
Cartoon – Pharmaceutical Convention



Humana has brought a lawsuit against 37 pharmaceutical companies including Novartis, Mylan and Teva, alleging price fixing for numerous generic drugs.
The conspiracy increased the profits of the drug makers and others working with them at the expense of consumers, the government and private payers such as Humana, the lawsuit said.
Humana wants to recover damages it said it incurred from overcharges for certain widely-used generics, according to the lawsuit filed Friday in federal court for the Eastern Division of Pennsylvania.
Humana said the conspiracy is far-reaching among the drug makers to manipulate markets and obstruct generic competition. They agreed to fix, increase, stabilize and/or maintain the price of the drugs specified, along with other drugs, the court document said.
Humana accuses the pharmaceutical companies of secret meetings and communications at public and private events such as trade association meetings held by the Generic Pharmaceutical Association and others.
Humana’s allegations are based on personal knowledge and information made public during ongoing government investigations, the insurer said.
The pricing fixing is also under investigation by federal and state authorities, the lawsuit said.
The Attorneys General of 47 states, Washington, D.C. and Puerto Rico have filed a civil enforcement action against most of the named defendants, alleging agreements to fix 15 drug prices, the lawsuit said.
The Department of Justice has convened a grand jury to investigate a number of the defendants for price increases ranging from 100 percent to 400, 2,600 and 8,000 percent, Humana said.
The price increases are consistent with Medicare Part D price increases found by the Government Accountability Office for many of the subject drugs.
Among the drugs for which GAO identified “extraordinary price increases” — defined as a price increase of 100 percent or more — between the first quarter of 2011 and the first quarter of 2015, are, according to Humana, Amitriptyline, an antidepressant; Baclofen, a muscle relaxant and anti-spastic agent; Benazepril, an ACE inhibitor to treat hypertension; Clobetasol, a steroid and anti-inflammatory agent; Clomipramine, an antidepressant for obsessive compulsive disorder; Digoxin, used to treat heart failure and atrial fibrillation; Divalproex for seizure disorders; Doxycycline (in Hyclate form) an antibiotic; Leflunomide for rheumatoid arthritis; Levothyroxine, a thyroid drug to treat hypothyroidism; Lidocaine, an anesthetic; Nystatin, an antifungal for skin infections; Pravastatin to lower cholesterol; Propranolol, a beta blocker to treat hypertension; Ursodiol, to decrease the amount of cholesterol produced by the liver; and Verapamil, to treat hypertension, angina and certain heart rhythm disorders.
http://www.thefiscaltimes.com/2018/08/03/Chart-Day-Where-Prescription-Drug-Spending-Goes

U.S. spending on pharmaceuticals totaled $480 billion in 2016, according to a report published this week in Health Affairs.
“Two-thirds of this total ($323 billion) was captured by drug manufacturers in the form of net revenues,” the researchers from Memorial Sloan Kettering’s Center for Health Policy and Outcomes write. “The remaining third ($157 billion) was retained as gross profits in the supply chain. Of this share, nearly half was captured by retail and specialty pharmacies ($73 billion), and about 20 percent ($35 billion) by providers, such as hospitals and doctors’ offices. PBMs and wholesalers together captured approximately 25 percent ($23 billion and $18 billion, respectively).”
The takeaway: The analysis — which factors in the entire prescription drug supply chain, including pharmacies and pharmacy benefit managers as well as drugmakers themselves — shows that prescription drugs make up closer to 15 percent of all health care spending rather than the 10 percent more typically cited.
https://commonwealthmagazine.org/opinion/the-real-driver-of-health-care-spending/
An inefficiency gap is boosting costs — and profits
THE HEALTH CARE DEBATES that occurred in Washington over the past year were largely irrelevant to what’s happening in the health care marketplace. Republicans couldn’t repeal the Affordable Care Act but they made some changes that weakened it. Those changes will increase insurance premiums in the individual market but they do nothing to address the most significant trends that are evolving across the system. To understand the important trends, one must look elsewhere.
