Cartoon – Only Two Kinds of Facts



Ride-hailing service Lyft has hired an executive to lead its expansion into healthcare.
Megan Callahan will join the company as vice president of healthcare, Lyft announced. Callahan, who served most recently as chief strategy officer at Change Healthcare, will lead the strategic direction and growth of Lyft’s healthcare business.
Lyft currently partners with nine health systems and offers healthcare rides in all 50 states and the District of Columbia.
Lyft’s main competitor, Uber, has also launched healthcare-focused initiatives. (Announcement)
Ride-hailing company Uber’s healthcare platform is seeking supporters within the industry to help it expand its reach.
Uber launched the Uber Health dashboard in March, which allows providers to schedule rides for patients and is compliant with the Health Insurance Portability and Accountability Act (HIPAA). The concept was born from the company’s idea to use Uber’s growing influence to improve quality of life beyond commuting to work, said Lauren Steingold, head of strategy at Uber Health.
She said that Uber believes it can play a role in healthcare’s growing interest in home healthcare—helping providers offer more visits in a day—and could supplement nutrition services by delivering food.
More than 100 providers signed on to Uber Health at launch, and the program can be rolled out at any healthcare facility operating in regions where Uber provides its typical services. Steingold said that Uber Health’s growth will rely strongly on word-of-mouth marketing.
“For us, we just need one champion and an organization that gets it,” she said. “If someone believes in what we’re doing, they can champion it and get us over the line.”
Steingold was one of dozens of speakers at U.S. News & World Report’s Healthcare of Tomorrow conference in Washington, D.C., this week.
The healthcare industry is slow to take on new or innovative technology, but having the support of a clinician or a prominent voice within a hospital is what’s driving interest in their platform, she said.
Uber Health allows providers to schedule transportation 30 days in advance and will bill for all rides on a monthly basis. Patients are not billed directly for the rides, and any trips booked through the healthcare dashboard are not linked to that patient’s personal Uber account, if they have one.
Uber Health is also working to address access gaps that can arise for patients who may not have a cellphone. At present, the dashboard will send a text message to the patient when a ride is booked, providing the driver’s license plate number and car model, along with the time and other meetup information.
For patients who may not have a mobile phone, the providers themselves have to call them and offer those details. That hiccup is something Uber is working to address, Steingold said.
She said the company is also looking to expand its reach into underserved, rural areas, which may lack the public transportation alternatives to help patients get to appointments. Drivers are more likely to make themselves available for rides to and from the doctors’ office as more providers embrace Uber’s tools, as visits are often in the mid-day lull for ride-sharing.
Uber is also working with payers, both public and private, to address coverage concerns. Commercial payers have expressed interest in the dashboard, Steingold said, but regulations governing public programs were written long before Uber was conceieved—and are far harder to navigate.
But ride-sharing is finding its place in the healthcare system, she said.
“It’s just a matter of time,” Steingold said.

Hospitals saw a profitable October, spurred by a boost in volume and length of stays, according to a new report.
Kaufman Hall’s latest flash report, based on financial data from 600 hospitals in October, showed improved performance in both operating margin and EBITDA compared to September and to October 2017.
Year-over-year EBITDA margin improvements were reported across the country, aside from the Northeast and mid-Atlantic, with the greatest gains reported in the Midwest. Midsized hospitals with between 200 and 300 beds made the greatest profitability gains, while large hospitals with 500 or more beds struggled to manage costs as effectively, according to the report.
“For Halloween, October delivered a treat rather than a trick for hospitals,” Jim Blake, managing director and publisher at Kaufman Hall, wrote in the report.
A major source of the improvement, according to the report, was a 15.8% month-over-month increase in operating room minutes. Kaufman Hall’s team found a 5.2% increase in discharges and a 3.6% increase in emergency department visits.
Though October’s results were positive, the analysts say it’s hard to determine whether one month of gains portends a longer-term rebound. But in the short term, Kaufman Hall does predict a strong December compared to the year before, though it could trail October and November’s figures.
As increased volume also means increased labor and supply costs, the report additionally spotlights the role the Centers for Medicare & Medicaid Service’s expansion of cuts to 340B discounts could play in the profitability discussion for 2019.
