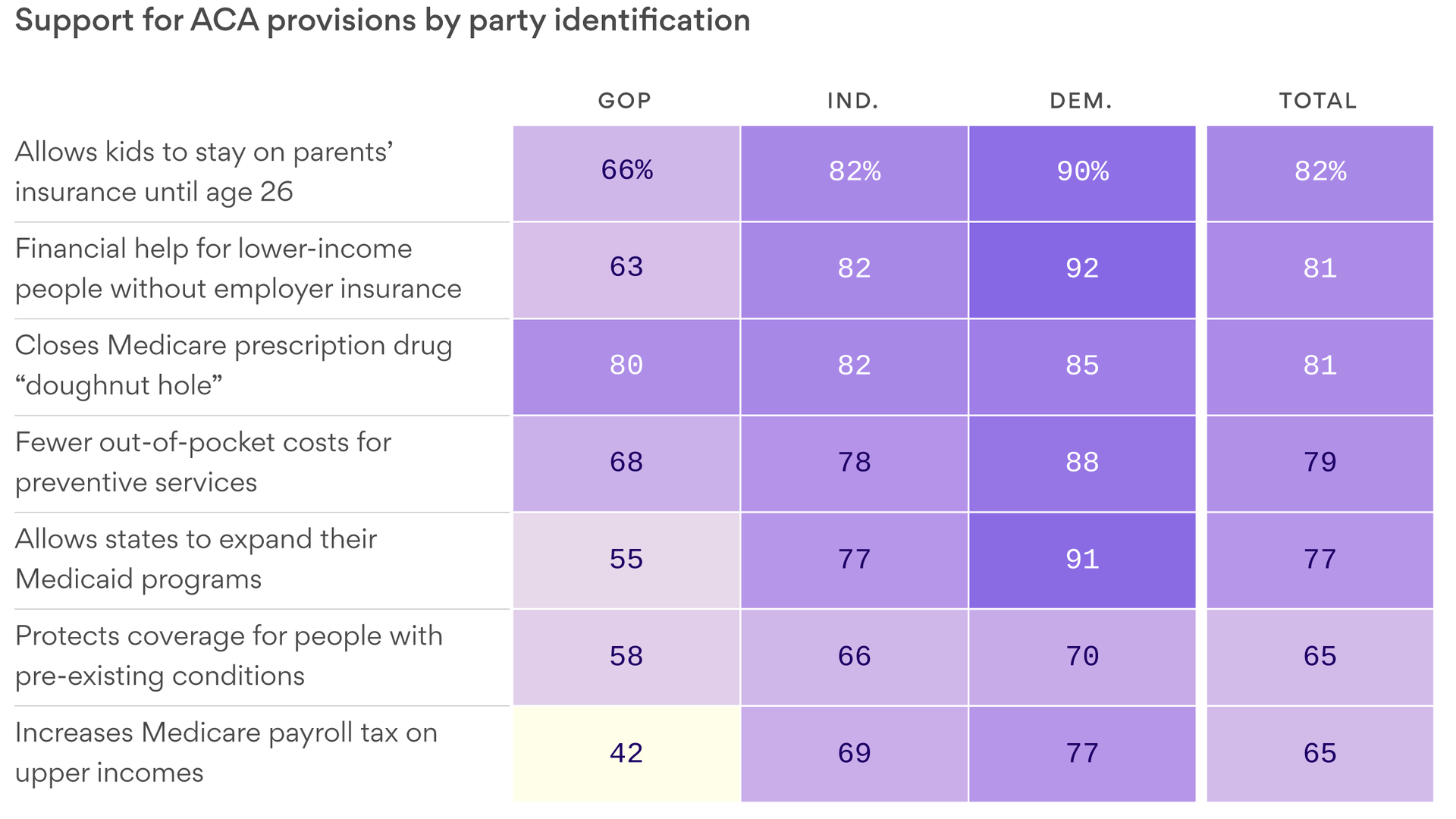
- Guaranteed issue. Health insurers are prohibited from denying an individual or employer group a policy based on their health status.
- Community rating. Health insurers may not use an individual or small employer group’s health status to set premiums.
- Preexisting condition exclusions. Health insurers and employer group plans are prohibited from refusing to cover services needed to treat a preexisting condition.
- Essential health benefits. Health insurers selling to individuals and small employers must cover a minimum set of 10 “essential” benefits: ambulatory services; emergency services; hospitalization; maternity and newborn care; mental health and substance use disorder services; prescription drugs; rehabilitative and habilitative services and devices; laboratory services; preventive and wellness services; and pediatric services, including oral and vision care.
- Cost-sharing protections. Health insurers and employer group plans must cap the amount enrollees pay out-of-pocket for health care services each year.
- Annual and lifetime limits. Health insurers and employer group plans are prohibited from imposing annual or lifetime dollar limits on essential health benefits.
- Preventive services. Health insurers and employer group plans are required to cover evidence-based preventive services without any enrollee cost-sharing.
- Nondiscrimination. Health insurers must implement benefit designs for individuals and small employers that do not discriminate based on age, disability, or expected length of life.
To help blunt potential fallout and prevent adverse effects for millions of individuals, several states are enacting bills to ensure that federal ACA protections become part of state law (see box). However, before the ACA, state efforts to require insurers to cover people with preexisting conditions resulted in large premium spikes and, in some cases, caused insurers to exit the market.
The ACA’s premium subsidies have had a critical stabilizing effect. If those subsidies are invalidated, states will have a hard time restoring them with state dollars. In addition, state regulation of self-funded employer plans is preempted under the federal Employee Retirement Income Security Act (ERISA), meaning the 61 percent of people with this type of job-based coverage can regain their protections under the ACA only if Congress steps in to restore them.
States Are Stepping Up, but Power to Fully Protect Consumers Is Limited
In a previous post, we found that at least four states (Colorado, Massachusetts, New York, and Virginia) had laws that would preserve key ACA preexisting-condition protections if the federal law is overturned. Since that time, seven more states (Connecticut, Hawaii, Indiana, Maine, Maryland,1 New Mexico, and Washington) have acted to preserve the ACA’s protections for their residents.
These bills take different approaches. Maine, New Mexico, and Washington passed comprehensive bills that would preserve all the protections listed above. The Connecticut, Hawaii, and Indiana laws are more narrowly focused. Hawaii and Indiana prohibit insurers from imposing preexisting condition exclusions; Connecticut aligns its benefit standards with the ACA. Maryland took a different approach, creating a workgroup to recommend ways to protect residents if the ACA is struck down. The governors of New Jersey and Rhode Island have issued executive orders directing their state agencies to uphold the ACA’s principles, by guarding against discrimination based on preexisting conditions and strengthening consumer protections to ensure access to affordable coverage.
Looking Forward
The Fifth Circuit Court of Appeals is expected to hear arguments in Texas v. Azar in July. Whatever that court decides, the losing party is likely to ask the Supreme Court to hear the case, and a ruling could come as soon as June 2020. With the future of the ACA hanging in the balance, at least 14 other states are considering legislation codifying some of the federal consumer protections during their 2019 sessions.