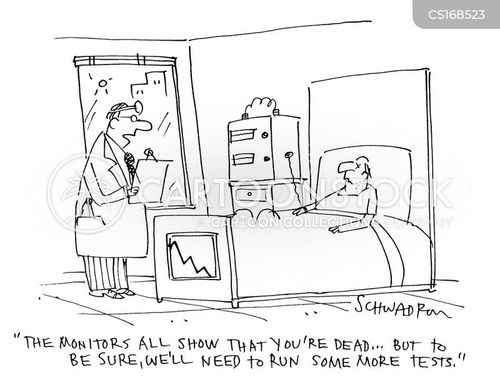
Cartoon – That Was Close!



Get ready for about six more months of headlines like this: Insurers in Maryland are proposing premium hikes as high as 91% for coverage sold through the Affordable Care Act.
This will keep happening, nationwide. Proposed increases have been steep in Maryland and Virginia, the first two states to release them. But all signs point to steep hikes across the country, especially in rural areas. Some insurers also will likely decide to simply quit offering coverage in some parts of the country.
The latest: Insurers in Maryland’s individual market are seeking rate hikes for next year that range from 18% (for the biggest plan in the state) to 91% (for the smallest). They average out to roughly 32%.
Why you’ll hear about this again: More preliminary rates will trickle out until the summer, as will any insurers’ decisions to pull up stakes in some markets. After negotiations with state regulators, rates will be finalized a few weeks before the midterms.
The other side: Expect the Trump administration to cite these same figures as it finalizes regulations that would loosen access to options outside the ACA’s exchanges, saying they’re providing new options to people who simply can’t afford ACA coverage.

Imagine you’re living with type 2 diabetes. You’ve been trying to manage the condition for years with a typical medication. What if instead of metformin — a drug that works to lower sugar in the blood, — our doctor could simply prescribe meals tailored to your unique diagnosis that help control your blood sugar? A growing body of research indicates that such a shift in treatment, away from Big Pharma and towards common-sense treatment measures, is the future of U.S. health care.
For too long, the sickest patients in this country have been ill-served by a system that rewards doctors and insurers for the volume of services they render versus the quality of health outcomes their methods deliver. “Food Is Medicine” is a new approach that nonprofits, politicians, medical centers and nutrition experts are increasingly recommending as a low-cost, high-impact intervention that complements or supplants the use of expensive, pharmaceutical drugs.
In recognition of this growing medical consensus, the House Hunger Caucus recently launched a bipartisan Food is Medicine Working Group, led by Rep. Jim McGovern (D-Mass.) and other caucus members, the overarching goal of which is the better alignment of government nutrition policy and health outcomes.
Some of the group’s suggestions are policy initiatives including: incentivizing the purchase of healthy food, strengthening the Supplemental Nutrition Assistance Program (SNAP), adding medically tailored meals to the care plans of those fighting severe and chronic diseases and programs through which doctors can prescribe well-balanced diets.
Chronic diseases afflict 120 million Americans and account for an astounding 75 percent of U.S. healthcare spending. The need for creative solutions to help our nation’s highest need consumers of health services is significant. By taking steps like those outlined above by McGovern in January, we will be moving towards a more effective system for keeping people healthy and out of the doctor’s office. We will also be saving patients and insurers a lot of money.
The Hunger Caucus’ Food is Medicine Working Group meets this week to discuss the research, policy and practice of incorporating medically tailored meals into healthcare across the country.
Medically tailored meals (MTM) are meals tailored to the specific medical conditions, medications, side effects, allergies and other needs of a person living with severe or chronic illness. In this briefing, two recent studies will be discussed, both of which present compelling evidence that MTM can significantly improve health outcomes while curbing care costs. Both studies involved MTM provided by Food is Medicine Coalition nonprofit organizations. FIMC is a national alliance of MTM providers that I am proud to lead as the President & CEO of God’s Love We Deliver.
As a result of the findings published in a 2013 study, MANNA in Philadelphia partnered with Pennsylvania-based Medicaid managed care organization Health Partners Plans on an ongoing contract that resulted inthe delivery of medically tailored meals to HPP members living with illnesses like diabetes, heart disease, malnutrition and kidney failure.
That study found a 28 percent reduction in inpatient hospitalization and 9 percent reduction in ED visits, when members received medically tailored meals. Another MTM provider, Community Servings in Boston, conducted a retrospective claims analysis study with Massachusetts General Hospital and determined a 16 percent net healthcare cost savings with MTM. Results were published in Health Affairs.
