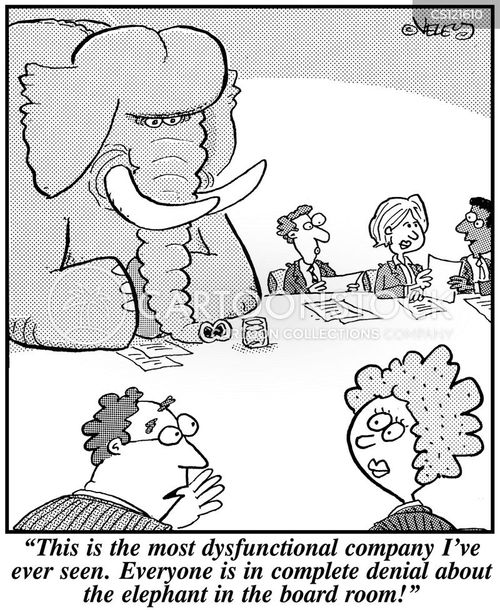
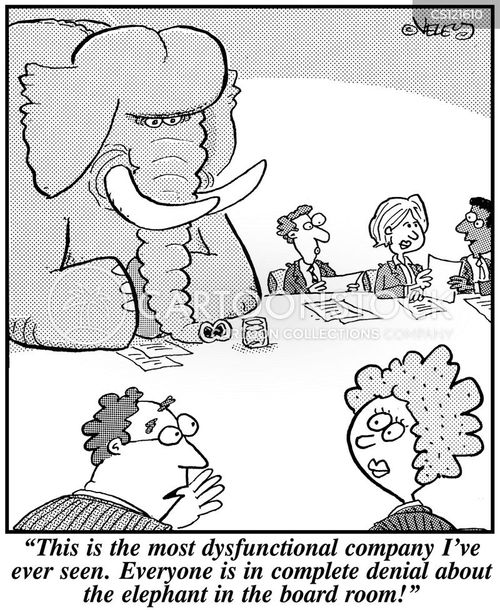
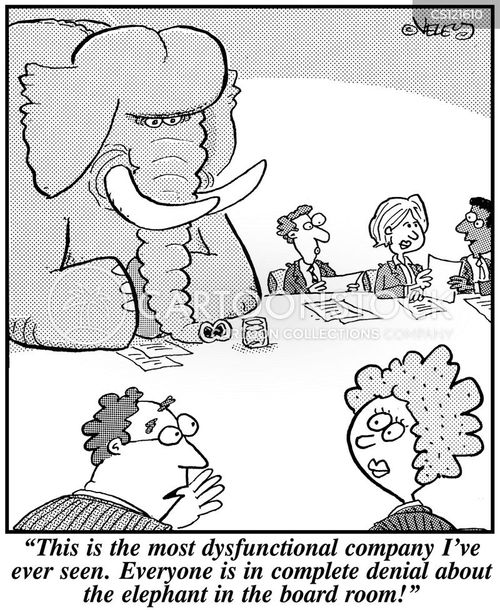
Cartoon – The Most Dysfunctional Company
Despite a meeting between President Donald Trump and various members of Congress, officials have not come to an agreement to end the partial government shutdown, which began Dec. 22. While the majority of the federal government’s public health efforts are continuing as usual, several agencies, including the FDA, are at a loss for funding as long as the temporary closure is in place, Kaiser Health News reports.
Here are five things to know:
1. Congress has already passed five major appropriations bills, which were responsible for funding roughly 75 percent of the federal government, including HHS and the U.S. Department of Veterans Affairs. However, seven bills are still outstanding, including bills funding the Interior, Agriculture and Justice departments, the report states.
2. While the government’s flagship programs, like Medicare, Medicaid and the ACA, are insulated from the effects of the shutdown, other public health agencies are beginning to feel the squeeze from narrowing funding streams. For example, the FDA’s food safety operations are funded through the Department of Agriculture, which has been affected by the shutdown. The FDA’s contingency plan states that in the event of a shutdown, roughly 40 percent of the the agency’s workforce is furloughed.
3. Funding for the Indian Health Service — which is funded by the Department of the Interior — has also not been approved, meaning that the only IHS’ services currently available are those that meet the “immediate needs of the patients, medical staff, and medical facilities,” according to the agency’s contingency plan cited by Kaiser Health News. Many IHS facilities across the country remain open, with staffers reporting to work because they are necessary employees and “excepted” from the furlough, an agency spokesperson told the publication.
