Tag Archives: Leadership
The Three Types of Workplace Courage

COURAGE IS THE FIRST VIRTUE of organizational performance. Consider, for example, all the other concepts that courage connects to in workplace settings. Leadership takes courage because it requires making bold decisions that some people won’t agree with or support. Innovation takes courage because it requires creating ideas that are ground-breaking and tradition-defying; great ideas always start out as blasphemy! And sales always take courage because it requires knocking on the doors of prospects over and over in the face of rejection. These aspects of work simply can’t exist in the absence of courage.
That’s why it’s crucial to instill courage in those you lead, both in their development and training programs, but also by leading by example. There’s a lot you can do as a leader toward this end: rewarding jumping first, creating safety nets to make trying and failing a palatable option, teaching to harness fear, and modulating comfort levels are all management tools for setting a foundation that supports and encourages courageous behavior. But while courage in the abstract is an easy thing to get behind, in practice it’s more useful to break it down into different types of courage. Having a way of categorizing courageous behavior allows you to pinpoint the exact type of courage that each individual worker may be most in need of building.
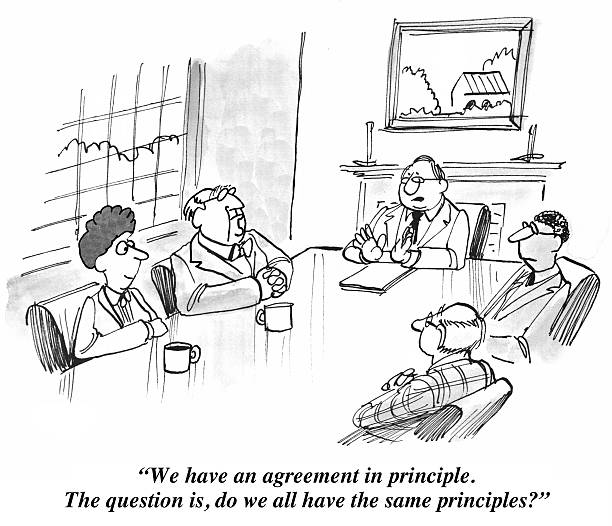
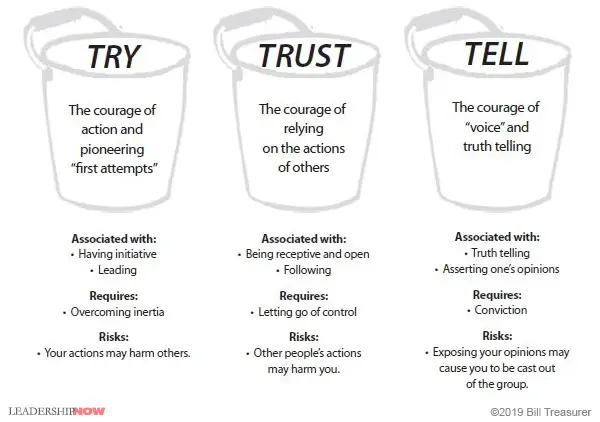
I think of courage as falling into three distinct buckets: TRY, TRUST, and TELL Courage. Let’s talk about each.
TRY Courage
The first bucket of courage is TRY Courage. TRY Courage is the courage of action. It is the courage of initiative. TRY Courage requires you to exert energy in order to overcome inertia. Certainly, it is easier not to do something than to do it, which is one reason why many people prefer to stay in their “comfort zones.” It takes courage to TRY something, particularly when you’ve not done it before. This is the kind of courage that’s demonstrated when someone “steps up to the plate,” for example, taking on a project on which others have failed. You experience your TRY Courage whenever you must attempt something for the very first time, as when you cross over a threshold that other people may have already crossed over.
The courage of try is associated with:
- “Stepping up to the plate,” such as volunteering for a leadership role.
- First attempts; for example, the first time you lead an important strategic initiative for the company.
- Pioneering efforts, such as leading an initiative that your organization has never done before.
- Taking action.
