http://www.charlotteobserver.com/news/politics-government/article160601814.html

New data on the improving finances of the nation’s individual insurers are calling into question repeated Republican claims that Obamacare marketplaces are collapsing under the Affordable Care Act.
For months, Republican leaders from President Donald Trump and Health and Human Services Secretary Tom Price to House Speaker Paul Ryan have said Obamacare was crumbling under its own weight and could not be saved. And this week, when HHS announced a 38 percent decline in the number of insurers that want to offer coverage next year in states that use the federal marketplace, Price said, “The situation has never been more dire.”
But new research released Monday by the Kaiser Family Foundation shows that profitability and other financial measures for individual insurers have dramatically improved over the last year.
“Now it looks like they’re on track to be profitable and that they’re actually having the best year that they’ve had since the ACA began,” said Cynthia Cox, associate director of health reform at Kaiser.
The share of premiums paid out as medical claims by individual insurers fell to 75 percent in the first quarter of 2017, down from 86 percent in the first three months of 2016 and 88 percent in the first quarter of 2015.
In addition, average monthly premium income exceeded monthly per-enrollee medical claims by roughly $100 in the first quarter of 2017, Kaiser reported. That’s up from about $48 in the first quarter of 2016 and just over $36 in the first quarter of 2015.
Throughout their push to repeal the Affordable Care Act, Republicans have said the market troubles in some areas were proof that Obamacare was unraveling and legislative change was needed. In a pair of tweets on May 4, Trump declared that ObamaCare was “dead” and the individual market was in a “Death spiral!,” in which insurance offerings disappear as premium hikes force all but the sickest to drop coverage.
Cox disputed that assessment: “There’s not really signs of a death spiral here,” she said.
The report, based on insurers’ first-quarter financial reports filed with the National Association of Insurance Commissioners and compiled by Mark Farrah Associates, comes as Senate Majority Leader Mitch McConnell struggles to find 50 votes to pass his Obamacare repeal legislation. Facing opposition from some conservatives, he has expressed a willingness to negotiate with Democrats on a legislative fix of the ACA as Republicans try to re-draft their legislation and move forward next week.
But Monday’s report could make across-the-aisle appeals more difficult, as the data indicates insurers could be on the verge of righting their financial ship.
In a letter to McConnell on Monday, four Democratic senators — Charles Schumer of New York, Debbie Stabenow of Michigan, Richard Durbin of Illinois and Patty Murray of Washington — urged McConnell make “common sense reforms” such as guaranteeing the cost-sharing payments, creating a permanent reinsurance program and finding solutions for areas without insurers.
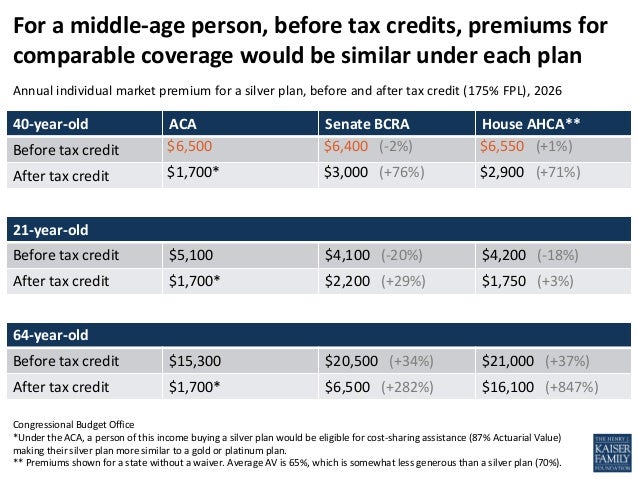
Certainly, some marketplaces remain under enormous pressure. Far fewer people than originally expected enrolled into marketplace coverage and those who did were sicker, older and more costly than insurers expected. As losses mounted, insurers sharply increased premiums in 2017, making coverage unaffordable for many as enrollment slipped. Some insurers exited unprofitable markets altogether, leaving 38 rural counties in Ohio, Indiana and Nevada with the possibility of no coverage options next year, according to Kaiser. Five states — Alabama, Alaska, Oklahoma, South Carolina and Wyoming — have only one insurer offering marketplace coverage this year.
The Trump administration added to insurers’ problems by relaxing enforcement of Obamacare’s individual mandate and refusing to reimburse insurers for billions of dollars of financial assistance, known as cost-saving reductions, that go to low-income plan members.
An analysis by the Oliver Wyman consulting firm estimated that up to two-thirds of insurer rate increases for 2018 “will be due to the uncertainty surrounding these two market influences” and the Congressional Budget Office estimates premiums will increase 20 percent next year if the individual mandate is not enforced.
Blue Cross Blue Shield of North Carolina, which has more than 500,000 individual policy holders, wants to increase rates on their Obamacare plans by an average of 23 percent next year.
Speaking in Washington, DC at a recent Bipartisan Policy Center panel discussion, J. Brad Wilson, President and CEO of BCBS North Carolina said, “Over 50 percent of that increase is attributable to the uncertainty of CSRs.”
The industry trade group America’s Health Insurance Plans would not comment on the report.