Tag Archives: Pharmaceutical Industry
USA Today editorial board: Amazon, Berkshire Hathaway, JPMorgan can’t ‘fix our nonsensical health care system’
While health insurers and benefit managers saw stocks tumble on news Amazon, Berkshire Hathaway and JPMorgan Chase & Co. will enter the healthcare arena, the editorial board at USA Today isn’t convinced the move will be as disruptive as some think.
In an opinion piece published Feb. 20, USA Today editors wrote, “To BBD [Jeff Bezos, Warren Buffett and Jamie Dimon] we say: Go for it. If you can come up with ways to provide your employees with better health care for less money, more power to you. To the rest of the country we would say this: Don’t get too excited. Not even a company as crafty as Amazon, or a bot as all-knowing as Alexa, can fix our nonsensical health care system.”
USA Today said the reason an Amazon-Berkshire-JPMorgan company won’t create overarching change is because U.S. healthcare is built upon an “upside-down” architecture. They wrote providers and drug companies “have monopoly or near-monopoly powers” to set prices, while employers and payers are much more fragmented.
“The three companies — particularly Amazon — are known for their ability to disrupt industries. But in health care, they aren’t up against an old-school industry fallen behind the times; they’re facing powerful monopolies or near-monopolies brimming with technology of their own,” according to the report.
To view the full opinion piece, click here.
Monopoly Medicine: How Big Pharma Stops Its Competitors and Monopolizes the Health Industry
After Another Merger Monday In Health Care, CVS Is Still The Company To Watch In 2018

The health care sector rallied yesterday on another “Merger Monday” with the announcement of Sanofi’s (SNY) purchase of Bioverativ (BIVV) for $11.6 billion, and Celgene’s (CELG) $9 billion purchase of 90 percent of Juno Therapeutics (JUNO). But there’s still one transformative merger that will define and reshape the U.S. health care market in 2018: the CVS/AETNA $69 billion deal announced last December.
CVS is best known for its 9,700 retail pharmacies and 1,100 walk-in clinics, but its most significant profit driver is its pharmacy benefits manager (PBM) enterprise—a middleman between pharmaceutical manufacturers and dispensers like drugstores. The company generated $177.5 billion in net revenue in 2016.
With its purchase of Aetna, another bold company and the nation’s third largest health plan, CVS upended uncomfortable business incentives built into its business model. In theory at least, the CVS PBM has new incentive to bring down drug prices and push for the most efficacious—not necessarily the most expensive—treatment choices, to achieve more competitive insurance premiums. They can also favor common sense preventive and primary care through convenience clinics.
This is what makes the CVS/Aetna deal different. It crosses sectors and realigns previously competing business incentives to better target consumer demand. Most of the merger proliferation we have seen over the past few years involves companies in similar categories within the health care industry. Providers merge with other providers, health plans with other health plans, and pharmaceutical companies with others in pharma.
Realigning incentives is the central problem in the health care marketplace, which is built on thorny knots of unintended consequences and senseless rules that resist untangling. The most famous of those knots are fee-for-service payment rules, still largely dominant, whereby payors reimburse for any and all services, regardless of quality. Among its hazards, fee-for-service incentivizes infections because it results in more care and thus pay better. Nobody thinks that is a good idea, but the business model is extremely difficult to unravel. CVS seems up to the challenge.
CVS Chief Executive, Larry J. Merlo, is the man for the job. His signature style is a laser-focus on the company’s core mission of “helping people on their path to better health,” which he is determined to accomplish even when short-term profit incentives nudge in a different direction. That was why Merlo led CVS to discontinue tobacco sales in 2014, and why CVS recently banned digitally altered photos on cosmetic products sold in their stores. Maybe it sounds logical that a health enterprise shouldn’t sell cigarettes or promote eating disorders and depression, but it takes unusual courage to turn away lucrative business.
Many greeted the news of the CVS/Aetna merger as a play to head off new ventures coming from Amazon or other new players. But what makes me optimistic about this particular deal is the new company’s combination of health industry and retail savvy. Many companies have one but not the other. Enterprising outsiders often enter the health care industry with good backing and an idea that would definitely help patients, only to end up six feet under the health care lobbyists, special interests, regulatory twists, and perverse incentives that have dogged the health care system over decades. There are large graveyards full of great companies that naively believed that normal business models work in health care. CVS is not naïve.
Cartoon – State of the Pharmaceutical Industry

Cartoon – Where does that leave us?

The health care industry’s bubble
Health care companies at this year’s J.P. Morgan Healthcare Conference celebrated the Republican tax overhaul and trumpeted optimistic views of their future financial power. But as more Americans become unable to afford drug prices, hospital bills, deductibles and copays — and as they voice their anger — there is sentiment brewing in the industry that a day of reckoning will come.
Key quote: “We are in the middle of a bubble in all health care asset classes,” said Bijan Salehizadeh, a health care investor at NaviMed Capital. “Everyone knows it, but no one knows how it will end.”
DOJ recovers $2.4B in healthcare fraud cases: 4 things to know

