https://www.kaufmanhall.com/insights/blog/gist-weekly-july-12-2024
On Wednesday, the Centers for Medicare & Medicaid Services (CMS) issued its proposed annual changes to physician payments in its 2025 Medicare Physician Fee Schedule Proposed Rule. Required by statute to maintain budget neutrality, CMS is proposing to reduce the conversion factor—which translates the cost of providing medical services into physician payments—by 2.8%.
This is expected to lower physician payments by 2.93% on average. The proposed rule also includes new telehealth flexibilities, changes allowing eligible accountable care organizations access to a quarterly advance on their earned savings, and new payments for providers that help patients at high risk of overdose or suicide.
The Gist: With CMS proposing to reduce physician payments for the fifth straight year, the American Medical Association and other physician groups are once again calling on Congress to avert these cuts.
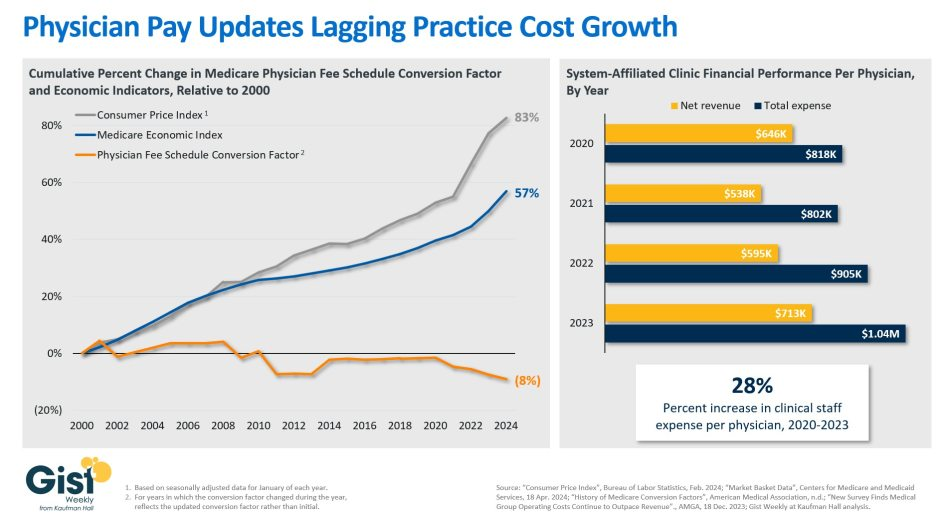
Congress has previously responded with “Band-Aid” solutions to temporarily reduce or eliminate reductions for the next calendar year, but physician groups are demanding a more comprehensive fix that ties Medicare payment updates to the Medicare Economic Index, a measure of practice cost inflation.
Medicare physician pay has declined 20% relative to practice costs from 2000 to 2021, and post-COVID inflation has only worsened the issue. Although lawmakers on Capitol Hill have explored various means of doing so, structural changes to Medicare budgetary policy face an uphill legislative battle in a presidential election year.