How Big Health Insurers hijacked a medical term and built a denial machine around it.
We hear the term “medically necessary” used every day by insurance companies as a reason to deny or delay health care. While doctors were hard at work treating patients, insurers quietly co-opted the term, and that’s causing serious problems now.
If you ask most doctors to define ‘medically necessary,’ you’ll get some version of: “The test, therapy, drug or procedure that will do the best job of treating my patient.” It’s that simple: whatever is best for my patient.
If you ask an insurer, you may get some legal definition about care “provided for the cure or relief of a health condition, illness, injury or disease (looks good so far, but wait there’s more!), and is not for experimental, investigational or cosmetic purposes and is necessary for and appropriate to the….” The problem begins with the meaning of “necessary and appropriate.”
The terms ‘necessary’ and ‘appropriate’ are left to interpretation. My doctor may feel that a certain test or medication is necessary and appropriate, but someone else may disagree. So how do insurers resolve that disagreement? This is where things go off the rails.
They resolve it by having a medical director they employ review what my doctor wants for me – and that medical director becomes the sole arbiter of what care I can have that will be covered by my health plan. That medical director can sign off on a denial of a claim or a request, and many times they justify that denial by saying the treatment isn’t medically necessary – for reasons that are entirely defined by the health plan.
It seems a clear conflict of interest when an anonymous medical director – possibly lacking in both expertise and experience – rejects a course of treatment laid out by a physician specializing in that disease or condition who has a history with that particular patient. But it happens all the time.
These medical directors work for the company that is denying the claim or request. They have been granted stock and stock options in that company. Their bonus is tied to the financial performance of the company. To say they are impartial and doing what is best for the patient is laughable at best.
Frequently, these medical directors are reviewing requests in areas outside their specialty. In addition, they make these determinations without ever seeing the patient, or reviewing the medical records, studies or lab results that led the treating physician to make the recommendation in the first place. An investigation by ProPublica found that Cigna medical directors were signing off on denials once every 1.2 seconds. This isn’t clinical review; this is profit enhancement.
This brings us to another problem: “coverage policies.” Insurance corporations have created a whole library of coverage policies, and they differ from health plan to health plan. If you’ve never read one of these coverage policies let me save you some time and trouble. Get up now and place your head between the door and the door jam. Now slam the door. You just achieved the headache and confusion that reading a long coverage policy would give you in a fraction of the time. You’re welcome.
Even if you read the policy and think it’s got you covered, you still aren’t home free. A medical director can overrule the policy and still deny the care. Also, that coverage policy may be different for each health plan, and they change from time to time. I am struck by this basic question: Why should the care you receive depend on the insurance card in your wallet and not your clinical situation? The answer, of course, is because that’s how the insurance companies want it.
So, what do we do about this? Let me give you two relatively easy solutions.
First, follow a coverage policy.
If only there was a group of doctors that represented every specialty, we could get them to meet and determine universal coverage policies that could be mandated for all health insurance, both government and commercial. Wouldn’t that be nice? Doctors could then provide good care to patients without having to figure out a library of different coverage policies. Wait, a group like that does exist. It’s called the RUC.
The RUC (Relative Value Scale Update Committee) is an American Medical Association specialty panel, a volunteer group of 32 physicians and over 300 physician advisors who represent every medical specialty. The committee evaluates thousands of individual services across the medical spectrum. Why don’t we ask them to develop a universal set of clinical coverage policies?
Second, fix the denial system. Pass a law that says whenever an insurer denies payment or a request for care, that denial must be signed by a medical doctor, and signing that denial qualifies as “the practice of medicine.” This would make those denials and the doctor who signed off on them subject to all the responsibilities and accountabilities required to practice medicine.
This includes:
- having an active license in the state where the patient is seeking care; practicing within your specialty;
- documenting your decision-making in the patient’s medical record, including the information you reviewed to come to your decision; and
- being liable for malpractice if your decision causes harm to the patient and is not clinically justified.
Let’s assume we had this in place right now and applied it to a real-world situation: the GLP-1 coverage debate. When these glucagon-like peptide-1 drugs for diabetes and weight loss came to market they would have gone before the RUC for a clinical coverage policy. Let’s say the RUC determines that the drugs should be covered for individuals with a BMI over 30 who have tried and failed other diet programs, or for people with a BMI between 25 and 30 who have significant cardiac risk or are diabetic.