All courage buckets come with a risk, and the risk is what causes people to avoid behaving with courage. The risk associated with TRY Courage is that your courageous actions may harm you, and, perhaps more importantly, other people. If you act on the risk and wipe out, not only are you likely to be hurt, but you could also potentially harm those around you. It is the risk of harming yourself or others that most commonly causes people to avoid exercising their TRY Courage.
TRUST Courage
TRUST Courage involves resisting the temptation to control other people. Unlike TRY Courage, TRUST Courage is not about action. Instead it often involves inaction, or “letting go” of the need to control. With TRUST Courage, you step back and follow the lead of others. A common example of TRUST Courage is delegation. TRUST Courage is very hard for people who tend to be controlling and those who have been burned by trusting people in the past. TRUST Courage, though, is a crucial element in building strong bonds between people.
The courage of trust is associated with:
- Releasing control, such as delegating a task without hovering over the person to whom you’ve delegated.
- Following the lead of others, such as letting a direct report facilitate your meeting.
- Presuming positive intentions and giving team members the benefit of the doubt.
TRUST Courage, of course, comes with a risk. The risk associated with TRUST Courage isn’t that you will harm other people, but that by trusting them, they might harm you. By trusting others, you open yourself up to the possibility of your trust being misused. Thus, many people, especially those who have been betrayed in the past, find offering people trust very difficult. For them, entrusting others is an act of courage.
TELL Courage
The third bucket of courage is TELL Courage, which is the courage of voice. TELL Courage is what is needed to tell the truth, regardless of how difficult that truth may be for others to hear. It is the courage to not bite your tongue when you feel strongly about something. Brown-nosing and people pleasing are symptoms of low TELL Courage. TELL Courage requires independence of thought. We also use our TELL Courage when we take responsibility for a mistake or offer an apology. Whenever we speak up and say what’s hard to say, whether it be speaking truth to power, admitting a mistake, or saying “I’m sorry,” we are using TELL Courage.
The courage of TELL is associated with:
- Speaking up and asserting yourself when you feel strongly about an issue.
- Telling the truth, regardless of where the person to whom you are telling the truth resides in the organizational hierarchy, such as presenting an idea to your boss’s boss.
- Using constructive confrontation, such as providing difficult feedback to a peer, direct report, or boss.
- Admitting mistakes and saying, “I am sorry.”
TELL Courage can be scary and comes with risks too. We avoid using TELL Courage because we don’t want to offend others and fear being cast out of the group. The need for affiliation with those we work with is very strong, and the risk of TELL Courage is that, by speaking up and asserting ourselves, we will be cast out of the group and won’t “belong” anymore.
Courage is Contagious
Understanding (and influencing) courageous behavior requires that you be well versed in the different ways that people behave when their courage is activated. By acting in a way that demonstrates these different types of courage, and by fostering an environment that encourages them, you can make your company culture a courageous one where employees innovate and grow both personally and professionally. Here’s a handy diagram to remind you of these types of courage and what they require:
Solving the Decision Bottleneck In Two Essential (But Not So Easy) Steps

Imagine a single organization from the perspective of two different cultures: Culture Accountability and Culture Bottleneck.
In Culture A (Accountability), things get done quickly and efficiently. Executive teams are cohesive and managers know what is expected. As a result, managers run a tight ship and are quick to course-correct any activity, behavior or process that doesn’t align with the shared mission and vision. Managers are confident that their decisions will be supported by the executive team. Conversations, both vertical and horizontal, are focused on both process and people; results and relationships. Those who do not fit the culture leave on their own accord.
In Culture B (Bottleneck), bottlenecks create frustration. Decisions seem to be an afterthought and lack of trust precedes the need to micromanage. Managers fear making decisions because their decisions are often overridden. Executives complain that their managers never get the job done. On the front lines, turf wars and internal drama erupt spontaneously. Uncertainty, unexpected change and chaos color the culture. Conversations are avoided and poor performance is justified until something major happens and firing is the only option.
“At most organizations, the bottleneck is at the top of the bottle.”– Peter Drucker
All other things considered, there are two components that distinguish Culture A from Culture B: Clarity and Communication.
1. Clarity: How and who makes decisions
In every single instance of time-wasting drama, no matter how it manifests, at the root is a lack of clarity in some form.