The Department of Justice obtained $2.4 billion in fraud and false claims settlements and judgments in fiscal year 2017, marking the eighth consecutive year recoveries in the healthcare sector exceeded $2 billion.
Here are four things to know about the DOJ’s false claims and fraud recoveries.
1. The DOJ recovered more than $900 million from the drug and medical device industry in fiscal year 2017. That total includes Shire Pharmaceuticals’ $350 million settlement. The settlement resolved allegations Shire, a multinational pharmaceutical company with its U.S. headquarters in Lexington, Mass., and one of its subsidiaries paid kickbacks and used other unlawful means to induce physicians and clinics to use or overuse Dermagraft, a bioengineered human skin substitute approved by the Food and Drug Administration for the treatment of diabetic foot ulcers. The settlement was the largest False Claims Act recovery by the federal government in a kickback case involving a medical device.
2. The DOJ also reported substantial recoveries from healthcare providers, including Cleveland, Tenn.-based Life Care Centers of America, which agreed to pay $145 million to settle allegations it caused skilled nursing facilities to submit fraudulent claims to Medicare for unnecessary rehabilitation services.
3. In another substantial settlement this year, Westborough, Mass.-based eClinicalWorks, an EHR vendor, and some of its executives and employees agreed to pay $155 million to resolve false claims allegations. The government alleged eClinicalWorks falsely obtained certification for its EHR software by withholding information from its certifying entity. Due to eClinicalWorks’ alleged misrepresentations, healthcare organizations using the company’s software submitted false claims for federal incentive payments, according to the DOJ.
4. In 2017, the DOJ continued to pursue physicians and healthcare executives involved in fraud cases to hold them personally responsible. For example, in 2015, Fort Myers, Fla.-based 21st Century Oncology paid $19.75 million to settle allegations it violated the False Claims Act by billing for medically unnecessary laboratory urine tests and paid bonuses to physicians based on the number of tests they referred to its laboratory. This year, the DOJ secured separate settlements with various urologists who allegedly referred unnecessary tests to one of 21st Century Oncology’s labs.
Cartoon – Pharmaceutical Industry Today

Pharma’s big quarter
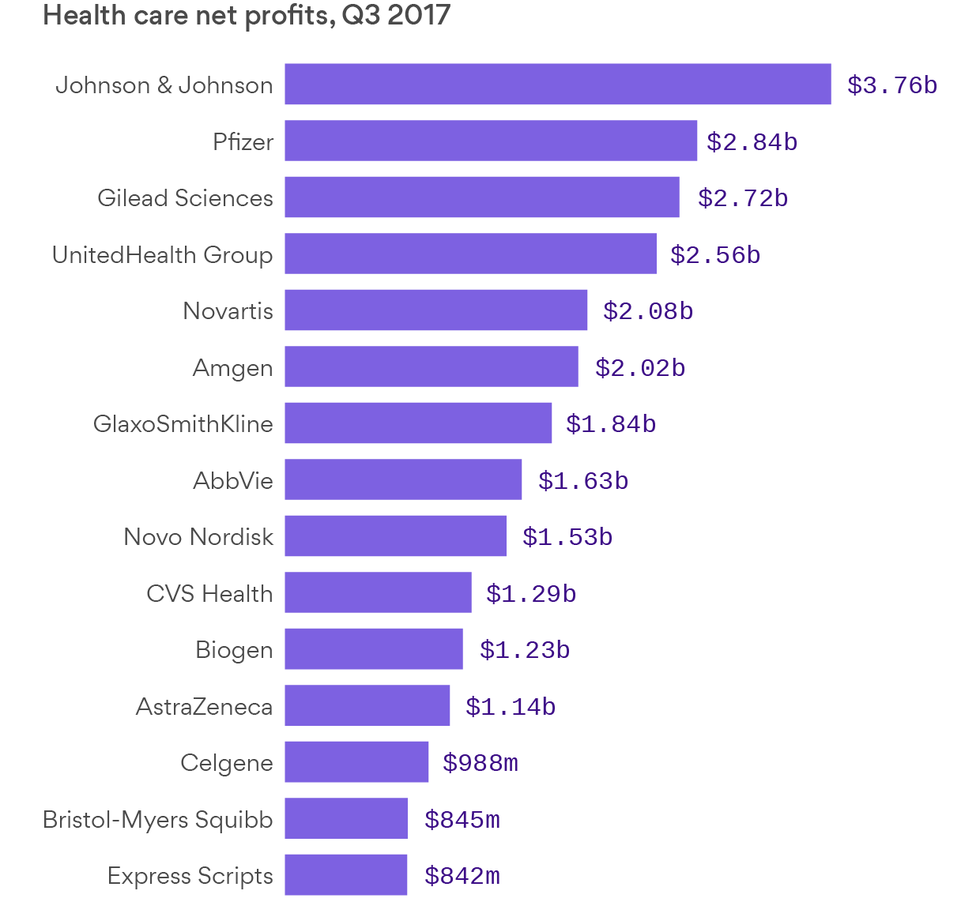
Data: SEC filings; Chart: Andrew Witherspoon / Axios
Axios’ Bob Herman has been tracking the health care industry’s financials over the third quarter, in which the 99 largest publicly traded health care companies cumulatively collected $33 billion of profit and $577 billion of revenue worldwide.
Winners: Pharmaceutical companies collected more than 60% of those profits, but only 22% of the revenue.
- No health care company netted more profits than Johnson & Johnson, the behemoth maker of drugs, medical devices and consumer products like Band-Aids and Tylenol. Its net profit was $3.8 billion in the quarter.
- 8 of the 15 highest net profit margins were at drug companies.
- 12 of the 15 highest net profit totals were at drug companies.




