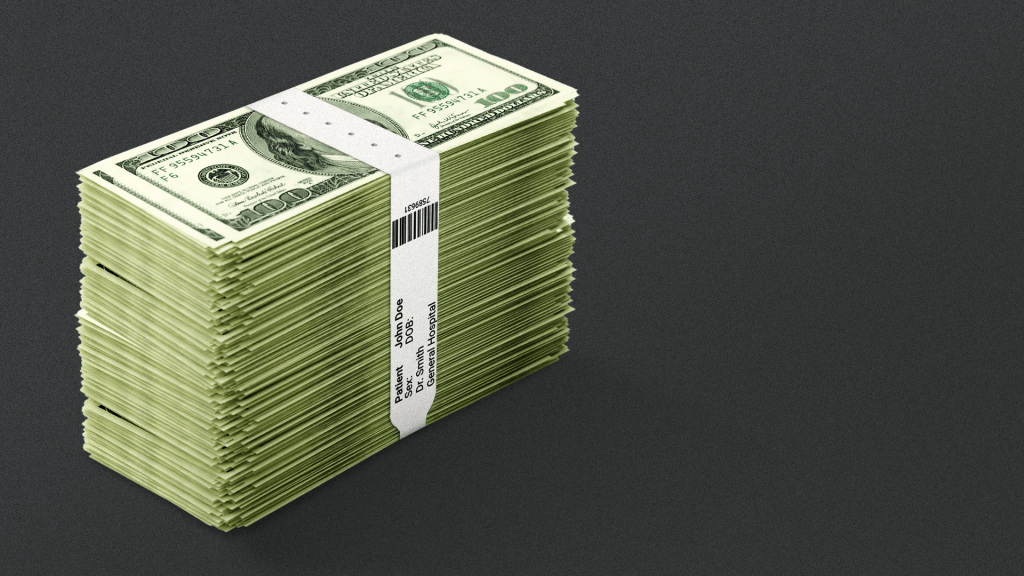
The Trump administration is shaking up how health systems are paid for outpatient care with a plan that could reduce Medicare hospital spending by nearly $11 billion over the next decade.
Why it matters:
It’s a big step forward for “site-neutral” payment policies that have been touted as a way to save taxpayers and patients money, but that hospitals say will lead to service cuts, especially in rural areas.
Driving the news:
Medicare administrators on Friday finalized a proposal to reduce what the government pays hospitals to administer outpatient drugs, including chemotherapy, at off-campus sites.
- The move would equalize payment rates to hospitals and physician practices for the same services — an idea that Congress debated last year but didn’t act on in the face of aggressive hospital lobbying.
- Medicare now pays about $341 for chemotherapy administration in hospital outpatient facilities, compared with $119 for the same service delivered in a doctor’s office.
- Medicare next year will also start to phase out a list of more than 1,700 procedures and services only covered when they’re delivered in an inpatient setting.
What they’re saying:
The policy changes will give seniors more choices on where to get a procedure and potentially lower out-of-pocket costs at an outpatient site, the Centers for Medicare and Medicaid Services said.
- Some health policy experts said the change will help make Medicare more affordable.
- “We hope the administration will continue its efforts and adopt site neutrality for other services in future rules,” Mark Miller, executive vice president of health care at Arnold Ventures, said in a statement.
The other side:
“Both policies ignore the important differences between hospital outpatient departments and other sites of care,” Ashley Thompson, a senior vice president at the American Hospital Association, said in a statement.
- “The reality is that hospital outpatient departments serve Medicare patients who are sicker, more clinically complex, and more often disabled or residing in rural or low-income areas than the patients seen in independent physician offices.”
- Hospitals indicated before the rule was finalized that they’d challenge the policy in court if CMS moved forward.
Hospital outpatient departments still will see an $8 billion overall increase in their Medicare payments in 2026.
- But the Trump administration contends that new technologies and other factors are shortening recovery times for procedures done on an outpatient basis.
Between the lines:
Health systems still scored a small win when CMS dropped a plan to speed up the repayment of $7.8 billion in improper cuts the first Trump administration made to safety-net providers’ reimbursements in the federal discount drug program.
- The policy would have clawed back the money from hospitals’ Medicare reimbursements. Scrapping the idea “helps preserve critical resources for patient care during an already challenging time,” Soumi Saha, senior vice president of government affairs at Premier, said in a statement.
- Still, CMS said it may try again in 2027. And law firm Hooper Lundy Bookman is already sending out feelers to hospitals willing to challenge the version of the repayment plan that will go into effect next year, per an alert sent Friday night.
What we’re watching:
Whether health systems challenge the site-neutral payment changes. The hospital payment plan came weeks later than expected and will make it harder for facilities to update billing, revise their budgets and train staff, Saha said.
- The administration is also launching a survey of hospitals’ outpatient drug acquisition costs next year, which is seen as a prelude for cutting reimbursements under the discount drug program.