On the front lines, when employees are unclear about what success looks like, they lose confidence and waste productive hours getting reassurance and clarification — procrastinating when uncertain. At the highest level, lack of clarity about the real problem or the desired end result wastes time and resources hiring vendors and consultants offering “one and done” workshops or other ineffective solutions.
Even when there is clarity about the real problem, the end result and the process, a big road-block I often see is the lack of clarity about who is in charge and how decisions are made.
For context, let me share a quick example. Years ago I was on a project for a mid-sized corporation. My inside contact, a high-level director, had absolutely no power to push the project forward. Because of this fact, any work I did had to be approved by the top executive who would continuously change calendar dates and, in doing so, would “delegate” the date changing to the director, who had to navigate calendars and multiple dates. I estimate we wasted at least 40 productive hours chasing down the real decision maker to make a change instead of setting up one phone call.
Increasing clarity inevitably increases your productivity and speed. Here are some suggestions for increasing speed by increasing decision-making clarity.
What to start doing
- After identifying the real problem and the desired outcome, take the necessary time to agree on how decisions will be made among top executives. Whether you are a co-owner or a team of C-suite executives, your organization’s success and your peace of mind is dependent upon your maturity to clarify your decision-making processes.
- Have a plan in place to maximize efficiency and decision making for those times when change happens.
- Give real decision-making authority to those to whom you delegate power.
What to stop doing
- Stop going rogue on your senior partners. Before you make a major decision, get alignment from your executive team.
- Stop delegating when delegation creates a bottleneck. Instead, hire an assistant to do the grunt work and let your director-level people get their own work done.
- Stop complaining about your employees and team members. If you find yourself complaining, set a time on the calendar to confront the issue with the person (or people) who needs to hear the conversation.
2. Communicate: Initiate clear conversations
The number-one problem I see that slows progress and efficiency is the inability or unwillingness of leaders to initiate what I call executive conversations. Executive conversations (as I define them) are both results- and relationship-oriented.
Many drama-laden cultures adopt an either-or mentality: a mindset that it’s all about results — anything for a profit, or it’s all about relationships — avoiding conflict at all costs. Both mindsets create accountability-related issues.
In his bestselling book, Advantage, Patrick Lencioni says:
“Many leaders struggle with accountability but don’t know it. Some will tell me that since they aren’t afraid to fire people, they must not have an accountability problem. Of course, this is misguided. Firing someone is not necessarily a sign of accountability, but is often the last act of cowardice for a leader who doesn’t know how or isn’t willing to hold people accountable. At its core, accountability is about having the courage to confront someone about their deficiencies and then to stand in the moment and deal with their reaction which may not be pleasant.“
When there is a lack of accountability there is a lack of alignment, and when there’s a lack of alignment there’s a need for executive conversations.
What to start doing
- Increase your awareness of what is happening that should not be happening, and articulate it.
- Ask for the behavior or action you want directly and succinctly without blame.
- Keep the overall good of the organization in mind when you address the issue.
- State how the problem you perceive affects the revenues, productivity, team, client satisfaction or any other business case.
What to stop doing
- Stop holding grudges and realize that a grudge is a sure sign of a conversation that needs to happen.
- Get coaching support to learn how to initiate conversations that get results instead of resentment.
- Stop firing people before you’ve had the courage to have a couple of conversations. If you communicate effectively, they will either improve with some coaching, or they will eliminate themselves when they see they can’t cut the mustard. The good news is they will probably leave on friendly terms.
Conclusion
There are many factors that shape culture; however, it’s up to the senior leaders to eliminate the time-wasting bottlenecks that contribute to high-drama cultures. Get clear on the real problem and the desired end result. Clarify who is in charge and how decisions are made. Initiate executive conversations that are both relationship- and results-oriented to transform the Bottleneck Culture into a Culture of Accountability.
Five Components of a Thought Leadership Strategy
https://www.thinkrevivehealth.com/blog/five-components-thought-leadership-strategy
The role of a thought leader is to offer unique insight on a specific topic, problem, or trend and establish themselves as a go-to resource. A successful thought leadership strategy supports organizational business goals, making it an essential part of any communication plan. You shouldn’t have to look hard to find a thought leader in your organization—they typically are the individuals in your C-suite, but there are likely others equally as valuable in your organization with ideas, passion, and experience that may be credible thought leaders.