In March, three researchers from the Harvard T. H. Chan School of Public Health published a study in JAMA analyzing the well-known reality that the United States spends dramatically more on health care than other wealthy countries. They compared the US, where health care consumes 17.8 per cent of gross domestic product, to 10 comparable nations where the mean expenditure is 11.5 percent. Despite spending much less, the other countries provide health insurance to their entire populations and have outcomes equal to or better than ours. The researchers found that this inefficiency gap is primarily driven by two characteristics of the US system: the high cost of pharmaceuticals and inordinate administrative expenses.
The high administrative spending derives in large part from the fact that 55 percent of the people in the US are covered by private health insurers who embed their own billing requirements, expenses, and profit into the system. The next highest country in this regard is Germany, where 10.8 percent of the population is covered by private insurers. In many countries, there are no such middlemen.
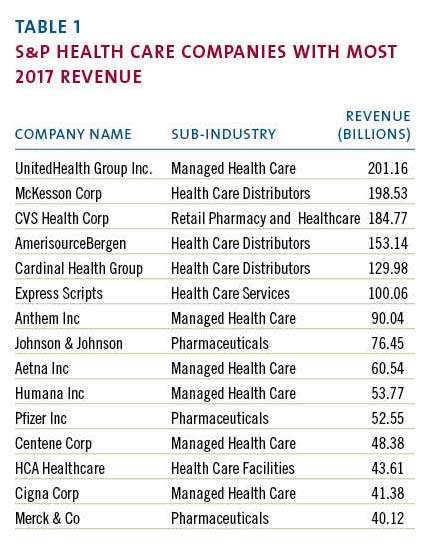
Coincidentally, when the JAMA study was published, the large publicly traded health care companies that dominate the US market had just finished disclosing their 2017 financial results. Examining those results provides additional insight into the economic forces that make our system so expensive and inefficient. The scale of the money involved is sometimes hard to grasp. The largest health care corporations, those included in the S&P 500, had almost $2 trillion in revenue last year. (Table 1)
Most of these enormous companies are engaged in one of two businesses: they’re either selling drugs or they’re selling health insurance. The excess costs reported by the Harvard researchers serve mainly to support the revenue of the companies in those fields.
The 2017 reporting of corporate profits was complicated by the passage of the new tax bill. But most companies also reported “adjusted net income,” which shows their normalized profits after accounting for the one-time impact of the tax law. The chart below (Table 2) uses the adjusted numbers to show the largest annual profits among S&P health care companies.
Health insurers such as United Health and retailers such as CVS have enormous revenue and impressive profits but, when profit is measured as a percentage of revenue, they can’t compete with biotech and pharma. The highest relative profitability, using the same reported adjusted results, is in the chart below. (Table 3)
These profit margins show that there are many situations where between a third and a half of every dollar spent on a prescription drug falls to the bottom line of the of the company that made it. This profit derives in large part from the enormous difference in drug prices in the US versus other countries where such prices are more effectively controlled.
The high administrative cost of the US system stems from the large portion of the market dominated by insurance companies looking to maximize their profits. Notwithstanding many news stories about turmoil in the insurance markets, 2017 was a banner year for the largest health insurers. The big players all had significant increases in annual profitability in 2017.
Note that Humana did not report “adjusted” numbers even though its profit was swollen by unusual events. A major distortion was a huge break-up fee the company received from a failed merger. That accounted for approximately $630 million in after-tax profit. Even discounting that, it was a very good year.
The revenue and profitability of these corporations support the proposition that high pharmaceutical prices and insurance-related administrative costs account for much of the extraordinary expense of our system. US health policy, or the absence thereof, has enabled these businesses annually to drive costs up for the benefit of their bottom line. That effect will continue. Not surprisingly, the big health care companies are developing new strategies to enhance their businesses and drive their profits going forward.
