Category Archives: Leadership
Cartoon – Changing Company DNA
Cartoon – Totally Different Goals
Cartoon – Becoming Change Masters
The sudden strategic importance of the CNO
https://mailchi.mp/f12ce6f07b28/the-weekly-gist-november-10-2023?e=d1e747d2d8
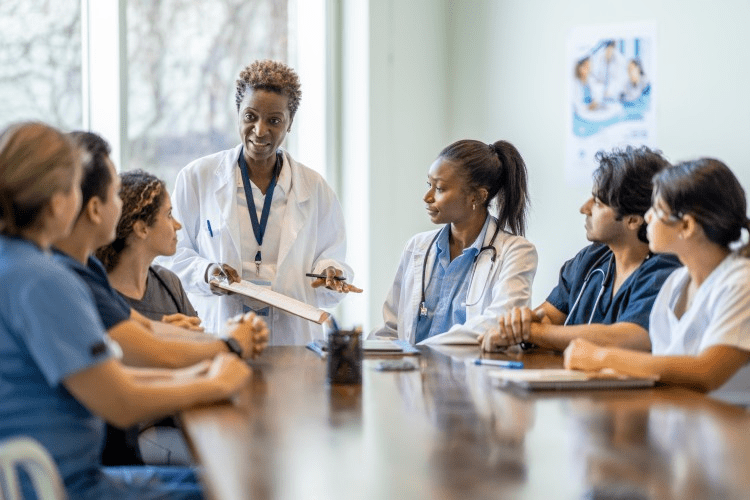
One welcome side effect of the current economic challenges health systems face has been the return to prominence of the chief nursing officer (CNO) as a pivotal driver of system strategy.
So many of a hospital’s important operating and margin pressures intersect with the CNO’s domain: staffing shortages, nurse recruiting and retention, workplace violence, rising union activity, care model redesign, adoption of new care technologies (including AI), the shift of the clinical workforce into non-hospital settings, and on and on.
Never has the role of the CNO been more important to ensuring systems’ continued ability to deliver high-quality, cost-effective care in a sustainable way.
Even more heartening, we’ve been part of a number of system board retreats and strategy discussions over the past several months at which the CNO has been an important voice in the room.
We’d argue that, given how important these issues will be over the coming years, it may be time to give CNOs a permanent role in health system governance, just as boards often include physician members.
One additional agenda item that will be critical for systems to address, given the demographics of nursing executives:
what’s being done to cultivate the next generation of strong nursing leadership to fill the CNO role? A topic worth keeping an eye on.
Cartoon – Time to Restructure
Cartoon – The Coffee has No Filter
‘Streamlining’ efforts reach the CEO
Health systems are increasingly focused on their regional structures, reorganizing leadership to provide oversight most effectively. On Oct. 23, those changes hit the corner office.
Providence is phasing out the CEO role at two of its California hospitals, the Renton, Wash.-based system confirmed to Becker’s. One year ago, Providence’s Northern and Southern California regions came together to create a sole South Division. Now, a single chief executive — Garry Olney, DNP, RN — will oversee operations in the Northern California service area, replacing the CEOs of Napa-based Queen of the Valley Medical Center and Santa Rosa (Calif.) Memorial Hospital.
“This was part of a systemwide restructuring to streamline executive roles so we could preserve more resources for front-line caregivers and become nimbler and more responsive to the times,” the system said in a statement.
Providence isn’t alone in its desire to streamline leadership. Corewell Health East — part of Corewell Health, which has dual headquarters in Grand Rapids and Southfield, Mich. — made seven executive changes within the region, the system confirmed to Becker’s on Oct. 23. The senior vice president of medical group operations was let go, along with two hospital presidents. The region’s COO of acute and post-acute care, Nancy Susick, RN, will take over one hospital in addition to her current duties; the second hospital will be overseen in a dual capacity by Derk Pronger, who already helms another hospital in the region.
The word “streamline” was also used by Chicago-based CommonSpirit, which recently shared plans to lighten its regional load.
“We are also making further changes to streamline the organization, including the consolidation of our operating divisions into five regions from eight, clearly define our market-based focus and strategies and continue to refine our operating model,” CFO Dan Morissette said on an Oct. 12 investor call.