Thought leadership can take many forms, such as contributed content, speaking engagements, webinars, white papers, and an ongoing social media presence. It is imperative to remember that, like all communication efforts, strategy should drive thought leadership and consistency is critical. Having a clear strategy tied to your business goals will help establish your voice, get buy-in from leadership, and allow for effective measurement of your program.
The best way to start is by identifying topics your thought leaders can speak to that will support your organization’s goals. For example, if you are a health IT vendor that wants to increase sales of your population health tools, focus on promoting your organization’s point of view (POV) on effective population health management.
Below are five components to consider incorporating in your thought leadership strategy.
1. Proactive outreach
Recently, members of ReviveHealth’s public relations team attended July’s Nashville Public Relations Society of America luncheon featuring presenter Johnny Smith Jr., senior director of public relations at Ascension. A fellow attendee asked about why proactive public relations is important to thought leadership. His response?
“PR is a tackle sport.”
The first step of proactive PR is engaging in daily media monitoring and other environmental scanning techniques to determine what topics are trending in your industry. Then, join the conversation via social media, contributed articles, etc., sharing your organization’s point of view. But remember: be strategic and specific about the topics your expert can speak to and make sure they are relevant to your business and the industry. See also: Managing the Race Against a Bad Reputation
Another tip from Smith, Jr.: it’s imperative to establish and maintain relationships with media, which lowers the barrier to entry when joining the conversation. A key part of this is setting up face-to-face meetings between thought leaders and reporters whenever possible—these often prove more valuable than a phone call or email. These conversations are opportunities to share a POV and establish credibility as source for reporters.
2. Local involvement
Securing coverage in trade and national consumer publications might be the goal, but having a presence in local media is foundational to any thought leadership strategy. This way, when you approach trade and national publications with your company’s story, you’ll already have an established presence as a thought leader on the subject on the local level. This could mean contributing content, writing a monthly column or being mentioned in an industry story.
Local media is also a chance for you to get creative as a PR professional. Is there a cause your thought leaders are passionate about they can advocate for locally? If you have a thought leader that’s making waves in the industry, what local award nominations are a good fit? These activities in the community will help lead to organic media coverage locally and beyond.
3. Speaking engagements
Securing speaking engagements are a tried-and-true practice when it comes to elevating the thought leaders in your organization. These opportunities get you in front of your audience and allow you to engage with them directly. Research opportunities for your thought leaders to give keynote speeches and participate in panel discussions or Q&As at industry conferences as part of your proactive PR activities.
Pro tip: the best way for vendors to showcase your business’ innovative solutions is to partner with one of your clients and share their success story. It’s a win-win for both parties. Check out this blog to learn more about The Power of the Proposal.
4. Content creation
In addition to earned media coverage, take advantage of blogging, op-eds, contributed content, webinars, and white papers. Developing a variety of content allows you to continually engage with your audience at different stages of the buyer’s journey while generating interest about a topic.
Make sure your content links to other (relevant) previously-developed thought leadership materials – such as white papers you’ve created and recordings of webinars – on your website.
5. Social media
Social media is another avenue for creating content and sharing your POV. Speaking at an event? Tell your organization’s followers and live tweet the presentation. Hosting a webinar? Invite your target audience to attend by setting up a Facebook event. Just released a new white paper discussing the current industry trends? Have the paper’s author publish a short blog about the content on his or her personal LinkedIn page.
Social media is also the place to share relevant industry articles and news that, while may not quote your thought leader specifically, still supports your thought leadership strategy. Remember, use the 80/20 rule on social media. Roughly 80 percent of the content you post should be non-branded industry content, while 20 percent should promote your organization.
A thought leadership strategy is critical to elevating your organization in the public sphere, and therefore helping achieve business goals. To maximize success, be strategic and consistent through proactive activities with your audience such as speaking engagements, content sharing, online communication and local advocacy.
