Top government health officials on Sunday warned that the United States will probably see record numbers of coronavirus cases and hospitalizations as the omicron variant spreads rapidly and forces Americans to again grapple with the dangers of a pandemic that has upended life around the globe.
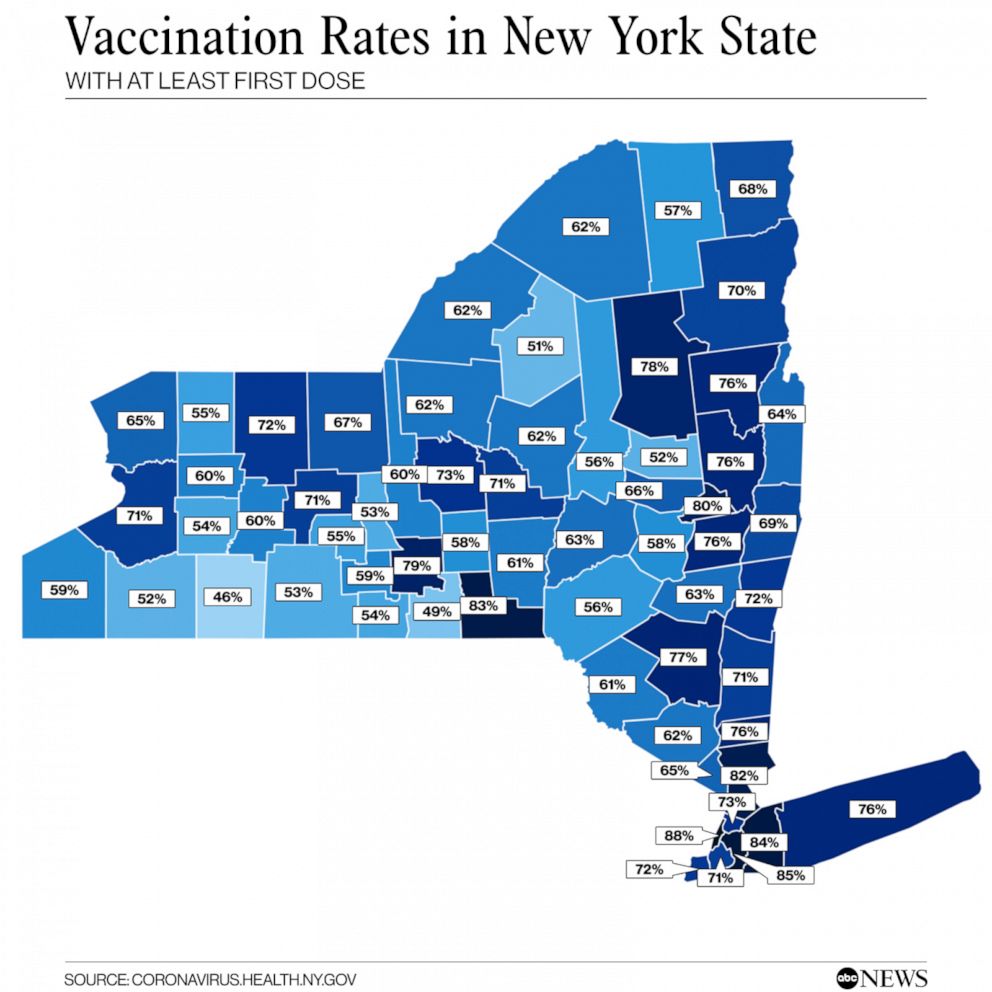
“Unfortunately, I think that that is going to happen. We are going to see a significant stress in some regions of the country on the hospital system, particularly in those areas where you have a low level of vaccination,” Anthony S. Fauci, the nation’s leading infectious-disease specialist, said on CNN’s “State of the Union” when asked whether the United States could see record numbers of cases, hospitalizations and deaths.
Fauci described the variant as “extraordinary” in its transmissibility, with a doubling time of two to three days. It accounts for 50 percent of coronavirus cases in parts of the country, which meant it would almost certainly take over as the dominant variant in the United States, he added.
“It is going to be a tough few weeks, months, as we get deeper into the winter,” Fauci said.
On CBS News’s “Face the Nation,” Francis Collins, director of the National Institutes of Health, said that cases will rise steeply over the next couple of weeks and that the country could soon see 1 million new cases a day tied to the omicron variant, dramatically exceeding the record of about 250,000 new cases per day set in January.
“The big question is, are those million cases going to be sick enough to need health care and especially hospitalization?” Collins said. “We’re just holding our breath to see how severe this will be.”
Fauci and Collins painted a stark but realistic picture of the winter ahead, on the heels of a week of coronavirus-related setbacks. Coronavirus cases, hospitalizations and deaths rose across much of the country last week, with officials warning of a surge just as millions of Americans — already weary after nearly two years of the pandemic — are expected to travel for Christmas and New Year’s. On Friday, Pfizer and BioNTech announced that coronavirus vaccines for children younger than 5 would be pushed back further into 2022, as the companies modified their trials to include a third dose. On Sunday, New York, one of the country’s early epicenters in the pandemic, reported 22,478 cases.
Health officials have continued to urge the unvaccinated to get their shots and those who have received only two doses of either the Pfizer or Moderna mRNA vaccines to get booster doses. Vaccines cannot be the only layer of protection against the omicron variant, Fauci said, but defeating the pandemic would not be possible without them.
There are still safe ways for vaccinated people to get together for the holidays, including wearing a mask while traveling, testing beforehand and knowing the vaccination status of everyone present at indoor celebrations, Fauci said on “Face the Nation.”
