https://www.healthcaredive.com/news/despite-provider-claims-hospital-ma-not-associated-with-improved-care-ne/569671/

Dive Brief:
- Hospital consolidation is associated with poorer patient experiences and doesn’t improve care, according to a study published Thursday in the New England Journal of Medicine, refuting a common provider justification for rampant mergers and acquisitions.
- The study funded by HHS’ health quality research division, the Agency for Healthcare Research and Quality, found that acquired hospitals saw moderately worse patient experience, along with no change in 30-day mortality or readmission rates. Acquired hospitals did improve slightly in clinical process, though that can’t be directly chalked up to the results of an acquisition, researchers found.
- It’s further evidence that bigger isn’t always better when it comes to hospitals, and adds onto a heap of previous studies showing provider mergers lead to higher prices for commercially insured patients.
Dive Insight:
Hospitals continue to turn to M&A to navigate tricky industry headwinds, including lowering reimbursement and flatlining admissions as patients increasingly turn to alternate, cheaper sites of care. Provider trade associations maintain consolidation lowers costs and improves operations, which trickles down to better care for patients.
Though volume of deals has ebbed and flowed, hospital M&A overall has steadily increased over the past decade. The hospital sector in 2018 saw 90 deals, according to consultancy Kaufman Hall, up 80% from just 50 such transactions in 2009.
Thursday’s study analyzed CMS data on hospital quality and Medicare claims from 2007 through 2016 and data on hospital M&A from 2009 to 2013 to look at hospital performance before and after acquisition, compared with a control group that didn’t see a change in ownership.
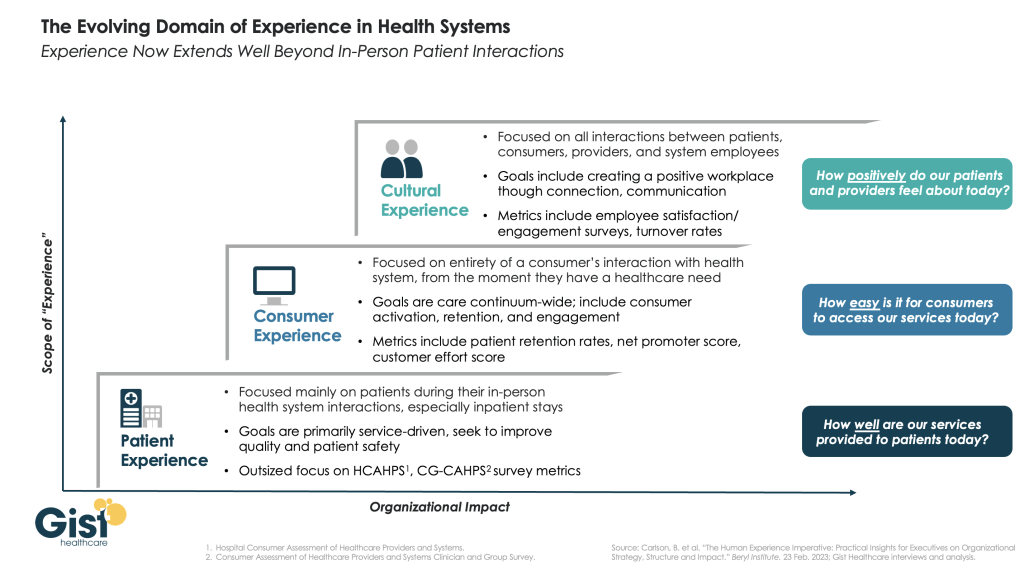
American Hospital Association General Counsel Melinda Hatton took aim at the study’s methods to refute its findings, especially its reliance on a common measure of patient experience called HCAHPS.
“Using data collected from patients to make claims about quality fails to recognize that it is often incomplete, as patients are not required to and do not always respond comprehensively,” Hatton told Healthcare Dive in a statement. “The survey does not capture information on the critical aspects of care as it is delivered today.”
The results contradict a widely decried AHA-funded study last year conducted by Charles River Associates that found consolidation improves quality and lowers revenue per admission in the first year prior to integration. The research came quickly under fire by academics and patient advocates over potential cherrypicked results.
A spate of previous studies found hospital tie-ups raise the price tag of care on payers and patients. Congressional advisory group MedPAC found both vertical and horizontal provider consolidation are correlated with higher healthcare costs, the brunt of which is often borne by consumers in the form of higher premiums and out-of-pocket costs.
A 2018 study published in the Quarterly Journal of Economics found prices rose 6% after hospitals were acquired, partially due to limiting market competition. Groups like the left-leaning Center for American Progress have called for increased scrutiny from antitrust regulators as a result, but — despite snowballing M&A — there’s been little change in antitrust regulation since the 1980s. The Federal Trade Commission won several challenges to hospital consolidation in the 2010s, but the agency only contests 2% to 3% of mergers annually, according to MedPAC analysts.
Providers, like most actors across the healthcare ecosystem, are increasingly under fire for high prices and predatory billing practices. President Donald Trump’s administration finalized a rule late last year that would force hospitals to reveal secret negotiated rates with insurers, relying on the assumption that transparency would shame both actors into lowering prices.
A cadre of provider groups led by the AHA sued HHS over the regulation, arguing it violates the First Amendment and would place undue burden on hospitals, while potentially stifling competition. The lawsuit is currently being reviewed by the U.S. District Court for the District of Columbia.