In late 2017, the agency finalized changes to the drug discount program’s payment rate, cutting it to 22.5% less than the average sales price for a drug. For 2019, CMS will expand those changes from hospitals to off-campus provider facilities, which will naturally tighten belts further, according to the report.
The decrease in payments is likely to be less than the $1.6 billion culled from the program in 2018, according to the report, but it does mean hospitals should be paying close attention to how their outpatient and ambulatory facilities prescribe 340B drugs.
It’s especially crucial to be vigilant, according to the report, as it’s likely CMS is considering other changes in this vein, and commercial payers follow the feds’ lead.
“The new CMS rule on 340B drugs is a sign of things to come, and healthcare leaders should be alert to such changes,” according to the report. “The federal government is likely to challenge any lines of business in which hospitals and health systems make significant margins.”

A report commissioned by the American Hospital Association and the Federation of American Hospitals warns that a conglomeration of health measures could result in funding losses of up to $218.2 billion for hospitals by 2028.
The report looked at multiple measures—from sequestration to cuts in Medicare payments for bad debt, hospital coding and documentation adjustment and clarifications to the three-day payment window—to project the cumulative losses between 2010 and 2028.
The single most costly changes they found? Adjustments to Medicare Severity Diagnosis Related Groups documentation and coding, which is expected to add up to $79.3 billion in cuts over that time period.
Here’s a look at what else they took into account:Sequestration
Among the reductions taken into account under sequestration, the Budget Control Act of 2011 imposed across-the-board cuts in federal spending, including a 2% reduction in Medicare payments after April 1, 2013. Sequestration cuts have since been extended several times to stretch through fiscal 2027.
Estimated cost: $73.1 billion by 2028.
Changes to Medicaid Disproportionate Share Hospital payments
The group took multiple pieces of legislation into account, namely the Affordable Care Act, which required cuts to federal DSH payments beginning in 2014 to account for the decrease in uncompensated care anticipated under health insurance coverage expansion. It was delayed but will take effect in 2020 and extend through 2025.
Estimated cost: $25.9 billion between 2020 and 2025
Off-campus provider-based departments
The Bipartisan Budget Act of 2015 modified the CMS definition of provider-based off-campus hospital outpatient departments so only those off-campus PBDs that were billing under CMS’ outpatient prospective payment system prior to November 2015 could continue to bill under the OPPS starting in 2017. Off-campus PBDs would otherwise be eligible under reimbursements from other payment schedules.
Estimated cost: $13.2 billion between 2017 and 2028
Post-acute care reductions
The Medicare Access and CHIP Reauthorization Act of 2015 capped Medicare reimbursements to post-acute care facilities by no more than 1% in fiscal 2018. Further, the Bipartisan Budget Act of 2018 continued restricting inflation-based payment increases for home health services starting in fiscal 2020.
Estimated cost: $6.1 billion between 2018 and 2028.
Hospice transfer policy
The Bipartisan Budget Act of 2018 extended the definition of post-acute care providers to include hospitals, which meant patients who are discharged from an IPPS hospital to a hospital will result in a reduced payment to the hospital starting in fiscal 2019.
Estimated cost: $5.5 billion
Bad debt
Under the Middle-Class Tax Relief and Job Creation Act of 2012, bad debt reimbursement was phased down to 65%.
Estimated cost: $5 billion between 2013 and 2028.
3-day window
This refers to the American Jobs and Closing Tax Loopholes Act of 2010, which was meant to prevent unbundling of related services within three days of an inpatient admission.
Estimated cost: $4.2 billion in 2010 and 2011.
https://www.healthcaredive.com/news/advocate-aurora-raising-minimum-wage-to-15hour/543378/

Health systems are making these moves as they struggle to find employees in the competitive job market. Labor costs remain a major issue for hospitals and have led to nursing strikes over the past two years.
A recent Navigant analysis predicted hospitals and health systems will continue to see higher labor costs in the coming years as administrators raise wages to tackle shortages. Total employment compensation for the industry increased 2% in 2017 and 2.3% the previous year, according to the Bureau of Labor Statistics employment cost index.
Many states are also moving forward with minimum wage increases, including some that have increased pay to $15 an hour.
Brady said the health system’s goal is to be a “destination employer where our team members feel valued, have opportunities for growth and connect with our values and purpose-driven culture.” The decision will improve the workplace and, in turn, make patients “feel this is the best place to entrust their health and wellness,” he added.