The term now heard often among health care giants is “vertical integration,” which means combining upstream suppliers with downstream buyers to control the flow of business. If this strategy persists, health care delivery will evolve significantly although it is unlikely to become less expensive. The most prominent current example of vertical integration is the planned $68 billion acquisition of Aetna by CVS.
How would these companies work together? A Wall Street analyst recently described the vision as a way to “identify high risk patients and preemptively get them into a Minute Clinic.” Thus, your health insurer could send you to a local store for diagnosis, treatment, drugs, and anything else you might need from the shelves. This will keep even more of the health care dollar under their control.
Similarly, Cigna is in the process of acquiring Express Scripts, a huge pharmacy benefits manager, for $54 billion, another attempt to bring more services under one roof. The combined company would have annual revenue of $142 billion and, presumably, enough leverage with drug companies to improve profits although not necessarily to lower costs to patients. United Health, a leader of vertical integration, previously bought a pharmacy benefit manager but co-pays and deductibles for its patients have continued to climb. United has aggressively acquired physician practices in recent years and is now in the process of buying DaVita Medical Group, which operates nearly 300 clinics and outpatient surgical centers.
More striking are reports of a potential but unsigned merger of Walmart and Humana, a combined company that would have revenue of $550 billion. Walmart is a large operator of retail pharmacies inside its stores and the logic is similar to the Aetna-CVS deal. Humana, a huge insurer, is separately in the process of acquiring a large home health business from Kindred so this could represent yet another level of vertical integration.

If this course continues, the health care system will evolve quickly, giving fewer and larger companies even more market leverage. Integration of this kind benefits the large corporations that initiate it but there is no evidence it will lead to lower costs, improved access, or enhanced quality. These changes are driven by highly focused corporate financial interests and are occurring without reference to public policy. That’s because there is no coherent public policy to guide these changes.
On May 11, President Trump made a long-awaited speech to reveal what he described as “the most sweeping action in history to lower the price of prescription drugs for the American people.” His typically firebrand language struck at “drug makers, insurance companies, distributors, pharmacy benefit managers, and many others” who contributed to “this incredible abuse.” His attack seemed to target the large public companies that have benefited from the abuse. Unsurprisingly, his speech did not include specifics. His staff then released tepid policy details, which immediately generated a significant upward spike in the biotech stock index as well as the stock prices of other large health care companies. For all the presidential bombast, investors saw Trump’s policy for what it is: indifference to the current path and no threat to high prices.
It is not in the interest of huge profit-making corporations to restrain the overall cost of the US health care system. In fact, their interest is served by driving health care expenditures higher. When combined with the spending analysis provided by researchers, the financial data disclosed by public corporations point to a path that the country must follow to make our system more coherent and less costly. Any progress will require driving down pharmaceutical pricing and reducing administrative costs imposed by middlemen. We are not doing that yet but, ultimately, we must.

At the core of the nation’s drug pricing problem is one fundamental fact: Drug companies enjoy government-sanctioned and -enforced monopolies over the supply of many drugs.
These monopolies result from patents awarded under federal law for novel molecules. Patents allow manufacturers to prevent competitors from selling the same drug for 20 years from the time the patent is filed. Given that the process of gaining regulatory approval to market their new drug takes time, research suggests new drugs have, on average, 12 to 13 years of market exclusivity.
Once new drugs are approved by the Food and Drug Administration, the monopolies assured by patents enable pharmaceutical companies to charge any price they choose. They generally pick prices that not only cover their development costs, but also generate profits that exceed those of most other industries: for example, the average profit margin for the 25 largest software companies (which are cited as having the same high R&D investment and low production and distribution costs as pharmaceutical companies) was 13.4 percent in 2015, while the average profit margin for the 25 largest drug companies was 20.1 percent in 2015. Drugmakers are also free to raise prices whenever they want at rates they alone determine.