4. The Department of Homeland Security’s Office of Health Affairs has also been scaling back its resources to survey threats posed by infectious diseases, pandemics, and biological and chemical attacks, the report states.
5. Roughly 800,000 federal employees nationwide have been affected by the shutdown and have found themselves in financial uncertainty, a New York City-based New York University professor told CNBC. One IRS employee told CNBC he cannot afford his more than $200 insulin prescription because he doesn’t know when he will begin work again.

Toby Cosgrove, MD, former CEO of Cleveland Clinic, told CNBC he foresees 2019 as the year telehealth becomes ubiquitous.
Although telehealth has already permeated the healthcare space, many patients don’t know it exists, Dr. Cosgrove said. However, as awareness grows, patients are increasingly becoming interested in using video conferencing with their physician as a way to save a trip to a hospital. Telehealth also helps patients with chronic conditions, who may need regular monitoring.
“[Oakland, Calif.-based Kaiser Permanente] is seeing over 50 percent of their patients distantly,” Dr. Cosgrove told CNBC.
Dr. Cosgrove, who now serves as an executive advisor to Google Cloud’s healthcare and life sciences team, also said the cloud will serve as a way to make the tremendous amount of data available in healthcare actionable.
“There’s an enormous amount of data and it’s a problem for us to keep track of and that’s why I think the cloud is going to come in,” he said, noting data can be stored and analyzed in the cloud. “So now you can have huge data sets that you can begin to analyze, and now that’s where [artificial intelligence] and machine learning comes in.”
“As the data goes to the cloud all the major cloud providers have come to an agreement that they will share unidentified information,” he added.
Hospital executives quit on the spot. Corporate giants took healthcare into their own hands. Flu hit the country hard. Nurses wanted to cut ties with Facebook. These and four other events and trends shaped the year in healthcare — and the lessons executives can take from them into 2019.
Flu-related deaths hit 40-year high
Roughly 80,000 Americans died of flu and related complications last winter, according to the CDC, along with a record-breaking estimate of 900,000 hospitalizations. That made 2017-18 the deadliest flu season since 1976, the date of the first published paper reporting total seasonal flu deaths, according to the CDC’s Kristen Nordlund.
The milestone flu season reflected a couple of trends. No. 1: Fee-for-service remains the dominant payment model in healthcare. Flu-related hospitalizations triggered financial gains for health systems and hospital networks. No. 2: A deadly flu season gave more weight to concerns about a flu pandemic, which weighs heavily on the minds of CDC Director Robert Redfield, MD, and Bill Gates, among others.
JP Morgan-Berkshire Hathaway-Amazon rocks healthcare
Not even one month into 2018, three corporate giants combined forces to lower healthcare costs for 1.2 million workers. Since the Jan. 30 announcement, Amazon, Berkshire Hathaway and JPMorgan Chase made several important hires: Surgeon, writer and policy wonk Atul Gawande, MD, started work as CEO of the health venture July 9. Soon after, Jack Stoddard, general manager for digital health at Comcast Corp., was appointed COO. More questions than answers remain about this corporate healthcare disruption, including how extensively the new entrants will redesign healthcare for their employees and how much they will collaborate with traditional healthcare providers.
While Dr. Gawande and Mr. Stoddard continue to build their healthcare-centric team to pursue an ambitious mission, remarks from a member of the old guard illustrate the frustration fueling these corporate giants’ foray into healthcare. “A lot of the medical care we do deliver is wrong — so expensive and wrong,” Charlie Munger, vice chairman of Berkshire Hathaway, said in a May interview with CNBC. “It’s ridiculous. A lot of our medical providers are artificially prolonging death so they can make more money.”
While someone briefed on the undertaking said the alliance does not plan to replace existing health insurers or hospitals, it will be fascinating to see how this partnership forces legacy providers to behave differently. Chief executives Jamie Dimon, Warren Buffett and Jeff Bezos are clearly dissatisfied with the way their employees’ healthcare has been accessed, delivered and priced to date.