Cartoon – Moving to a Shared Leadership Model
7 Cardinal Rules for Life

Integrity Matters Most in a Leader!
https://www.linkedin.com/pulse/integrity-matters-most-leader-brigette-hyacinth/
In every aspect of our lives we depend on the integrity of others, and others do the same with us. That’s why it’s such a big deal when we discover someone we trust hasn’t been truthful or hasn’t been playing by the rules.
Although integrity is one of the most essential and admired leadership traits, in today’s world it seems to be lacking. What you see in leaders is not often what you get.
Here are 7 masks some leaders wear:
1. Orator (The Two Face mask) – Double tongued are they. They can sound so persuasive and so sincere. Fervent lips which sound so eloquent can hide true character. Behind the dazzling mask lies their real intentions of deception. Erroneous communications are a big cause of lack of perceived trustworthiness in bosses. Politicians are notorious and highly populate this category. However, their actions always expose them. We don’t take them at face value because we don’t know which face they have on.
2. Advocate (The 3 Musketeers mask)- “One for all and one for one.” They are all for me, myself and I. The love of power is their main motivator. They outwardly proclaim they are people focused, and their priority is with the team but behind closed doors they are self- seeking. Therefore when the opportunity is presented to prove it they cannot. They will do anything to make themselves look good, or maintain their status quo even at the expense of the team.
3. Philanthropist (The Robin Hood mask) – They give with the right hand but secretly take back with the left hand. Under this disguise these type of leaders give openly so others can think highly of them. If there was no fanfare they would not support charitable initiatives. Former Tyco International Ltd. Chairman Dennis Kozlowski improperly used company funds to promote himself as a generous benefactor. He committed more than $100 million of the conglomerate’s money to good causes however, his own foundation gave little to charity. He was accused of stealing $134 million from the company and served 8 years in prison.
4. Obdurate (The Iron Man mask) – They scarcely show their true feelings or human side. They think they need to have this public tough image. Marissa Mayer, former CEO of Yahoo came across as cold and disconnected to her employees. Her policies (maternity leave and long-term telecommuting) caused outrage. Adopting this persona alienates and pushes people away. By not showing any vulnerability, such leaders do not develop deep meaningful connections or build relationships with their team.
5. Meek (The Mister Fantastic mask) – They appear so humble and act down to earth when in fact they have an entitlement and superiority complex. However, their true colors are revealed in unguarded moments. I remember once working late and overhearing a manager speaking with a supervisor. He didn’t realize I was there and openly spoke to her. As I sat there I couldn’t believe that this is the person I thought I knew. When he came out of his office and saw me by my desk, he seemed really disoriented and shocked and asked if I had overheard him. Well, my whole perception of him changed from that day.
6. Proficient – (The Phantom of the Opera mask) – Some leaders conceal imperfections in favor of a polished image. The demands or expectations that society creates leaves them feeling mediocre and inadequate. They are uncomfortable in their own skin so they try to measure up and may even employ unethical methods to fit in. Lying on his resume cost former Bausch & Lomb CEO Ronald Zarrella $1.1 million in bonus after it was revealed he did not have an MBA as recorded. Company officials declined to accept his resignation. He remained in his role for another six years before retiring in 2008. Ironically, he probably didn’t need that degree. His prior job experiences were almost certainly enough. Still, like so many people, he seemed to have yearned for a status symbol.
7. Conformist – (The Shape-Shifter mask) – In this case, top management puts pressure on these types of managers to change their principles. Their style may not fit in with the changing culture. There is a shift between their preferred style of behavior and what the company wants. They play it safe to preserve their position and privileges. They just follow orders and exude no loyalty to employees. It’s demotivating working for a manager who does not stand up for their team. If you make a mistake they quickly turn into judge, jury and executioner. It’s hard to feel passion for a job when you experience this.
In the era of social media, where leaders’ personal and professional lives are often transparently intertwined, the mask eventually becomes apparent. Trust once lost is often hard to regain. Integrity requires humble introspection.
It requires you do what is right – not what is easy. Our actions must mirror our words in all facets of life. It all starts with keeping your word, making fair decisions, communicating honestly, taking responsibility, treating others with dignity and respect and giving credit where it’s due. There are many things you can lack and still steer clear of danger. Integrity isn’t one of them. If you don’t have integrity, people will not trust, believe or follow you. If you don’t have integrity, you have nothing.