The existence of patents does not totally prevent competition. Often, other companies introduce drugs that are distinct enough to justify their own separate patents and accomplish the same therapeutic goal. This results in competition that lowers drug prices, but often by not enough to make the medications affordable for many patients. In addition, the makers of patented drugs — for example, Mylan’s EpiPen and the weight-loss drug Suprenza — have developed effective mechanisms to extend the lives of their patents beyond 20 years. These approaches include making minor modifications in the formulations or packaging of drugs that have no clinical significance, as well as paying potential generic competitors not to introduce generic drugs.
That said, patents eventually expire, at which point generic drug companies can manufacture the drug and sell it at a much lower price. But even generic drug competition has been weakened recently by generic drug market monopolies, as these manufacturers have bought up their competition. As a result, the prices of old and familiar drugs have risen dramatically. The price of the cardiac drug isuprel has increased more than sixfold between 2013 and 2015, and the price of the antibiotic doxycycline has soared 90-fold over the same period.
As long as drug companies (or a small group) hold monopoly (or oligopoly) power over potent new therapies, there is no free market solution to lowering drug prices. Only a countervailing nonmarket force of equal strength can bring those prices down. Other western industrial countries, recognizing this, authorize their governments to step in and moderate drug prices for the benefit of their citizenry. Some set prices by fiat, while other negotiate with drug companies. In the latter case, the negotiations are sometimes guided by comparative effectiveness analysis that estimates the value of new drugs to patients. Of course, drug companies are free to walk away from such deals, but they generally choose not to, presumably because they still make money from those sales.
Drug companies say their monopoly earnings are necessary to sustain the research and development that produce new drugs. In effect they are saying that they need to be able to charge the very high prices we now see for patented drugs so they can innovate. This raises the questions of how much money society should allocate toward pharmaceutical innovation and who should decide. Setting those questions aside for the moment, we should be very clear about one thing: As long as pharmaceutical companies have uncontested market power to set prices for many patented and generic drugs, those prices will remain a huge problem for Americans and their elected representatives.

A U.S. Supreme Court ruling this week that upholds the constitutionality of a patent review process is being hailed as a win for consumers by the health insurance industry.
America’s Health Insurance Plans says the high court’s 7-2 decision in Oil States v. Greene’s Energy Group upheld the inter partes review process as a way to prevent drug manufacturers from inappropriately prolonging patent monopolies past the time intended by Congress.
“Patients had a lot at stake in the Supreme Court’s determination. Congress designed inter partes review as a quick and cost-effective way to weed out weak patents – including patents for branded prescription drugs,” AHIP said in prepared remarks.
Nicole S. Longo, senior manager of public affairs at Pharmaceutical Research and Manufacturers of America (PhRMA), said the ruling “was narrowly tailored, finding only that IPR is constitutional, not that it is efficient or fair.”
Longo pointed to another Supreme Court ruling this week, SAS Institute v Iancu, that raises concerns about the patent review process.
“SAS Institute v Iancu makes clear there are problems with the IPR process that need to be addressed. This decision points toward reforms to IPR, something stakeholders have raised time and again to the Patent and Trademark Office and members of Congress,” she said.
“Given this narrow decision, we call on Congress and the PTO to take steps to address the Supreme Court’s ruling in SAS Institutes v Iancu and concerns raised by stakeholders, and we stand ready to work with policymakers to make the IPR process more fair for all.”
According to Reuters, Congress created the reviews in 2011 to handle the perceived high number of flimsy patents issued by the patent office in prior years. Since then, the agency’s Patent Trial and Appeal Board has canceled all or part of a patent in about 80% of its final decisions.
The health insurance lobby said that the ruling ensures that millions of people will have faster access to affordable medicine.
“By upholding a faster and less costly patent review process, the Supreme Court has protected an important pathway that allows generic prescription drugs to get to patients faster. Generic drugs increase competition and choice in the market, which helps to lower drug prices,” AHIP said.