Sudden executive resignations
The practice of two-week notice became less standard for hospital and health system leaders this year — especially CEOs. Becker’s covers roughly 100 executive moves per month, and the rate at which we wrote about executives abruptly leaving their hospitals in 2018 stood out from the norm. Executives normally provide ample notice of their departure from an organization, much more than the baseline of two weeks that’s expected for any industry or occupation. But in 2018 many more executives resigned immediately, withholding explanation for their sudden departure or bound by non-disclosures to keep it confidential. For the first time, we began publishing round-ups of executives who departed with little notice. Two months into the year, we had nearly a dozen to report.
Healthcare consistently has a high executive turnover rate — 18 percent in 2017. But 2018 was a year in which leadership churn became even more volatile with the swift and mysterious nature of executive exits. The uptick in unexplained resignations occurred during the #MeToo movement, but we don’t have the right information to draw any correlation between them. The frequency of “effective immediately” resignations will normalize this practice if it persists in 2019, which could prove detrimental to hospitals for a host of reasons. Transparency is important in healthcare; highly paid executives quietly walking away from their posts does not bode well for community affairs or physician engagement. It goes back to a lesson from media relations 101: “No comment” is the worst comment.
Health system-backed drug company receives warm welcome
Several leading health systems kicked off 2018 by uniting to create a nonprofit, independent, generic drug company named Civica Rx to fight high drug prices and chronic shortages. The pharmaceutical entrant — backed by Intermountain Healthcare, HCA Healthcare, Mayo Clinic, Catholic Health Initiatives, Providence St. Joseph Health, SSM Health and Trinity Health — is led by CEO Martin Van Trieste, former chief quality officer for biotech giant Amgen. The company’s focus will be a group of 14 generic drugs, administered to patients in hospitals, that have been in short supply and increasingly expensive in recent years. The consortium has declined to name the drugs in development, but said it expects to have its first products on the market as early as 2019.
Intermountain CEO Marc Harrison, MD, exercised measure when describing the new drug company’s mission, noting that responsible pharmaceutical companies will fair fine, but those that have been unprincipled in the past with price increases or supply issues should watch out. Civica Rx may be starting with 14 drugs, but it has noted that there are nearly 200 generics it considers essential that have experienced shortages and price hikes.
Based on reactions from providers and on The Hill, the potential for Civica Rx to quickly gain participants and policy advocates seems rich. For instance, even before Civica Rx applied to the FDA for permission to manufacture drugs, the idea of the company caught hospitals’ interest nationwide. Dr. Harrison said approximately 120 healthcare companies — representing about one-third of hospitals in the U.S. — contacted Civica Rx organizers with interest in participating. Furthermore, lawmakers and regulators were quick to throw support behind the venture even though Congress has done little to get drug pricing under control. Dr. Harrison noted to Modern Healthcare that, as of November 2018, the collaborative “received tremendous bipartisan encouragement from elected officials and from regulatory agencies to continue with our efforts.”
Guns and shootings cemented as a healthcare issue
Gun violence was never outside the realm of health and wellness, but in 2018 the medical community passionately declared the issue as one within their jurisdiction. When the National Rifle Association tweeted Nov. 7 that “Someone should tell self-important anti-gun doctors to stay in their lane,” physicians were quick to respond with detailed, graphic stories and images of their encounters treating the aftermath of gun violence. The #ThisIsOurLane social media movement coincided with tragedy Nov. 19, when a man fatally shot a physician, pharmacist and police officer in Mercy Hospital in Chicago.
With the right resources, clinicians can become ardent advocates to better patients’ social determinants of health, including responsible gun ownership and use. Leavitt Partners released poll findings in spring 2018 in which physicians said they see how social determinants influence patients’ well-being, but do not yet have the resources to help with things like housing, hunger, transportation and securing health insurance. If the fervor of #ThisIsOurLane — and attention paid to it — is any indication, physicians deeply care about nonmedical issues that affect patients’ health. With the right resources, the medical community stands to become a powerful catalyst for change for a broad range of issues.
If health systems are serious about success under value-based payment models, they will empower clinicians with the support, partnerships and tools needed to intervene and improve social determinants of health for the good of their patients.
Media coverage of surprise billing
In late 2017, the American Hospital Association released an advisory notice encouraging members to prepare for a yearlong media investigation into healthcare pricing, conducted by Vox Media Senior Correspondent Sarah Kliff. The AHA’s memo illustrated how poorly prepared hospital executives and media teams are in fielding questions about pricing, especially facility fees.