In each instance, medical diets helped keep ill patients out of the hospital, which is critically important considering that one can provide half a year’s worth of medically tailored meals for the cost of one night in a hospital.
God’s Love We Deliver has found similar results in people living with HIV and FIMC agency Project Open Hand in San Francisco demonstrated cost savings for patients with type 2 diabetes and increased adherence for people living with HIV.
The Food is Medicine Coalition strives for a positive continuation of the trend towards expanded healthcare access brought to this country by the Affordable Care Act close to a decade ago. The ACA allowed organizations focusing on the medically underprivileged, like those within the Food is Medicine Coalition, to work in a grassroots manner with regional Medicaid programs to implement additional benefits, like medically tailored food and nutrition, to high-need patients’ care plans.
The good sense of keeping a healthy diet shouldn’t be news to anyone. We sometimes lose sight, however, of how our basic everyday behaviors influence our long-term health. “Food Is Medicine” is more than a quaint cliché. It’s a proven, viable healthcare solution that must become a more central aspect to how we deal with an American epidemic of chronic illness.
http://www.latimes.com/local/education/la-me-uc-workers-strike-20180507-story.html
A massive labor strike across the University of California on Monday forced medical centers to reschedule more than 12,000 surgeries, cancer treatments and appointments, and campuses to cancel some classes and limit dining services.
More than 20,000 members of UC’s largest employee union, the American Federation of State, County and Municipal Employees Local 3299, walked off their jobs on the first day of a three-day strike. They include custodians, gardeners, cooks, truck drivers, lab technicians and nurse aides.
Two altercations involving protesters and people driving near the rallies were reported at UCLA and UC Santa Cruz. At UCLA, police took a man into custody Monday after he drove his vehicle into a crowd, hitting three staff members. They were treated for minor injuries at the scene and released, said Lt. Kevin Kilgore of the UCLA Police Department.
The system’s 10 campuses remained open, largely operating on regular schedules, and protests were peaceful and even festive.
At UCLA, workers marched through campus in green union shirts that said “We run UC” and held signs calling for equality, respect and more staff. Some brought children and walked dogs. Drivers honked in solidarity. Hundreds of workers rallied in front of the Ronald Reagan UCLA Medical Center, taking taco breaks under green balloons.
Oscar Rubio, a UCLA food services worker, said that staffing at some dining hall stations has been cut from five workers to three, leading to more injuries for those who remain.
Top UC officials “make more money … while we suffer,” Rubio said. “We’re not asking to make like they make. We’re asking to support us enough to pay our rent.”
The walkout is expected to widen Tuesday, when two other unions will join sympathy strikes. About 14,000 members of the California Nurses Assn., who work at UC’s medical centers and student health clinics, are set to walk off their jobs, along with 15,000 members of the University Professional & Technical Employees, who include pharmacists, clinical social workers, physical therapists, physician assistants and researchers.
The union and university reached a bargaining impasse last year. Subsequent mediation efforts have failed to produce an agreement on wage increases, healthcare premiums and retirement terms. A recent union study on pay disparities angered workers, said AFSCME spokesman John de los Angeles. The study used UC data, union officials say, to show that starting wages of blacks and Latinos were about 20% lower than white workers in comparable jobs.
“The strong showing sent a clear message to administrators that our workers are very concerned about inequity and they’re willing to be on the picket line until UC comes up with a proposal to address their concerns,” De los Angeles said.
UC officials say they cannot confirm the study’s accuracy. They criticized the union’s demands, which include a multiyear contract with annual pay raises of 6%, no increase in healthcare premiums and continued full pension benefits at the retirement age of 60. The university is offering 3% annually over four years, which officials say is equal to raises given to other UC employees. UC also wants to raise the retirement age to 65 for new employees who choose a pension instead of a 401(k) plan and to raise monthly health insurance premiums by a maximum $25.
“Unfortunately, the only thing union leaders accomplished today is hurt the care we provide our patients and the services for our students,” UC spokeswoman Claire Doan said in an email Monday. “It will do nothing to change UC’s position on AFSCME’s unreasonable demands for excessive raises and benefits.”
At UC’s request, a Sacramento County Superior Court judge issued a temporary restraining order Friday barring certain essential employees, such as pharmacists and respiratory therapists, from participating in order to protect public health and safety. AFSCME also assembled a “patient protection task force” to respond to life-threatening emergencies.
UC’s five medical centers hired contract workers to fill in during the strike and scrambled to reschedule exams and treatments. UC San Francisco rescheduled more than 12,000 appointments for surgeries and treatments, including chemotherapy and radiation.