Longo said PhRMA has raised significant concerns with the IPR process because it requires drug makers to defend patents in multiple venues under different standards and with procedural rules that are less fair to patent owners than a federal court.
“This creates significant business uncertainty for biopharmaceutical companies that rely on predictable intellectual property protections to justify long-term investments needed to discover new treatments and cures,” Longo said.

If one message is becoming clear, it’s that increased concentration is harming consumers and leading to less competition, decreased choice and higher cost. The need for corporations to compete is dampened when markets are dominated by a small number of firms. Worse, when consumers don’t have the ability to discipline markets there is a lack of transparency or accountability.
Nowhere is that more true than in the market for Pharmacy Benefit Managers (PBMs) — the unregulated entities that control the reimbursement of drugs. These little known, unregulated middlemen are able to ramp up the cost of drugs by demanding rebates and other payments from drug manufacturers, and because of a lack of transparency and choice they are able to pocket much of these rebates, escalating the cost of drugs.
The Council of Economic Advisors, after a comprehensive review of rising drug costs, identified the lack of PBM competition as a major culprit. It found that only three PBMs controlled more than 85 percent of the market, “which allows them to exercise undue market power against manufacturers and against the health plans and beneficiaries they are supposed to be representing, thus generating outsized profits for themselves.”
The effect of market power on rebates and other payments to PBMs is clear. As one study found pharmaceutical manufacturer rebates skyrocketed 108 percent from 2011 to 2016 — rising from $66 billion to $127 billion in those five years.
Do skyrocketing rebates benefit consumers? Not much. As Health and Human Services Secretary Alex Azar has observed, “this thicket of negotiated discounts makes it impossible to recognize and reward value, and too often generates profits for middlemen rather than savings for patients.” Consumers pay more because their copays are based on list prices that are inflated by the rebates and other payments secured by the PBMs.
You do not need a Ph.D. in economics to figure out that the market is not competitive and that consumers are paying more than they otherwise would. FDA Commissioner Scott Gottlieb observed, “Kabuki drug-pricing constructs — constructs that obscure profit taking across the supply chain that drives up costs; that expose consumers to high out of pocket spending; and that actively discourage competition.”
Gottlieb identifies the lack of PBM competition and transparency as the real culprit. “The consolidation and market concentration make the rebating and contracting schemes all that more pernicious. And the very complexity and opacity of these schemes help to conceal their corrosion on our system — and their impact on patients.”
Now the two largest PBMs seek to merge with two insurance giants — CVS Caremark’s proposed acquisition of Aetna and Cigna’s proposed acquisition of Express Scripts. I have already observed how the CVS deal will harm competition and consumers. Adding another deal is like fighting a fire with gasoline.
These mergers rightly face tough scrutiny before the Antitrust Division of the Department of Justice. As the American Antitrust Institute’s recent comprehensive white paper documents in detail, these mergers significantly threaten competition in health insurance, pharmacy and PBM markets and must be blocked.
And as Rep. Rick Crawford’s (R-Ariz.) recent letter to Attorney General Jeff Sessions opposing the CVS/Aetna merger nicely emphasizes, such “vertical integration does not encourage competition or lower prices, but rather, could limit the choices and access for patients, driving out competitors while driving up prices and reimbursements for themselves.”
The reasons are straightforward and compelling. Many insurance companies want the service of an independent PBM — one not aligned with a rival insurance company. PBM services and the ability to control pharmaceutical costs are a crucial input for any insurance company, especially since the costs of drugs is an increasing part of the costs that need to be controlled.
Such reforms would include meaningful transparency and disclosure of rebates to payers, eliminating pharmacy gag clauses that prevent pharmacists from disclosing lower priced drugs, preventing PBMs from egregious reimbursement practices that force pharmacists to dispense below cost, and proper disclosure of pricing to pharmacists. As a basic first step both Express Scripts and Cigna must commit to pass through rebates to lower consumer costs as UnitedHealthcare has done.