Brady said the health system is investing in higher pay while still facing shrinking reimbursements and rising pharmaceutical costs. “Continuing to ensure that our team members have access to rewarding jobs with comprehensive benefits, competitive wages and an engaging work environment will not only strengthen our workplace, it will strengthen our marketplace and most importantly, enhance the quality of life in our communities from Green Bay to Bloomington Normal and everywhere in between,” he wrote to staff.
The Downers Grove, Illinois-based health system was created earlier this year with the merger of Advocate Health Care and Aurora Health Care. The system experienced a 20% drop in operating income in the first six months. The decrease was related to added costs connected to the merger and a new EHR.
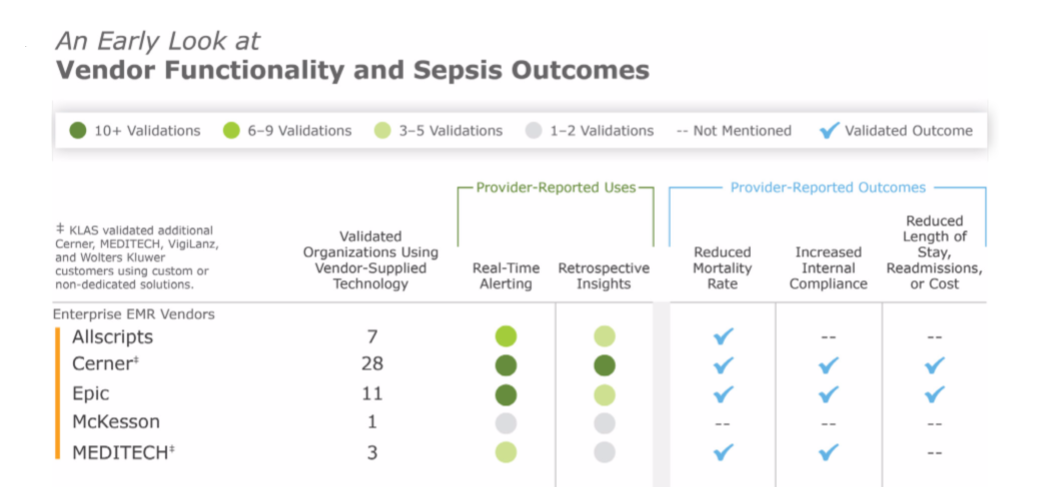
Cerner and Epic offer the most frequently adopted clinical surveillance tools in the provider market, according to a KLAS Research report.
KLAS interviewed providers about their experiences with vendors offering popular clinical surveillance tools for its report. These tools review information from data sources such as EMRs to alert clinicians about a range of patient care activities that decrease readmissions and mortality. The most common use case for clinical surveillance tools today is sepsis detection, according to KLAS.
Cerner and Epic were the only vendors KLAS validated as having “extensive adoption” for their clinical surveillance tools. Of the 17 Cerner customers surveyed, most were using the vendor’s clinical surveillance for sepsis detection. The 18 Epic customers KLAS surveyed tended to use the vendor’s functionalities for sepsis detection, orders checking and floorwide alerts, among a few other less-common use cases.
KLAS noted that although Cerner and Epic were the most widely adopted clinical surveillance vendors, customers of these two vendors tended to be “less satisfied than customers of the other charted vendors in this report,” which included companies like Bernoulli and Stanson Health.
Cerner customers told KLAS they felt the system needed to better integrate with physician workflows and lacked customization options. Epic customers said that the vendor’s alerts were difficult to set up, but were pleased with its ease of use after implementation. KLAS noted Epic does not have a dedicated clinical surveillance modality, but customers have adapted its EMR to provide similar features.