UC Davis rescheduled several hundred appointments, including more than 100 cancer surgeries and 150 radiology exams. But campus spokeswoman Kimberly Hale said 78% of UC Davis health workers showed up for work. UC San Diego directed emergency room patients to other hospitals.
At UC Santa Cruz, where more than 150 protesters assembled at both entrances Monday, Chancellor George Blumenthal canceled most morning classes. Services were limited for hours at the student health center and some libraries and dining halls. Santa Cruz Metro buses did not enter the campus, dropping riders off at the entrance.
Samuel Walcoff, a sophomore studying computer science, said he had to trek up the hills to get to his afternoon lab and scrounge for food.
“I’m not at all opposed to people protesting and striking, but to have students who are powerless pay the price is extremely unfair,” he said.
At UC Berkeley, however, freshman Ella Smith said she supported the workers even though there was no Peet’s Coffee service inside the Golden Bear Cafe.
“Us not getting our morning coffee does not compare to the injustice UC workers face due to the inequity and inequality in their work experience,” she said in an email.
Some faculty members chose to teach off-campus to avoid crossing the picket line or to use the strike to discuss labor rights.
Paul Spickard, a UC Santa Barbara professor, has invited striking workers to speak Tuesday to the more than 300 students in his modern world history class.
“The UC system has been starved of money by the state,” he said in an email. “We have chosen to pay even lower wages to staff … than to faculty. That is shameful. They are our colleagues and the university would not run without them.”
Reyna and Dennis Avila both work at UCLA Medical Center — he as a hospital assistant, she as a secretary, monitor technician and nurse’s assistant. To juggle their schedules with one car and different work shifts, the couple leave their home in Inglewood at 2:45 a.m. Dennis starts work at 4 a.m. while Reyna sleeps in the car until her shift begins at 7 a.m. He takes the car home, and she returns by bus.
Reyna said her pay increases over two decades at UCLA have not kept up with rising rent.
“It’s gotten harder to make ends meet,” she said.

The Trump administration is unveiling a multibillion-dollar roster of proposed spending cuts but is leaving this year’s $1.3 trillion catchall spending bill alone.
The cuts wouldn’t have much impact, however, since they come from leftover funding from previous years that wouldn’t be spent anyway.
The White House said it is sending the so-called rescissions package to lawmakers Tuesday. Administration officials, who required anonymity because they weren’t authorized to speak publicly on the matter, said the package proposes killing $15 billion in unused funds. A senior official said about $7 billion would come from the Children’s Health Insurance Program, or CHIP, which provides health care to kids from low-income families, though that official stressed the cuts won’t have a practical impact on the popular program.
The administration is trying to use its authority to prod Congress to “rescind” spending approved years ago, but even if the package is approved it would only have a tiny impact on the government’s budget deficit, which is on track to total more than $800 billion this year. Some of the cuts wouldn’t affect the deficit at all since budget scorekeepers don’t give credit for rescinded money that they don’t think would have ever been spent.
For instance, more than $4 billion in cuts to a loan program designed to boost fuel-efficient, advanced-technology vehicles wouldn’t result in fewer loans since the loans are no longer being made. And $107 million worth of watershed restoration money from the 2013 Superstorm Sandy aid bill is going unused because local governments aren’t stepping up with matching funds. Another $252 million is left over from the 2015 fight against Ebola, which has been declared over.
Still, the cuts, if enacted by Congress, would take spending authority off the table so it couldn’t be tapped by lawmakers for other uses in the future. The catchall spending bill, for instance, contained $7 billion in cuts to CHIP that were used elsewhere to boost other programs.
“This is money that was never going to be spent,” a senior administration official said on a press call ahead of Tuesday’s submission. “The only thing it would be used for is offsets down the line.”
Democrats have supported such cuts in the past, eager to grab easy budget savings to finance new spending. But some Democrats howled over the White House proposal anyway.
“Let’s be honest about what this is: President Trump and Republicans in Congress are looking to tear apart the bipartisan Children’s Health Insurance Program (CHIP), hurting middle-class families and low-income children,” said Senate Minority Leader Chuck Schumer, D-N.Y.
Pressure from party conservatives to increase cuts in a tentative $11 billion proposal contributed to a delay from Monday’s original release date.
The White House and tea party lawmakers upset by the budget-busting “omnibus” bill have rallied around the plan, aiming to show that Republicans are taking on out-of-control spending. The administration says it will propose cuts to the omnibus measure later in the year.
The spending cuts are also a priority for House Majority Leader Kevin McCarthy, R-Calif., who likens them to “giving the bloated federal budget a much-needed spring cleaning.” But while the package may pass the House it faces a more difficult path — and potential procedural roadblocks — in the Senate.