“When I have tried to conduct interviews with hospital executives about how they set their prices, I find that many are reluctant to comment,” Ms. Kliff wrote. By the end of her 15-month project, Ms. Kliff had read 1,182 ER bills from every state and wrote a dozen articles about individual patient’s financial experiences with hospitals (she was also on maternity leave from June through September). Her work produced some effective headlines. Case in point: “A baby was treated with a nap and a bottle of formula. His parents received an $18,000 bill.” In that case, the hospital reversed the family’s $15,666 trauma fee after Ms. Kliff published her report.
As of Jan. 1, Medicare requires hospitals to disclose prices publicly — but this change is unlikely to greatly benefit patients and consumers since list prices don’t reflect what insurers, government programs and patients pay. Furthermore, price transparency is but one of the problems Ms. Kliff encountered in her extensive reporting. Others include high prices for generic drug store items ($238 for eye drops that run $15 to $50 in a retail pharmacy), out-of-network physicians tending to patients who are visiting in-network hospitals, and ER facility fees. Hospitals reversed $45,107 in medical bills as a result of Ms. Kliff’s reporting. Based on the change spearheaded by her work and the Congressional attention paid to medical billing practices, hospitals and health systems shouldn’t quit their AHA-advised preparation on their own billing practices just yet. They also shouldn’t chalk much progress up to CMS-mandated price postings, because that information does not answer the questions Ms. Kliff set out to answer, including how hospital set their prices. There will only be more questions like this — from journalists, patients and lawmakers.
Optum ‘scaring the crap out of hospitals‘
Which business is keeping hospital leaders up at night? Many executives will tell you it’s not Amazon, not CVS, not One Medical — but Optum, the provider services arm of UnitedHealth Group. Optum was a key driver of the 11.7 percent gain UnitedHealth Group’s stock saw in 2018, which made it one of the top performers in the Dow Jones Industrial Average, according to Barron’s. Through its OptumCare branch, Optum employs or is affiliated with more than 30,000 physicians — roughly 8,000 more than Oakland, Calif.-based Kaiser Permanente.
Aside from directly competing for patients, Optum wants to hire or affiliate with the same MD-certified talent. It offers physicians three ways to do so: direct employment, network affiliation or practice acquisition. “OptumCare Medical Group offers recent medical school graduates the opportunity to practice medicine and become a valuable partner in their local community minus the hassles associated with the ever-changing business side of healthcare,” the company writes on its employment website.
It’s not just the physician force that makes Optum a serious concern for hospitals. Part of the challenge is that the $91 billion business has a hand in several healthcare buckets, expanding its presence as either a serious competitor/threat or a potential collaborator in multiple arenas since it is not easily categorized. For instance, consider the mountain of data Optum sits upon, with valuable insights related to utilization, costs and patient behaviors. “Because they are connected to UnitedHealth, they probably have more healthcare data than anyone on the planet,” the CEO of a $2.5 billion health system said.
Mark Zuckerberg lost face with nurses
For as much as we talk about the collision of Silicon Valley and healthcare, one of the year’s most vivid clashes came down to a dozen California nurses and Mark Zuckerberg, the chairman and CEO of Facebook and world’s third-richest person. San Francisco General Hospital and Trauma Center was renamed the Priscilla Chan and Mark Zuckerberg San Francisco General Hospital and Trauma Center in 2015 after Mr. Zuckerberg and his wife, Priscilla Chan, MD, gave $75 million to the organization.
Soon after the Facebook-Cambridge Analytica ordeal came to light, a dozen nurses protested and demanded Mr. Zuckerberg’s name be stripped from their hospital. His name is hardly synonymous with the protection of privacy, they argued. But philanthropy proves to be more of an art than a science. By November, even as a San Francisco politician pressed for the removal of the name, hospital CEO Susan Ehrlich, MD, said: “We are honored that Dr. Chan and Mr. Zuckerberg thought highly enough of our hospital and staff, and the health of San Franciscans, to donate their resources to our mission.”
