As Donald Trump begins his second term, America’s healthcare system is in crisis: medical costs are skyrocketing, life expectancy has stagnated, and burnout runs rampant among healthcare workers.
These problems are likely to become worse now that Trump has handed the federal budget over to Elon Musk. The world’s richest man now co-heads the Department of Government Efficiency (DOGE), a non-government entity tasked with slashing $500 billion in “wasteful” spending.
The harsh reality is that Musk’s mission can’t succeed without gutting healthcare access and coverage for millions of Americans.
Deleting dollars from American healthcare
Since Trump’s first term, the country’s economic outlook has worsened significantly. In 2016, the national debt was $19 trillion, with $430 billion allocated to annual interest payments. By 2024, the debt had nearly doubled to $36 trillion, requiring $882 billion in debt service—12% of federal spending that is legally untouchable.
Add to that another 50% of government expenditures that Trump has deemed politically off-limits: Social Security ($1.35 trillion), Medicare ($848 billion) and Defense ($1.13 trillion). That leaves just $2.6 trillion—less than 40% of the $6.75 trillion federal budget—available for cuts.
In a recent op-ed, Musk and DOGE co-chair Vivek Ramaswamy proposed eliminating expired or misused funds for programs like Public Broadcasting and Planned Parenthood, but these examples account for less than $3 billion total—not even 1% of their target.
This shortfall will require Musk to cut billions in government healthcare spending. But where will he find it?
With Medicare off limits to DOGE, the options for major reductions are extremely limited. Big-ticket healthcare items like the $300 billion in tax-deductibility for employer-sponsored health insurance and $120 billion in expired health programs for veterans will prove politically untouchable. One will raise taxes for 160 million working families and the latter will leave veterans without essential medical care.
This means DOGE will have to attack Medicaid and the ACA health exchanges. Here’s how 20 million people will likely lose coverage as a result.
1. Reduced ACA exchange funding
Since its enactment in 2010, the Affordable Care Act (ACA) has provided premium subsidies to Americans earning 100% to 400% of the federal poverty level. For lower-income families, the ACA also offers Cost Sharing Reductions, which help offset deductibles and co-payments that fund 30% of total medical costs per enrollee. Without CSRs, a family of four earning $40,000 could face deductibles as high as $5,000 before their insurance benefits apply.
If Congress allows CSR payments to expire in 2026, federal spending would decrease by approximately $35 billion annually. If that happens, the Congressional Budget Office expects 7 million individuals to drop out of the exchanges. Worse, without affordable coverage alternatives, 4 million families would lose their health insurance altogether.
2. Slashing Medicaid coverage and tightening eligibility
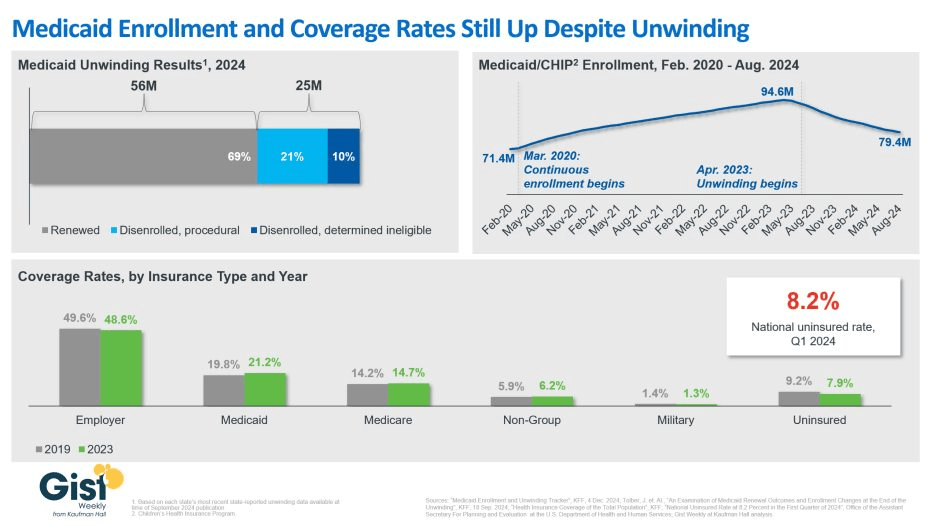
Medicaid currently provides healthcare for over 90 million low-income Americans, including children, seniors and individuals with disabilities. To meet DOGE’s $500 billion goal, several cost-cutting strategies appear likely:
- Reversing Medicaid expansion: The ACA expanded Medicaid eligibility to those earning up to 138% of the federal poverty level, reducing the uninsured rate from 16% to 8%. Undoing this expansion would strip coverage from millions in the 40 states that adopted the program.
- Imposing work requirements: Proponents argue this could encourage employment, but most Medicaid recipients already work for employers that don’t provide insurance. In reality, work requirements primarily create bureaucratic barriers that disqualify millions of eligible individuals, reducing program costs at the expense of coverage.
- Switching to block grants: Unlike the current Medicaid system, which adjusts funding based on need, less-expensive block grants would provide states with fixed allocations. This will, however, force them to cut services and reduce enrollment.
Medicaid currently costs $800 billion annually, with the federal government covering 70%. Reducing enrollment by 10% (9 million people) could save over $50 billion annually, while a 20% reduction (18 million people) could save $100 billion.
Either outcome would devastate families by eliminating access to vital services including prenatal care, vaccinations, chronic disease management and nursing home care. As states are forced to absorb the financial burden, they’ll likely cut education budgets and reduce infrastructure investments.
The first 100 days
The numbers don’t lie: Musk and DOGE could slash Medicaid funding and ACA subsidies to achieve much of their $500 billion target. But the human cost of this approach would be staggering.
Fortunately, there are alternative solutions that would reduce spending without sacrificing quality. Shifting provider payments in ways that reward better outcomes rather than higher volumes, capping drug prices at levels comparable to peer nations, and leveraging generative AI to improve chronic disease management could all drive down costs while preserving access to care.
These strategies address the root causes of high medical spending, including chronic diseases that, if better managed, could prevent 30-50% of heart attacks, strokes, cancers, and kidney failures according to CDC estimates.
Yet, in their pursuit of immediate budgetary cuts, Musk and DOGE have omitted these kinds of reform options. As a result, the health of millions of Americans is at major risk.