https://www.axios.com/2025/10/30/trump-immigration-elder-care
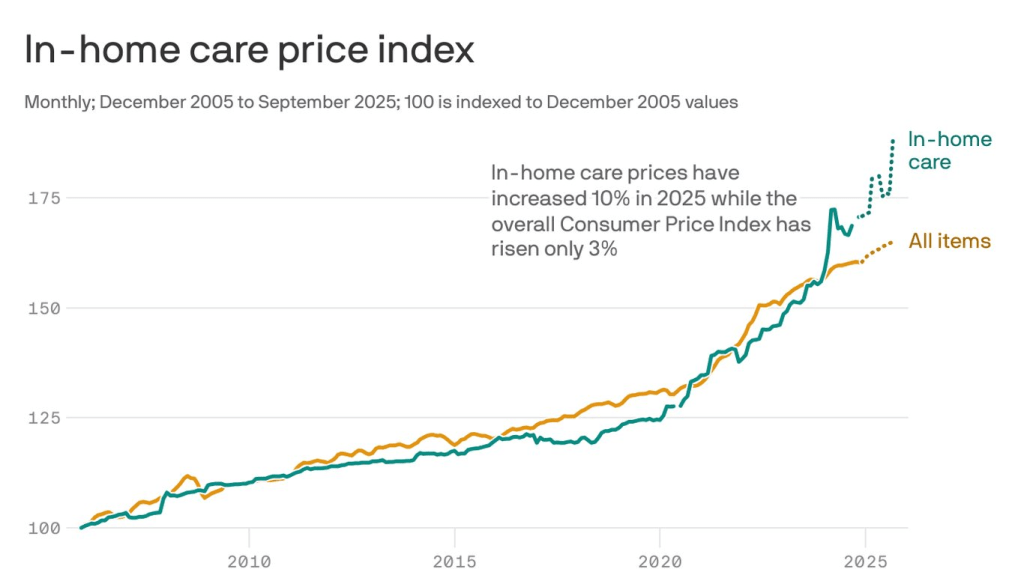
The cost of hiring help to care for an elderly or a sick person at home is skyrocketing.
Why it matters:
A labor shortage and surging demand from an aging population was already driving up prices, and now the White House’s crackdown on immigration and funding cuts are making things worse.
By the numbers:
So far this year, the price of in-home care for the elderly, disabled or convalescent at home is up 10%, compared with a rise of 3% for prices overall, according to government data.
- From just August to September, prices for home health care spiked a staggering 7%.
Zoom in:
Rising prices and the limited availability of people who do this work are pushing families to make hard choices. Some will put relatives and loved ones into institutions, a more expensive and often less desirable option than staying at home.
- Others will drop out of the workforce or cut back their hours to care for parents, relatives or partners.
- The supply of workers is not keeping up with demand, Matthew Nestler, senior economist at KPMG, writes in a post. “That hurts workers and their families, employers and the overall U.S. economy.”
Friction point:
Last year, employment was surging in home health care, with an average of 13,500 jobs added each month.
- But after the Trump administration immigration crackdown began in January, employment dropped off, falling into negative territory for three consecutive months in the spring, Nestler noted this summer.
- This isn’t a matter of demand falling, but a cutoff in supply, he explained.
How it works:
Immigrants make up 1 in 3 workers in home care settings, per data from KFF, a health care research organization.
- The severe crackdown this year on undocumented immigrants and the Trump administration’s removal of legal status from workers who are here from Venezuela and other countries are making it hard to find workers, says Mollie Gurian, vice president of policy and government affairs at LeadingAge, an aging-services nonprofit.
- “The supply of workers was already so low,” she says. With fewer folks available, the companies that provide these service are raising prices to put pressure on demand. Others are raising prices in anticipation of cuts to Medicaid funding, she says.
The big picture:
At the same time that the supply of people to do this work is falling, the number of Americans who need care is rising, as a silver tsunami of baby boomers ages.
The bottom line:
We are only at the very beginning of a dramatic demographic shift, Nestler says.
- Elder care is a “ticking time bomb that no one’s talking about.”