Regional revamps don’t always lead to cuts or “consolidation.” In some cases, they lead to the creation of new roles. Atlanta-based Emory Healthcare recently split its 10 hospitals into two divisions — one for regional hospitals, one for university hospitals — and tapped a president to helm each. Plus, Tampa (Fla.) General Hospital named eight new executives in a C-suite overhaul following the adoption of three Bravera Health hospitals into TGH North.
If the healthcare leaders plan to confront looming challenges, they need to be comfortable with “innovating and disrupting [themselves],” John Couris, president and CEO of Tampa General, told Becker’s.
“The way I would describe this is the last five years was all about foundational work,” Mr. Couris said. “The next five years and beyond is all about transformational work. So we’re shifting from the foundational activity to the transformational activity, and we need an organizational structure and a leadership team that reflects that journey. That’s why we made the changes.”
Thought of the Day: On Life’s Writing
Listening and Learning

Something I have been writing about and speaking about recently is how difficult it is to operate a hospital in post-Covid America.
The line-up of management and governing obstacles includes both old and new healthcare issues:
- Financial instability
- Ongoing labor disruption
- Remnants of significant healthcare inflation
- Payer chaos
- A continuing pivot from inpatient to outpatient services
- The endless introduction of alternative care options (CVS, Walgreens, Walmart, Amazon, and now Costco)
It takes considerable hard thinking within executive suites to figure out the best way forward; to find the best roadmap through—at a minimum—the six obstacles outlined above. And as I have noted in my recent speaking engagements, a solution to one of these obstacles might actually make others of these obstacles more difficult to solve.
I have in recent weeks been looking for a “thought platform” that can assist hospital C-suite executives in resetting managerial expectations and operational initiatives—expectations and initiatives that can more effectively cope with the current and distressingly difficult environment.
Moving the hospital organizational thought platform from its 2019 managerial themes to a more relevant platform that better suits the challenges of 2023 is a managerial problem all of its own. Simply telling a large and very complex healthcare organization to stop thinking in pre-Covid terms is not likely to accomplish much. Before you can establish the organizational thought platform that best guides your hospital forward, you will need a leadership team that is committed to creating a “listening and learning” healthcare company.
A good tool for making your way to a listening and learning organization and eventually to a new and more relevant thought platform is the book The First 90 Days: Proven Strategies for Getting Up to Speed Faster and Smarter, by Michael D. Watkins.
Mr. Watkins is a co-founder of Genesis Advisers and a professor at the IMD Business School in Lausanne, Switzerland. The First 90 Days was originally published in 2003 as a guide to business executives moving into new senior positions of major responsibility. But the book also contains general management advice which is relevant not only to new jobs, but also to executives struggling with fast-changing and especially difficult market conditions.
One of the most compelling chapters in The First 90 Days is a chapter that focuses on the absolute importance of executive learning and the need to accelerate that learning.
While Professor Watkins was making a general business point, I would suggest that the need to accelerate executive learning and listening was never more important than in the “right now” post-Covid healthcare environment. Professor Watkins posed a series of critical leadership learning questions that I have modified to reflect the complex operating conditions of the 2023 hospital.
From that perspective, here are six critical learning questions for the hospital leadership team:
- How effective are you as a hospital leader at learning about your current job and how that current job is changing?
- What is your learning agenda for your current assignment? Have your day-to-day responsibilities changed so dramatically that you no longer know what you need to know?
- Given questions one and two, how should you go about gaining better insight?
- What is the best structure for being a top-flight learner within your organization? Note that this is a question that has both individual and organizational implications.
- What support is there within your organization for ongoing day-to-day learning? Note this should not be viewed as “training.” This is how executives “learn” through constant interaction with their changing jobs and changing market conditions. We are headed here not toward “skillsets” but toward “learned strategies and insights.” The difference is material.
- Professor Watkins suggests creating a learning agenda that relates directly to an ongoing learning plan. What don’t you know right now and how are you going to learn what you don’t know? And, importantly, how has the healthcare macroeconomy made your job more difficult and why?
One of my last blogs focused on the importance of vision and strategy in the post-Covid hospital recovery process; the importance of reinventing the hospital of the future that best fits into a rapidly changing marketplace. This marketplace requires entirely new skillsets and functions on top of changing shared experiences and perceived social values. Finding the right going-forward strategy and vision is the first imperative.
But without executive learning and listening that leads directly to organizational-wide learning and listening, the chances of finding your way to that highest and best and most effective vision and strategy will be greatly diminished.