But even these commitments are probably not enough. History tells a dismal story — past mergers have harmed consumers through less choice and higher costs as PBM profits have soared. No promises of good conduct can overcome the excessive concentration in the PBM market. The CEA recommended, “policies to decrease concentration in the PBM market … can increase competition and further reduce the price of drugs.” DOJ can begin this process by preventing the market from getting worse and simply blocking these mergers.
https://www.huffingtonpost.com/entry/opinion-beggelman-price-gouging_us_5ab45270e4b008c9e5f5c47f

It’s hard to remember now, but there once was a time when pharmaceutical companies were considered heroes, not villains.
In the 1920s, Dr. Frederick Banting and Charles Best discovered insulin could be purified and administered to diabetes patients via injection. Before this groundbreaking discovery, people living with diabetes were placed on starvation diets as a form of treatment, and many patients died.
Banting and Best understood the enormity of their discovery and considered insulin a public good. But as these researchers soon realized, insulin wouldn’t be able to save lives if patients couldn’t access it. They sold the rights to the drug to the University of Toronto for $1. The university, in turn, gave it to pharmaceutical company Eli Lilly for a 5 percent royalty so the company could manufacture at scale to meet the enormous demand. In 1923, insulin became widely available and saved countless lives, thanks to Banting and Best – and Eli Lilly.
Now, just under a century later, Eli Lilly and other insulin manufacturers are taking the exact opposite approach.
Big Pharma is pushing every scheme imaginable to squeeze money from the pockets of patients who need insulin to survive. Many with diabetes, faced with tripling insulin prices ($200 to $700 per month), are now forced to choose between life and rent. Some patients ― like 26-year-old Alec Raeshawn Smith, who aged out of his parents’ health insurance plan and whose job didn’t offer comprehensive coverage ― have died from a lack of affordable insulin.
Pharmaceutical companies can become heroes again, but only if they stop taking advantage of the patients who need them.
Eli Lilly says the company strives “to make life better for all those affected by diabetes around the world.” And because drug companies do save and improve lives (or, at least, are supposed to), the U.S. government allows them special privileges and protections. This includes tax breaks, government subsidies, extensive patent protection, free access to publicly funded scientific discoveries and more.
However, when drug companies use empty words to make promises they have no intentions of honoring, they do not deserve the public’s largesse.
Big Pharma has not shown any inclination to change its price gouging practices. On the contrary, drug companies continue to push higher costs despite the horrific impact this has both on human life and the U.S. economy. Price freezes in the U.S. are rare (and are exclusively voluntary). They also tend to be set at high levels, like the price “freeze” for the HIV drug Isentress, which caused a stir among HIV patients because of its exorbitant cost compared to competitive products.
Some companies have rolled back drug prices but typically only in response to public humiliation. Doctors at Memorial Sloan-Kettering publicly rejected Sanofi’s Zaltrap, a colon cancer drug, because it was priced twice as high as a competing product. Three weeks after the doctors’ announcement, Sanofi cut its price in half. This is why consumers shouldn’t be satisfied with price freezes; only rolling back prices will return us to reasonable drug costs.
Pharmaceutical companies do sometimes offer “solutions” to runaway drug prices, like value-based pricing and discount cards, but though these practices may help some, they are generally gimmicks meant to distract the public. Value-based pricing sets prices according to a drug’s perceived value rather than according to the actual costs of developing and manufacturing it. Such a practice can put a limit on the price of marginally effective drugs, but on the other hand, it increases the price of medications like insulin ― drugs that save lives but have been around for years and are cheap to produce. Discount cards are sometimes offered to a small subset of insured patients and do very little to help the vast majority of users or those who need the drugs most.