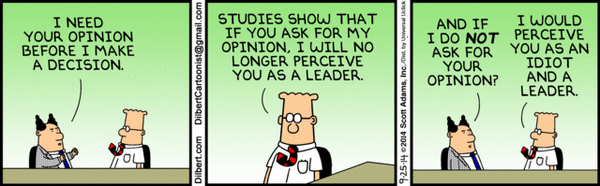
Cartoon – I Need Your Opinion
Cartoon – Trying Not to Lead by Example
16 Rules for Effective Decision-Making
https://www.leadershipnow.com/leadingblog/2019/04/16_rules_for_effective_decisio.html
WHERE WE GO in life is determined by the choices we make. How we make those decisions becomes critical. The speed of change, the abundance of choices, the unknown unknowns, and the impact of a connected world, all conspire to make decision-making a labyrinth. We face traps everywhere.
In Labyrinth: The Art of Decision-Making, Pawel Motyl examines “The most prevalent weak spots in decision-making processes, not only in business but in life in general; during crisis and calmer times; in both individual and group decisions.”
I agree with Motyl that “We really do live in a world where everything is out of whack and everything we thought we knew is being called into question.” It calls for a deeper look at not just what we think, but more importantly how we think and a clear understanding of how we got there.
Motyl digs into the series of decisions that led to some of the modern world’s most dramatic events: from the Cuban missile crisis to the 1996 Mount Everest climbing disaster; from the Apollo 13 rescue mission to the ill-fated Daimler–Chrysler merger.
Using many and varied examples Motyl reveals 16 rules for effective decision-making. The rules with the accompanying narrative are well-researched and intriguing. Here is the overview:
Rule #1
Prepare for a black swan (an unpleasant surprise or event that we cannot predict from prior experience), because one thing is certain: sooner or later you will meet one. Because of easy access to information and globalization, black swan events are on the rise.
Rule #2
The better it’s going, and the more successful you are, the more you are at risk of turkey syndrome. The deeper you fall into turkey syndrome, the nastier your black swan will be.
Rule #3
The more you admire someone, the more critically you should examine their opinions. The more exciting somebody’s vision seems, the more closely you should test its foundations in reality. This fundamental misunderstanding comes into play here: “a harmonious group = a tight group = an effective group”
Rule #4
The more everyone around insists something is impossible, the more you should check it yourself. Several times.
Rule #5
The greater the investment of time, effort, money, and our own reputation, the harder it is to objectively assess a situation and make the right decision.
Rule #6
If you find yourself in a black swan situation, go into inquiry mode. Whatever your intuition or experience is telling you may be wrong.
Rule #7
Set up your own Executive Committee. Surround yourself with people who don’t think like you. Value those who disagree with you, and who aren’t afraid to say it.
Rule #8
When improving and organization, also pay attention to the best and most efficient processes. In a black swan situation, they can fail. Do you have a backup plan?
Rule #9
Shoot down Concordes and hunt for monkey habits. Eliminating loss-making projects and bad practices frees up time for other things, increasing a company’s agility and flexibility.
Rule #10
Recognize the value of your failures (and those of others). Thoroughly analyze your past failures and draw in depth, objective, and actionable conclusions for the failure.
Rule #11
Never stop shaping the organizational culture. It can be your greatest ally, or your worst enemy, in making the right decisions.
Rule #12
Great leaders are distinguished by their awareness that greatness is no guarantee of infallibility.
Rule #13
Don’t be a “decision drunk”—use data for illumination, not only for support. Data can be a great ally, when properly analyzed.
Rule #14
Never ignore the values and convictions of other generations, especially those only just entering the market. Even if their influence on decision-making today is minimal, the new normal means this may change sooner than you expect.
Rule #15
The world of data overload is also a word of new possibilities. Actively seek out opportunities to engage a cost-free force that can radically improve the quality of your decision-making.
Rule #16
Encourage and create leaders around you. Dispersed leadership involves many people, which means there is less risk of a single person making a poor strategic choice.