McCarthy wants to succeed soon-to-retire House Speaker Paul Ryan, R-Wis., and some of his allies view the project as a way to improve his standing with fractious GOP conservatives who blocked his path to the speakership in 2015.
The proposal has already had a tortured path even before its unveiling. More pragmatic Republicans, including the senior ranks of the powerful House and Senate Appropriations committees, rebelled against the measure. They argued that it would be breaking a bipartisan budget pact just weeks after it was negotiated. In response, White House budget director Mick Mulvaney cleansed the measure of cuts to the huge omnibus bill.
Last month, Mulvaney told lawmakers the plan could have totaled $25 billion or so. Now he says he’s planning to submit several different packages of spending cuts — and it’s likely they’ll get more conservative with each new proposal.
Either way, the idea faces a challenging path in Congress — particularly the Senate, where a 51-49 GOP majority leaves little room for error even though budget rules permit rescissions measures to advance free of the threat of Democratic filibusters. But the cuts to the popular children’s health insurance program probably could still be filibustered because they are so-called mandatory programs rather than annual appropriations.
https://khn.org/news/medicare-beneficiaries-feel-the-pinch-when-they-cant-use-drug-coupons/

This week, I answered a grab bag of questions about drug copay coupons and primary care coverage on the health insurance marketplace.
Q: My doctor wants me to take Repatha for my high cholesterol, but my Medicare drug plan copayment for it is $618 a month. Why can’t I use a $5 drug copay coupon from the manufacturer? If I had commercial insurance, I could. I’m on a fixed income. How is this fair?
The explanation may offer you little comfort. Under the federal anti-kickback law, it’s illegal for drug manufacturers to offer people any type of payment that might persuade them to purchase something that federal health care programs like Medicare and Medicaid might pay for. The coupons can lead to unnecessary Medicare spending by inducing beneficiaries to choose drugs that are expensive.
“The law was intended to prevent fraud, but in this case it also has the effect of prohibiting Part D enrollees from using manufacturer copay coupons … because using the coupon would be steering Medicare’s business toward a particular entity,” said Juliette Cubanski, associate director of the Program on Medicare Policy at the Kaiser Family Foundation. (Kaiser Health News is an editorially independent program of the foundation.)
The coupons typically offer patients with commercial insurance a break on their copayment for brand-name drugs, often reducing their out-of-pocket costs to what they would pay for inexpensive generic drugs. The coupons help make expensive specialty drugs more affordable for patients. They can also increase demand for the drugmaker’s products. If patients choose to use the coupons to buy a higher-cost drug over a generic, the insurer’s cost is likely to be more than what it would otherwise pay.
In addition, consumers should note that the copay cards often have annual maximums that leave patients on the hook for the entire copayment after a certain number of months, said Dr. Joseph Ross, associate professor of medicine and public health at Yale University who has studied copay coupons.
The coupons may discourage patients from considering appropriate lower-cost alternatives, including generics, said Leslie Fried, a senior director at the National Council on Aging.
According to a 2013 analysis co-authored by Ross and published in the New England Journal of Medicine, 62 percent of 374 drug coupons were for brand-name drugs for which there were lower-cost alternatives available.
Q: Last year, my marketplace plan covered five primary care visits at no charge before I paid down my $2,200 deductible. This year, it doesn’t cover any appointments before the deductible, and I had to pay $80 out-of-pocket when I went to the doctor. Is that typical now? It makes me think twice about going.
Under the Affordable Care Act, marketplace plans are required to cover many preventive services, including an annual checkup, without charging consumers anything out-of-pocket. Beyond that, many marketplace plans cover services such as some primary care visits or generic drugs before you reach your deductible.
The likelihood of having a plan that offers some cost sharing for primary care before you reach your deductible (rather than requiring you to pay 100 percent of the cost until you hit that amount) varies significantly depending on whether you’re in a bronze, silver or gold plan, according to a recent analysis by the Robert Wood Johnson Foundation.
In 2018, 77 percent of silver-level plans offered some cost sharing for primary care visits before enrollees had paid off their typical deductible of $3,800, the analysis found. In most cases, that means people owe a copayment or coinsurance charge for each visit until they reach their deductible. A small number of plans offered a limited number of no-cost or low-cost visits first, and then people using more services either had to pay the full charge for each visit or owed cost sharing until the deductible was met.
Bronze plans were much stingier in what they offered for primary care before people reached their deductible, which was $6,400 or higher in half of plans. Only 38 percent of bronze plans offered any primary care coverage before the deductible, and generally patients still had to pay a copayment or coinsurace. A smaller percentage of bronze plans offered limited visits at no cost or low cost before the deductible.