In the U.S., our 20 top-selling medications cost consumers three times more than the exact same drugs cost in Britain. I once paid $36 for a medication in Canada that costs me more than $700 here at home. In many European countries, government committees calculate “reference prices” for classes of drugs with similar ingredients, based on the costs to develop and manufacture them and their clinical effectiveness. That said, it’s probably not realistic to expect our politicians to agree to this kind of approach; in the U.S., pharmaceutical companies are some of the largest contributors to political campaigns, giving more than $2.3 billion over the past 10 years.
Big Pharma is pushing every scheme imaginable to squeeze money from the pockets of patients who need insulin to survive.
Our legislators, too afraid to challenge Big Pharma’s pocketbooks, continue to propose tepid solutions, like price transparency, that only work around the edges. Pharmacy benefit managers ― the industry middlemen who play a role in drug pricing ― take a piece of the pie, but how large a piece remains a secret. Legislation around transparency regarding undisclosed PBM deals could drive down drug prices somewhat, but it likely wouldn’t affect the baseline prices set by drug manufacturers.
The Right Care Alliance ― a group of patients, physicians, nurses, patient advocates, students and other community members with chapters around the country ― is currently organizing a campaign to target price gouging in the pharmaceutical industry. We are planning year-long grassroots actions, including town hall meetings, marches and demonstrations, to pressure Big Pharma to stop predatory pricing, particularly for life-saving medications.
We must force companies like Eli Lilly to address the gap between what they say they stand for and their actions. We must be loud with our demands to counterbalance the hold Big Pharma has on U.S. politics. Drug companies can become heroes again but only if they stop taking advantage of the patients who need them.

The man who embodied the phrase “pharma bro” and once urged his fans to pull a hair from Hillary Clinton’s head at a book signing has had a visit from pharma karma. The judge in Martin Shkreli’s fraud case, Kiyo Matsumoto, has sentenced the poster man for pharmaceutical company greed to seven years. Estimates are that Shkreli, 34, might get out in a couple of years if his behavior is good.
At his sentencing hearing, Shkreli apparently, and rather uncharacteristically, expressed contrition and shed enough tears that the judge called for the court officer to bring the defendant a box of tissues. Shkreli, in making his plea for leniency, tearfully told the judge that “the one person to blame for me being here today is me.” The judge apparently was unmoved, although the sentence is less than the 15 years the prosecution requested.
Shkreli drew the time after a jury found him guilty of one count of conspiracy to commit securities fraud and 2 counts of securities fraud. The same jury found him not guilty on an additional five counts, raising some hope from his legal team that his sentence would be light. The crimes, related to stock manipulation of shares in Retrophin, one of Shkreli’s companies, and ripping off hedge fund backers, could have carried a sentence of up to 20 years.
In February 2018, Matsumoto found that losses resulting from Shkreli’s crimes tallied up to $10.4 million.
Although he’s probably best known for overseeing a 5,000 percent price hike of a toxoplasmosis drug for HIV-positive patients, Shkreli’s post-pharmaceutical shenanigans caught a much attention as his venality while helming Turing Pharmaceuticals. He dropped $2 million on the sole copy of the Wu-Tang Clan album ‘Once Upon a Time in Shaolin,” which the judge has included in his assets. He harassed a journalist on Twitter, getting himself suspended, and seemed to want to fashion himself into the Snark King of Social Media.
His posturing ended up being his downfall.
While awaiting sentencing, Shkreli boasted that he would end up serving hardly any time and what time he did serve would be in the relatively posh environs of a “Club Fed” prison for white collar criminals. But after he exhorted Facebook followers to pluck a hair from Clinton’s head and offered $5000 per sample, the judge who sentenced him revoked Shkreli’s bail and ordered him to be placed in Brooklyn’s Metropolitan Detention Center, a far different experience for the pharma bro.
Although Shkreli is at the center of his own story, some believe that the industry overall is not blame-free. STAT journalist Adam Feuerstein has pointed out that the pharmaceutical industry can’t entirely disown Pharma Bro and his behavior, noting that Shkreli “was doing what lots of other biotech and pharma CEOs did, and still do to various degrees. Legally.”