
Hawaii reclaimed its title as the healthiest state in United Health Foundation’s 29th annual America’s Health Rankings report, which placed Louisiana as the least healthy state in the nation.
The report is the longest-running annual assessment of the nation’s health on a state-by-state basis from United Health Foundation, an arm of UnitedHealth Group.
Here are seven takeaways from the latest 188-page report, which calculates state health by analyzing five categories: health outcomes, health behaviors, community and environment, policy and clinical care. (Specific information on ranking methodology can be found here.)
1. The five healthiest states in the U.S. are Hawaii (No. 1), Massachusetts, Connecticut, Vermont and Utah, in ascending order. These same states ranked among the top five in 2017.
2. The five states with the most room for improvement are Arkansas (No. 46), Oklahoma, Alabama, Mississippi and Louisiana, in ascending order. Last year, Mississippi ranked as the least healthy state.
3. Maine experienced the greatest improvement in the past year, moving up seven spots from No. 23 to No. 16. Maine saw the most improvement in the categories of health behaviors and community and environment measures, with specific progress in smoking and the rate of children in poverty.
4. California and North Dakota each climbed five spots to the No. 12 and No. 13 ranks, respectively.
5. Oklahoma saw the greatest decline in rank, falling four places from No. 43 to No. 47. The downturn was largely driven by changes in health behaviors in the past year, including an 11 percent uptick in obesity rates and a 14 percent uptick in physical inactivity.
6. The report highlights some major setbacks for health of Americans. More are dying prematurely than in prior years, and suicide, drug deaths, occupational fatalities and cardiovascular deaths all increased. Obesity increased nationally and in all 50 states since 2017. The report also finds self-reported frequent mental distress and frequent physical distress increased in the past two years.
7. At the same time, several improvements are worth noting. The number of mental health providers per 100,000 population increased 8 percent since 2017, and the percentage of children in poverty decreased 6 percent in the same time frame. Stark differences by state still exist, however.
Here are the overall health rankings for each state in 2018. The full report contains breakdowns of the determinants for each state’s rank.
- Hawaii
- Massachusetts
- Connecticut
- Vermont
- Utah
- New Hampshire
- Minnesota
- Colorado
- Washington
- New York
- New Jersey
- California
- North Dakota
- Rhode Island
- Nebraska
- Idaho
- Maine
- Iowa
- Maryland
- Virginia
- Montana
- Oregon
- Wisconsin
- Wyoming
- South Dakota
- Illinois
- Kansas
- Pennsylvania
- Florida
- Arizona
- Delaware
- Alaska
- North Carolina
- Michigan
- New Mexico
- Nevada
- Texas
- Missouri
- Georgia
- Ohio
- Indiana
- Tennessee
- South Carolina
- West Virginia
- Kentucky
- Arkansas
- Oklahoma
- Alabama
- Mississippi
- Louisiana
Click to access ahrannual-2018.pdf


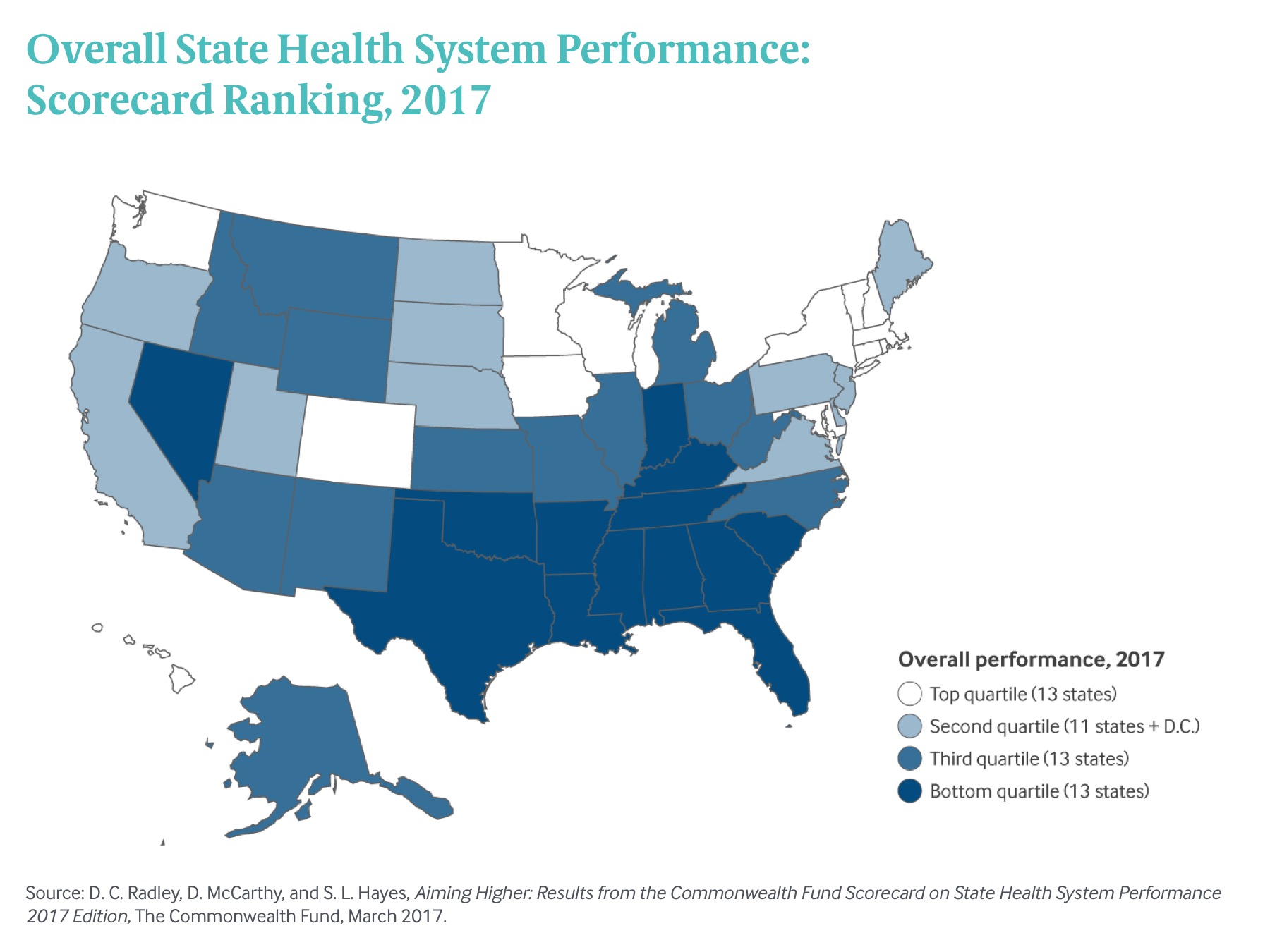
 Exhibit 1: Overall State Health System Performance: Scorecard Ranking, 2017
Exhibit 1: Overall State Health System Performance: Scorecard Ranking, 2017