http://healthaffairs.org/blog/2017/08/31/data-driven-policy-making-in-an-age-of-anecdotes-what-happens-when-a-foundation-creates-a-policy-center/

Why would a health foundation create a public policy research center?
The Healing Trust, in Nashville, Tennessee, has funded a wide variety of health-related service and advocacy organizations in Middle Tennessee. But in 2014, we asked them what additional support we could give to these organizations engaged in policy and advocacy work. One priority quickly rose to the top: timely, high-quality, and nonpartisan research and analysis on public policy issues critical to our community.
Tennessee has several prominent academic institutions with respected researchers in this field, but an independent and nonpartisan public policy research center simply did not exist. We began to explore this idea, using research to vet different business models for similar centers in other states. Ultimately, we decided to incubate this new policy center inside our foundation before spinning it off into a separate and independent nonprofit organization.
Aiming to create a true community resource, The Healing Trust worked with the Nelson Andrews Leadership Center to engage eighty stakeholders in an intense, three-day, co-design process. A core group of participants then spent another three months hammering out the details. This collaborative process established community buy-in and developed the road map for everything from staffing needs and board composition to the policy center’s mission, name, and brand.
Inspired and encouraged by the community’s engagement, The Healing Trust board committed $2.5 million over five years as seed funding to launch the Sycamore Institute.
Lessons Learned Through Launching The Center
What has the foundation learned through launching the Sycamore Institute, and why should philanthropy think about supporting policy research?
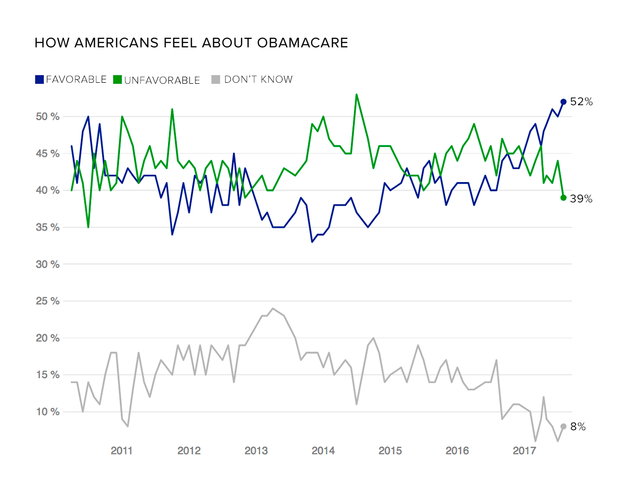
Ability to respond quickly in a rapidly changing policy environment: The Sycamore Institute has only been fully staffed for about six months—a period that includes one full legislative session in Tennessee and months of head-spinning debate in Congress over health reform. Yet, in that short time, our foundation’s investment has shown a solid return in the form of more than thirty reports, policy briefs, and blog posts about health policy and budget issues affecting Tennessee. As an independent public policy research center, the Sycamore Institute has the ability and agility to weigh in on rapidly evolving topics like how health reform efforts in Congress could affect our state.
Educating policy makers, the public, the media, and nonprofit partners: No matter where one stands on the political spectrum, we can all agree on the value of helping public officials make better-informed decisions. “Public Policy 101s” like how health insurance markets work and the nuts and bolts of Medicaid are just as important as analysis of specific legislation like the American Health Care Act. Our governor, administrative agencies, and legislators at the state and federal levels have already used the Sycamore Institute’s work to better understand key issues and communicate with their constituents.
These resources are equally valued by our foundation’s other grantees, who have become (1) even more knowledgeable about policy issues that affect their missions and (2) better equipped to engage with policy makers, the public, and other potential funders.
And in an era of shrinking newsrooms, the Sycamore Institute also provides important context and unbiased information to journalists covering health and fiscal policy. In very short order, the institute has become a trusted source for media outlets across Tennessee.
Unexpected Challenges
What were some of the unexpected challenges faced in launching a nonpartisan policy center?
Hiring the right leader: Hiring the right person to lead the Sycamore Institute proved more challenging than expected. The Healing Trust initially focused on candidates with backgrounds in policy research, but the collaborative design process we used shifted our focus to people with leadership experience who could launch a start-up and cultivate a diverse board. (Political, professional, geographic, and cultural diversity were all important criteria for the board.) Going back to the drawing board, our hiring committee interviewed new candidates and ultimately hired an experienced nonprofit executive director with an advanced degree in public policy.
Hiring the right staff: Building a staff with the ability to conduct high-quality research and analysis in-house and communicate about it to interested stakeholders was another challenge. Fully staffing the Sycamore Institute with an executive director, policy director, research analyst, and communications director took fourteen months—just in time to hit the ground running for the 2017 session of the Tennessee state legislature.
Recruiting a bipartisan board: To maximize and broaden the Sycamore Institute’s impact, the design shop showed we needed a bipartisan board committed to supporting nonpartisan work. The board’s balance of Republicans, Democrats, and political independents has been critical to building relationships with policy makers on both sides of the aisle. A balance of skill sets, diversity, and leadership potential is also key. With both the Sycamore Institute and its original board members based in the state capital, Nashville, recruiting additional board members from other regions of Tennessee remains a top priority.
Advocacy or analysis? Another question we wrestled with early on was where to draw the line. The primary goal of founding the Sycamore Institute was to fill a void of credible, independent, and nonpartisan analysis of policy issues in Tennessee. But should the organization go a step further to offer conclusions and recommend specific policies? Ultimately, the board and executive director decided that the Sycamore Institute would not advocate for specific policies, reasoning that doing so could hurt its credibility as a trustworthy source of politically neutral information.
Concluding Words
Building and maintaining health and well-being, which are complex issues, demand significant public and private resources. In Tennessee, as in most states, health care and education are the state’s top two budget priorities. The Sycamore Institute is dedicated to understanding and explaining the state budget and existing and proposed laws that affect the health and well-being of Tennesseans. Its information has already enabled citizens, policy makers, nonprofit agencies, foundations, media outlets, service providers, and others to understand better the fiscal and human impact of pending policies, giving stakeholders a nonpartisan and informed stake in the process and the outcomes.