The dispute illustrates the tension hospital and health system executives must deal with as cash-rich tech giants and venture capitalists make more high-profile forays into healthcare. Hospitals can use the cash, sure, but the alignment of value systems may present some challenges. 2018 was a year in which several tech companies faced problems with transparency, holding leaders publicly accountable, and diversity in hiring, among other issues. A dozen nurses protesting their hospital sharing a name with Mark Zuckerberg? That’s not the last time we’ll see clinicians urging wealthy but problematic tech icons to back off. Hospital executives will need to be adept in handling that tension and exercise urgency in their response.

A sizable percentage of Americans between the ages of 50 and 64 are worried about their healthcare coverage as they head toward retirement, according to a new poll from the University of Michigan.
Although some of these concerns include things people can’t directly control, such as policy changes, many are focused on maintaining current coverage provided through an employer while reducing personal healthcare expenses.
“The ACA’s insurance coverage expansion was intended, in part, to reduce ‘job lock’ and allow individuals to change or leave their job without concern about becoming uninsured,” the report says. “However, data from this poll suggest that many adults age 50–64 still worry about maintaining employer-sponsored health insurance and keeping a job for that reason.”
About a quarter (27%) of respondents fear they won’t be able to afford their insurance over the next year, and nearly half (45%) expressed little to no confidence in being able to afford their insurance when they retire.
Meanwhile, 13% of those surveyed postponed medical care within the last year due to cost concerns. Another 15% postponed procedures until they could change their plan the following coverage year—so it would be covered, to incur lower out-of-pocket costs or to see a specific doctor in-network. Additionally, 8% of respondents between the ages of 60 and 64 reported delaying a procedure until they could get Medicare.
Nearly 1 in 5 (19%) said they were keeping a job, delaying retirement or considering delaying retirement to keep their employer-sponsored insurance. With that in mind, 71% of retirees were confident in their ability to afford insurance—a much higher percentage than those who were working (54%) or not working (49%).
Men were more confident than women that they could afford insurance at retirement (61% vs. 50%). Those in “excellent” health were more confident than those in “good” or “fair/poor” health (62% vs. 54% and 42%), as were those with a college degree compared to those without.
Nearly 8 in 10 respondents (79%) said they were very confident in their ability to navigate the health insurance landscape, though about 3 in 10 (29%) indicated little or no confidence that they could determine the out-of-pocket costs associated with a prospective service.
The study indicates Americans are closely watching and responding to challenges to the Affordable Care Act, such as a ruling by a federal judge in Texas striking down the law. Over the weekend, the judge issued a stay on the ruling, saying the healthcare law should remain in effect as appeals weave their way through the courts.
Half of those surveyed said they closely follow news about the ACA, Medicare or Medicaid, and 68% said they are worried about how their coverage may change due to federal policies.
“Regardless of potential federal policy changes, patients and their health care providers should discuss the out-of-pocket costs of health care, such as medical procedures, tests, or medications. Such discussions can help inform decisions about their health insurance options and the timing, choice, and appropriateness of health care services,” it concluded.

If 2018 was about who was getting jobs, 2019 may be about how jobs work. Indeed, this may be the year that organizations start retooling how they find, evaluate, and even pay employees. Chalk the shifts up to, among several factors, the tight labor market and a massive influx of data, says Jeanne MacDonald, global co-operating executive and president of global talent solutions for Korn Ferry’s RPO and Professional Search business. “To succeed in attracting, developing, and retaining top talent as we head into another year, it’s critical to be agile and forward thinking,” she says.
Korn Ferry canvassed talent acquisition specialists, compensation experts, and HR professionals from around the world to identify 10 emerging talent trends in 2019.
(Don’t) Mind the Gap!
It has always been a red flag—the “hole” in a candidate’s resume, a period of time where a candidate wasn’t working. But an increasing number of organizations are realizing that those holes are there for very legitimate reasons, such as taking time off to care for children or aging loved ones. Many firms are now actively seeking out people with these types of gaps, MacDonald says. Firms are using workshops, customized landing pages and microsites, and other means to find these people.
Making Artificial Intelligence More “Intelligent”
Artificial intelligence (AI) has been touted as the new holy grail in recruiting. However, experts worry that its “intelligence” could create a lack of focus on diversity and inclusion. Even when resumes are anonymized by removing candidate names, AI often can figure out a candidate’s gender by analyzing the phrases used. For instance, “takes charge” and “tough task master” are often associated with men, while “leads persuasively” and “committed to understanding” are often used by women.