“If you do these things, I do believe that you can feel quite comfortable with a family setting,” he said. “Nothing is 100 percent risk-free, but I think if you do the things that I just mentioned, you’d actually mitigate that risk enough to feel comfortable about being able to enjoy the holiday.”
Collins stopped short of urging people to cancel holiday plans but said travel will be risky even for vaccinated people.
“This virus is going to be all around us,” he said. “I’m not going to say you shouldn’t travel, but you should do so very carefully. … People are going, ‘I’m so sick of hearing this,’ and I am, too. But the virus is not sick of us, and it is still out there looking for us, and we’ve got to double down on these things if we’re going to get through the next few months.”
Doctors, nurses and others are warning that the nation’s health system continues to be strained by an unending stream of coronavirus cases. Confirmed U.S. coronavirus infections have surpassed more than 128,000 per day and confirmed virus deaths are near 1,300 per day, according to The Washington Post’s rolling seven-day average.
“For people trained to save lives, this moment is frustrating, exhausting and heartbreaking,” the American Hospital Association, the American Medical Association and the American Nurses Association said in a joint statement on Friday, urging more Americans to get booster shots.
Public health experts are bracing for a winter surge of cases driven by the omicron variant, which can evade some protection conferred by vaccinations and prior infections, as well as cases linked to the delta variant. Officials caution that they are still relying on preliminary data about the omicron variant’s severity compared with earlier forms of the virus.
President Biden plans to address the nation Tuesday on the status of the country’s fight against the virus, the White House said Saturday.
“We are prepared for the rising case levels,” White House press secretary Jen Psaki wrote on Twitter, adding that Biden “will detail how we will respond to this challenge. He will remind Americans that they can protect themselves from severe illness from COVID-19 by getting vaccinated and getting their booster shot when they are eligible.”
The speech, coming just before Christmas and New Year’s Day, underlines Biden’s struggle to contain the pandemic nearly a year into office. On top of the emergence of new variants and attendant challenges, the administration has at times faced criticism for what some have described as mixed signals.
Biden won high marks from the public during the first half of the year as cases declined, the country opened up from shutdowns and vaccines became widely available. But the past few months have been more difficult. After he gave a speech on July 4 saying the country was “closer than ever to declaring our independence from a deadly virus,” the situation started changing. Case rates increased as the delta variant gained a foothold and many Americans refused to get vaccinated.
And despite Biden’s promise that at-home rapid tests would become a widely available tool to fight the coronavirus, the tests remain hard to find in many parts of the country and are more expensive than in some other places across the globe.
Fauci conceded Sunday that the administration needed to do better on increasing the availability of at-home coronavirus rapid tests, though he emphasized that the country was in a much better place than it was a year ago, with 200 million to 500 million tests available per month, many of them free.
“We’re going in the right direction,” he said on CNN. “We really need to flood the system with testing. We need to have tests available for anyone who wants them, particularly when we’re in a situation right now where people are going to be gathering.”
The omicron variant also has challenged the nation’s coronavirus medicine cabinet, with evidence that mutations will wipe out or weaken the effectiveness of treatments that can reduce the virus’s severity and keep people out of hospitals. As a result, the Biden administration around Thanksgiving paused distribution of sotrovimab, the one monoclonal antibody that remains effective against the omicron variant, with senior officials such as David Kessler calculating that the drug should be maximally deployed when the variant becomes more prevalent.
By Thursday, administration officials decided to resume shipments of the drug, amid indicators that the omicron variant was spreading faster in states such as New York and Washington than data published by the Centers for Disease Control and Preventionearlier in the week indicated, said two officials with knowledge of the deliberations.
“Shipment of product will begin soon, and jurisdictions will see product arrive as early as Tuesday, December 21, 2021,” the federal health agency said in a statement on Friday, announcing that about 55,000 doses of sotrovimab would soon go out.
Doctors said they were desperate for treatments like sotrovimab as emergency rooms begin to crowd and case numbers soar.
“Too slow! We are already seeing widespread omicron,” texted one infectious-disease doctor at a large New York City hospital, who estimated that at least 50 percent of patients had contracted the variant and requested confidentiality to discuss patient care. “It’s a lot of hospitalizations that could have potentially [been] averted because of slow response.”
Fauci said Sunday that he expected it to be months before antiviral drugs can be mass-produced and available to anyone who needs them. While he did not foresee the kind of shutdowns that were put in place in the early days of the pandemic, Fauci also noted that it would be difficult to keep the virus under control when there remained “about 50 million people in the country who are eligible to be vaccinated who are not vaccinated.”
Similarly, several governors on Sunday shied away from the possibility of implementing more shutdowns to fight the spread of the new variant. Maryland Gov. Larry Hogan (R) said on “Fox News Sunday” that his state, which has seen a 150 percent increase in hospitalizations over the past two weeks, was not considering shutdowns and instead was putting more resources into testing and encouraging vaccinations and boosters. New Jersey Gov. Phil Murphy (D) said on the same show that shutdowns remained “on the table” but that he didn’t think such a move was likely because a high percentage of the state’s population was vaccinated.
Colorado Gov. Jared Polis (D) emphasized that people in his state should keep themselves safe with “individual freedom and local control.” He also said Colorado officials were looking to change the definition of “fully vaccinated” to include three shots, as health officials in the country and around the world have signaled in recent days they are also considering.
“That’s certainly where it’s headed,” Polis said on NBC News’s “Meet the Press.” “I wish they’d stop talking about [the third shot] as a booster. It really is a three-dose vaccine.”