The share of people who chose bronze plans grew from 23 percent in 2017 to 29 percent this year, said Katherine Hempstead, a senior policy adviser at the Robert Wood Johnson Foundation. While premiums are typically significantly lower in bronze plans than other “metal”-level plans, it can be worthwhile to check out how plans handle primary care services before the deductible, she said.
https://khn.org/news/how-the-farm-bill-could-erode-part-of-the-aca/

Some Republican lawmakers continue to try to work around the federal health law’s requirements. That strategy can crop up in surprising places. Like the farm bill.
Tucked deep in the House version of the massive bill — amid crop subsidies and food assistance programs — is a provision that supporters say could help provide farmers with cheaper, but likely less comprehensive, health insurance than plans offered through the Affordable Care Act.
It calls for $65 million in loans and grants administered by the Department of Agriculture to help organizations establish agricultural-related “association” type health plans.
But the idea is not without skeptics.
“I don’t know that anyone at the Department of Agriculture, with all due respect, knows a darn thing about starting and maintaining a successful insurance company,” said Sabrina Corlette, a professor and project director at the Georgetown University Health Policy Institute.
Association health plans are offered through organizations whose members usually share a professional, employment, trade or other relationship, although the Trump administration is soon to finalize new rules widely expected to broaden eligibility while loosening the rules on benefits these plans must include.
Under that proposal, association plans would not have to offer coverage across 10 broad “essential” categories of care, including hospitalization, prescription drugs and emergency care. They could also spend less premium revenue on medical care.
Under the farm bill, the secretary of Agriculture could grant up to 10 loans of no more than $15 million each, starting next year, to existing associations whose members are ranchers, farmers or other agribusinesses.
The language is strikingly similar to a bill introduced April 12 by Rep. Jeff Fortenberry (R-Neb.), a supporter of association health plans. He did not respond to calls for comment.
Although the farm bill is usually considered “must-pass” by many lawmakers, it is currently facing pushback because of controversy surrounding other parts of the measure, mainly language that would add additional work requirements to the food stamp program.
Still, the focus on association health plans won’t go away.
The plans — coupled with another Trump administration move to make short-term insurance more widely available — could draw healthier people out of the ACA markets, leaving the pool of beneficiaries with higher percentages of people who need medical care. And that, some say, could drive up premiums for those who remain.
The National Association of Insurance Commissioners, for example, has warned that association plans “threaten the stability of the small group market” and “provide inadequate benefits and insufficient protection to consumers.”
Actuaries have made similar arguments.
Others are concerned about the idea of the government providing funding for such plans.
“We have reams of experience with AHPs that have gone belly up … and the notion that we should put taxpayer money into them is irresponsible,” said Georgetown University’s Corlette.
She was referring to the industry’s mixed track record with plans. Some have served members well, but other plans have been marked by solvency problems that left consumers on the hook with unpaid medical bills or were investigated for providing little or no coverage for such things as chemotherapy or doctor office visits.
It’s not fair to simply focus on the failures, countered attorney Christopher Condeluci, who served as tax and benefits counsel to the Senate Finance Committee and now advises private clients, some of whom are interested in association plans.
“Some AHPs were not successful,” he agreed. “But there’s arguably more examples of AHPs that work. The trouble is everyone focuses on the negative.”
Although the GOP generally supports association plans, using taxpayer funds to help start them could prove problematic for some conservatives in Congress.
Many Republican lawmakers expressed concerns about the use of tens of millions of taxpayer dollars to start insurance co-ops that were part of the ACA, most of which failed.
“The hard-earned tax dollars collected from working Americans, sitting at Treasury right now, are not venture capital, said Rep. Kevin Brady (R-Texas) at a subcommittee hearing in November 2015. Currently, Brady is chairman of the powerful House Ways and Means Committee.
The provision could also be popular in rural areas.
“We think it’s a good idea,” said Rob Robertson, chief administrator for the Nebraska Farm Bureau Federation, whose group is considering sponsoring one.
About half of his members, Robertson said, have a spouse working a non-farm job, mainly for insurance coverage. Of those who buy their own plan, some are facing astronomical premiums and are looking for relief.
“I can’t think of any sector that is affected more by the huge premium increases under Obamacare than farmers and ranchers,” he said.
The farm bill — including the AHP provision — was approved by the House Committee on Agriculture in mid-April, and is currently awaiting floor consideration. Meanwhile, a final rule on the Trump AHP rule, which has drawn more than 900 comments from supporters and opponents, could be issued as early as this summer.