One way to help alleviate the issue is to feed the artificial intelligence with non-partial data, such as talent assessment data, that highlights success factors. The AI also needs to be trained to look more for the skills needed for a specific role instead of focusing on subjective modifiers, says George Vollmer, Korn Ferry’s vice president of global account development.
Personalized Pay: Go Ahead, We’re Listening
There are four generations now in the workforce, each with different expectations when it comes to pay and rewards packages. Forward-thinking firms are using social listening, focus groups, and surveys to figure out what each generation actually wants. With that information, they are able to tailor rewards packages, offering different mixes of pay, flextime, paid time off, international assignments, student loan repayment, and other benefits. This is turning the pay and rewards discussion from a company talking to the entire employee population to a one-to-one discussion with employees.
Rethinking the Annual Performance Review
In the United States, the average job tenure is a little more than four years. Experts say that with such short tenures, annual reviews are no longer the primary way to help employees develop professionally. Many employees already recognize this. In a recent Korn Ferry survey of professionals, 30% said their annual review had no impact or was ineffective at improving their performance, and 43% said it had no impact or was unhelpful at making them understand what to do to improve future performance.
Firms are starting to consider real-time feedback as, at a minimum, a supplement to annual reviews, if not a substitute. Ongoing feedback can help employees learn and stay engaged.
Digging Deeper into the Diversity and Inclusion Pipeline
Around the world, there have been growing mandates for more women on boards and other senior leadership positions. While that’s a good development, firms need to maintain focus across all levels of an organization to create an ongoing pipeline of diverse talent, including women, people of color, disabled persons, and LGBTQ employees. To measure their progress, many organizations have begun using applicant tracking systems to find out what percentage of minority applicants were hired.
How Are We Doing?
For years, consumer product companies and retailers have been surveying customers about their experiences with the brand. Increasingly, that practice is becoming part of the recruiting process. Technology is allowing for real-time feedback from candidates about their experiences during the recruiting cycle. The survey tools seek feedback at all points within the process, which gives recruiters and hiring managers data-driven insights and intelligence.
With the data, they can amend recruiting practices, including specific job requirements and interactions with candidates, to successfully hire the best people.
That’s Really a Title?
Chief happiness officer. Data wrangler. Legal ninja. They may sound like off-the-wall job titles, but roles like these are emerging across many industries to meet the changing strategies of organizations.
For example, healthcare, finance, and other firms are increasingly looking to hire a chief experience officer. These businesses realize that the need is stronger than ever for customers to have positive experiences at every touchpoint, MacDonald says. Another emerging C-suite role is chief transformation officer, who is usually tasked with change-management initiatives, often during times of mergers and acquisitions.
Some names are also popping up to attract younger employees. For instance, data wranglers are responsible for organizing and interpreting mounds of data, and legal ninjas are the new generation of legal aides.
Talent Analytics Is Becoming Just as Important as Business Analytics
Traditionally, business leaders set their strategy by analyzing business analytics to determine cost and operational effectiveness. However, experts say they may fail because they don’t find the right type of talent. Increasingly, firms are incorporating talent analytics into the mix. This data measures things such as competition for qualified talent in a region and compensation norms.
Talking Talent Holistically, From Hire to Retire
With the massive influx of data, one would assume organizations would have an integrated way to analyze all elements of talent decisions, including recruiting, compensation, and development. Unfortunately, in many organizations, each of these functions is operating under a different “language,” often unable to talk with one another.
Experts say there is a trend toward a more foundational, data-centric approach that creates insights from organizational, team, and individual perspectives. That allows for a calibrated approach to talent that is tightly linked to business outcomes. For example, the data garnered during the recruitment process can be used to help create a customized development program once the candidate is hired.
Managing Short-Term Hiring Needs with Long-Term Business Goals
The speed of technological advances and changing business priorities makes knowing what’s going to happen next year—or even next month—extremely difficult. In fact, in a recent Korn Ferry survey of talent acquisition professionals, 77% say they are hiring for roles today that didn’t even exist a year ago.
Leading organizations are taking a holistic approach to talent acquisition. In the short term, they are speeding up hiring by figuring out the right mix of short-term contractors, gig workers, and full-time employees to do the work that currently needs to be done. At the same time, they are focusing on a longer-term approach by taking a deep dive into business imperatives to create a total strategic plan that has clearly defined goals, but one that can be amended as needs change.