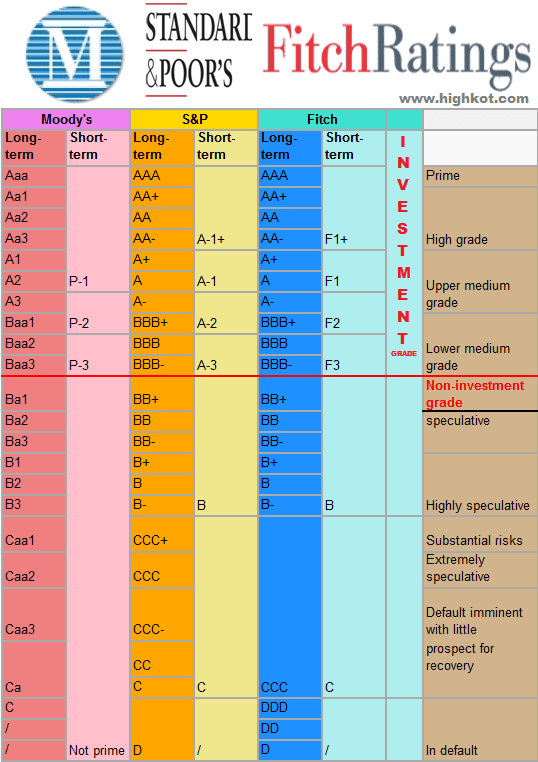
The following hospital and health system credit rating and outlook changes or affirmations occurred in the last week, beginning with the most recent:
1. Fitch affirms ‘AA-‘ rating for SSM Health
Fitch Ratings affirmed St. Louis-based SSM Health’s “AA-” issuer default rating and “AA-“/”F1+” rating where applicable on outstanding rated bonds.
2. Moody’s affirms Cook Children’s Medical Center’s ‘Aa2’ rating
Moody’s Investors Service affirmed its “Aa2” and “Aa2/VMIG 1” ratings for Fort Worth, Texas-based Cook Children’s Medical Center, affecting $356 million of outstanding revenue bonds.
3. Moody’s affirms ‘Baa2’ rating for Children’s Hospital Los Angeles
Moody’s Investors Service affirmed its “Baa2” rating for Children’s Hospital of Los Angeles, affecting $438 million of rated debt.
4. Moody’s affirms ‘A1’ rating for Lucile Packard Children’s Hospital
Moody’s Investors Service affirmed its “A1” revenue bond rating for Palo Alto, Calif.-based Lucile Packard Children’s Hospital.
5. Moody’s affirms ‘A2’ rating for Mary Greeley Medical Center
Moody’s Investors Service affirmed its “A2” rating for Ames, Ia.-based Mary Greeley Medical Center, affecting $64 million of outstanding revenue bonds.
6. Moody’s downgrades Marion County Health and Hospital to ‘Aa2’
Moody’s Investors Service downgraded Marion County (Ind.) Health and Hospital Corp.’s rating from “Aa1” to “Aa2.”
7. Moody’s assigns ‘A2’ rating to HonorHealth
Moody’s Investors Service assigned an “A2” rating to Scottsdale, Ariz.-based HonorHealth’s revenue bonds and affirmed its “A2” rating for the system’s outstanding parity debt.
8. Moody’s upgrades Gainesville Hospital District rating to ‘Ba1’
Moody’s Investors Service upgraded Gainesville (Texas) Hospital District issuer and general obligation limited tax debt ratings from “Ba2” to “Ba1.”
9. Moody’s downgrades Monroe County Health Care Authority rating to ‘Ba1’
Moody’s Investors Service downgraded Monroe County (Ala.) Health Care Authority’s rating from “A3” to “Ba1,” affecting $3.6 million in general obligation limited tax bonds.
10. Moody’s affirms ‘A2’ rating for MedStar Health
Moody’s Investors Service affirmed its “A2” rating on Columbia, Md.-based MedStar Health, affecting $1.4 billion of debt.
11. Moody’s assigns ‘A2’ rating to Mercy Health
Moody’s Investors Service assigned an “A2” rating to Cincinnati-based Mercy Health’s proposed taxable bond and also affirmed its “A2” and “A2/VMIG 1” ratings on the system’s outstanding bonds.
12. S&P revises Spartanburg Regional Health’s outlook to negative
S&P Global Ratings revised its outlook for Spartanburg (S.C.) Regional Healthcare System from stable to negative.
13. S&P affirms ‘A+’ rating for Rush University Medical Center
S&P Global Ratings affirmed its “A+” long-term rating for Chicago-based Rush University Medical Center’s outstanding revenue bonds.
14. S&P raises rating for Columbus Regional Healthcare to ‘A+’
S&P Global Ratings raised its rating for Whiteville, N.C.-based Columbus Regional Healthcare System from “BBB-” to “A+.”