Now we have a universal coverage guideline. The doctors prescribing the drug have a very clear understanding of who will be covered and when, and it would apply to all patients regardless of which insurance company they had. As long as the prescribing physician stays inside the guidelines, no denials would be expected.
Let’s take an example from the flip side. A doctor wants to prescribe an expensive chemotherapy regimen to an elderly patient with cancer. The insurer could have that request reviewed and possibly denied by a medical director. However, that medical director would need to be an oncologist with a valid license in the state where the patient is getting treatment. If that oncologist reviews the patient information, denies the chemotherapy for valid clinical reasons, and documents those reasons in the patient’s chart, then the insurer can deny the request.
These two changes would eliminate so many problems, improve the lives of doctors, improve the lives of patients, and reduce administrative costs.
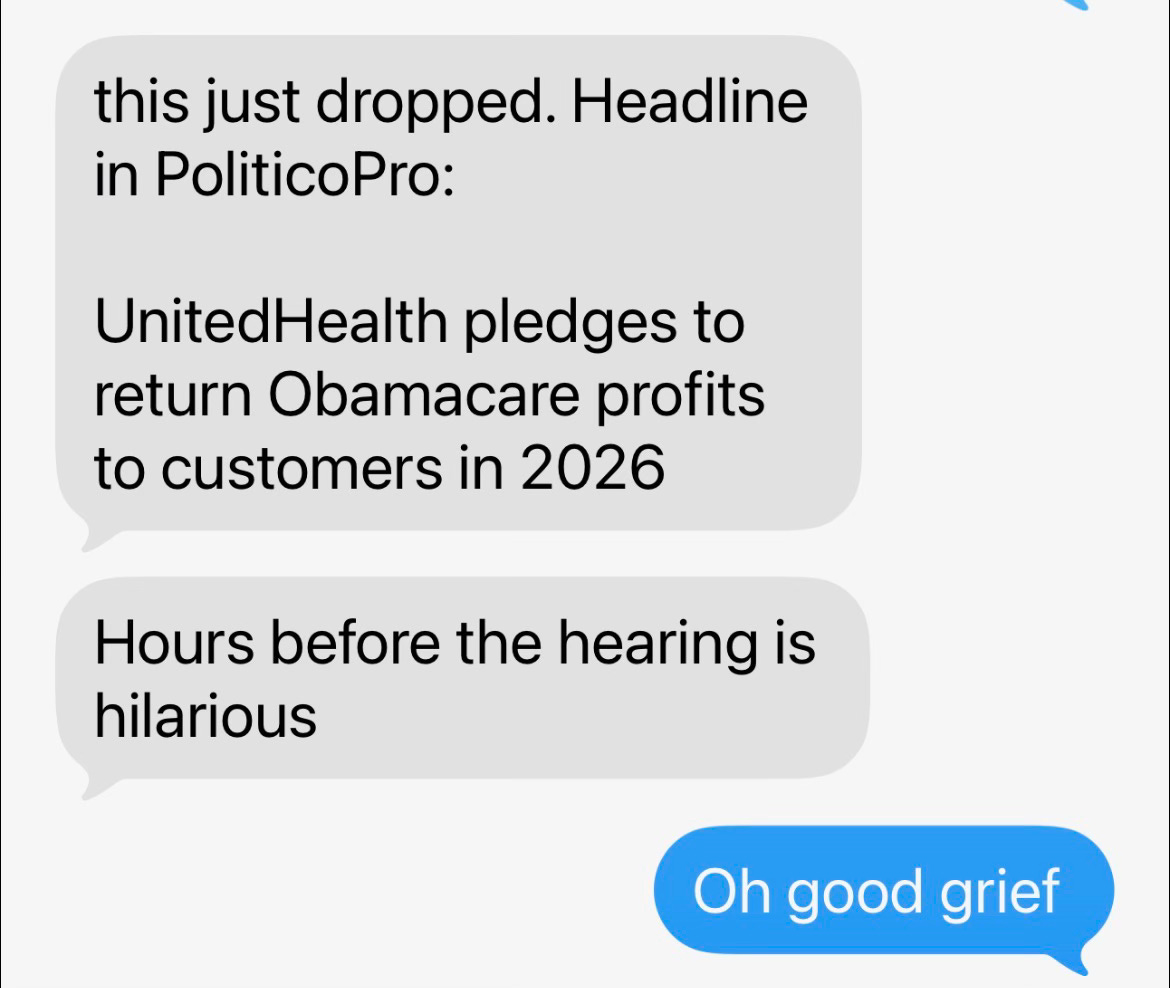
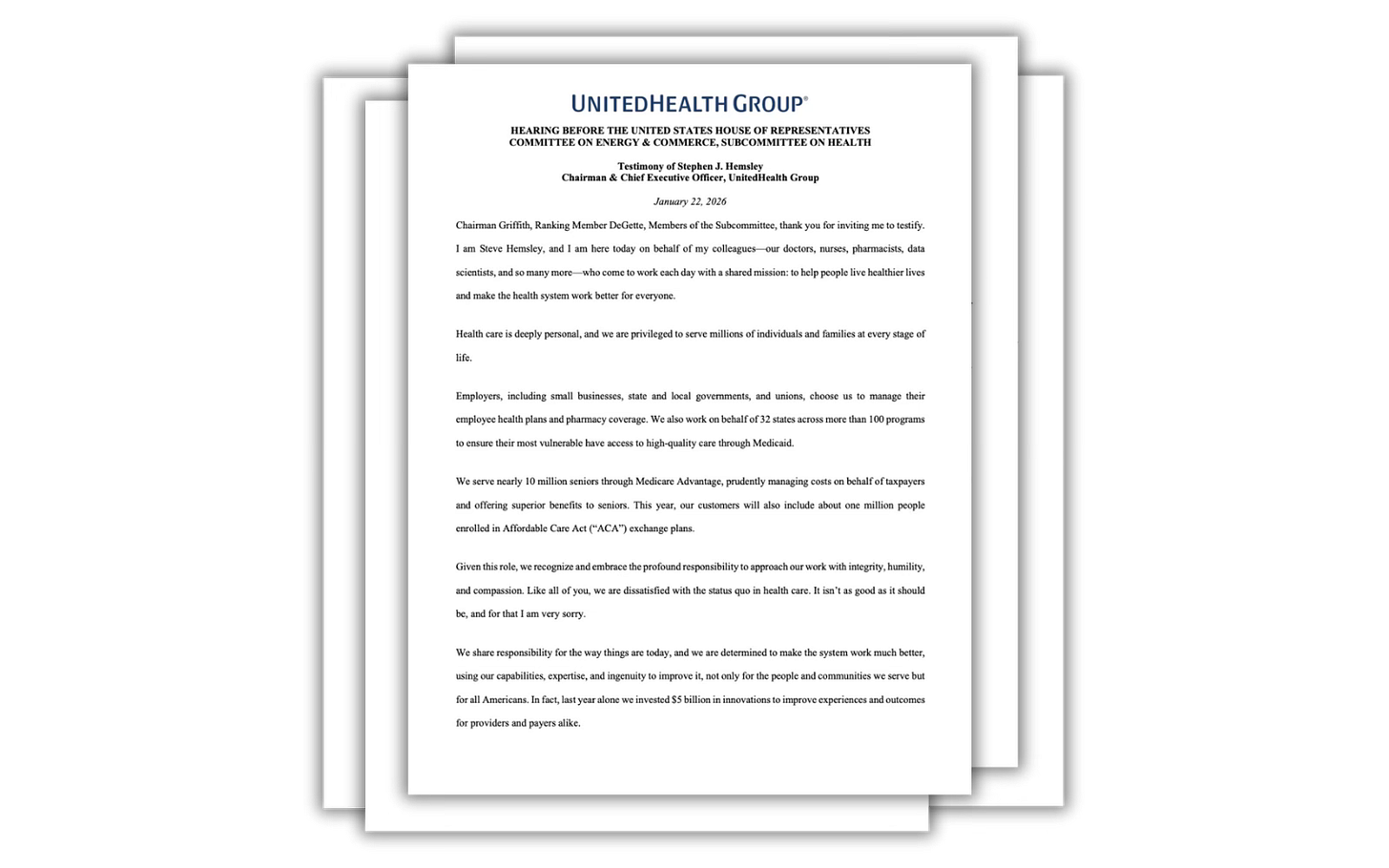
So why hasn’t this been done already? Well the one thing these changes would not do is increase the stock prices of insurance companies.
To put it more succinctly, it’s profits over patients. That’s why.