http://www.healthcaredive.com/news/the-hospital-divestiture-trend-is-heating-up-and-not-going-away-anytime-so/505566/

Not long ago, health systems gobbled up hospitals with the overriding goal of growth, expanded footprints and market share. Some major health systems are now regretting those buys as they have become saddled with community hospitals that are losing money and struggling with large debt and capital needs.
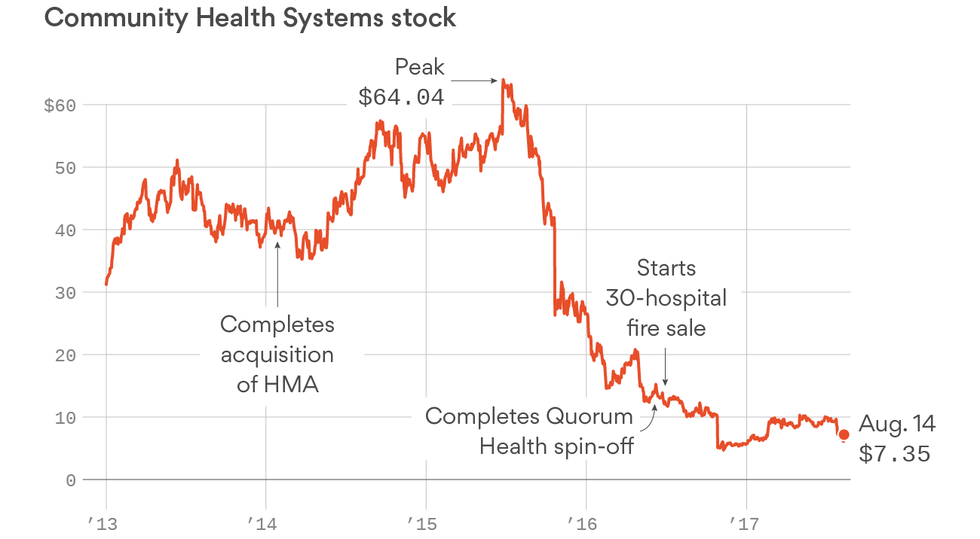
Two major health systems facing this issue are Community Health Systems (CHS) and Tenet Healthcare, who are both looking to shed facilities.
“The strategy that CHS, Tenet and many others had was to really build around scale without really thinking about the regional economics of how these hospitals work together,” Gregory Hagood, senior managing director at SOLIC Capital Advisors, which works with hospitals on mergers and acquisitions, told Healthcare Dive.
Health systems like CHS and Tenet grew their systems with large purchases, but they’ve learned from their experiences and are now looking at divestiture options as a way to shed unprofitable hospitals and billions of debt. No longer are major systems and investors interested in buying struggling hospitals, which CHS did when it purchased the struggling Florida system Health Management Associates for $7.5 billion in 2014.
CHS and Tenet look to cut facilities, debt
CHS, a for-profit system with 137 hospitals in 21 states, is looking to divest at least 30 hospitals this year. They have already announced more than 20 hospital sales this year. CHS’ divestitures come after the health system lost $1.7 billion last year and accumulated about $15 billion in debt. Given their financial situation, Moody’s Investors Service recently downgraded CHS’ corporate family rating, probability of default rating and senior unsecured notes.
Meanwhile, Tenet Healthcare, the third largest investor-owned U.S. health system, is looking into strategic business options that may include a sale. The Wall Street Journal estimated Tenet has a market value of $1.6 billion, which is a far cry from what it owes. Fitch Ratings reported that Tenet had about $15.4 billion of debt at the end of June.
Tenet recently announced it’s selling eight U.S. hospitals and all of its nine U.K. facilities, which CEO Trevor Fetter said will yield between $900 million and $1 billion.
In addition to the sales, the company is dealing with executive and board shake-ups. Fetter recently announced his impending departure and two board members left the board because of “irreconcilable differences regarding significant matters impacting Tenet and its stakeholders.”
CHS and Tenet might be the most high-profile systems looking to shed debt and facilities, but they’re far from the only ones. A recent report by Kaufman Hall found that hospital and health systems mergers and acquisitions increased 15% in Q2. Big players are especially active. There were six transactions of health systems with nearly $1 billion or more in revenues announced in the first half of 2017. There were only four such deals in all of 2016.
Though hospital M&A activity remains high, healthcare financial experts say the days of health systems swallowing small, unprofitable hospitals as part of larger deals to solely build a system’s footprint are gone. Those days have been replaced by more strategic decisions as to what is right for the organizations, Richard Gundling, senior vice president of healthcare financial practices at the Healthcare Financial Management Association, told Healthcare Dive.
Health systems are now taking a strategic view of hospitals to see if they fit into their culture. They are also ignoring small, community hospitals with debt or buying them for much less than they may be worth.
The systems that are selling unprofitable hospitals are also faced with a market in which investors aren’t interested in paying top dollar for struggling hospitals with heavy debt. Instead, Hagood said, investors are more interested in post-acute care services like rehab and long-term care and ambulatory care initiatives. They don’t typically see hospitals as a wise investment.
“Smaller systems that have huge debt loads or pent-up capital demands have received a lukewarm reception at best,” Patrick Allen, managing director with Kaufman Hall’s mergers and acquisitions practice, told Healthcare Dive.
Why are health systems divesting?
Health systems, especially ones that have built up debt, are having trouble making up lost revenues. Hospitals could once cover a struggling type of care through a different, more profitable service. That’s no longer the case as payers and the CMS have squeezed hospital margins.
Sagging reimbursements and payer policies that move patients from hospitals to outpatient care and freestanding facilities are hurting hospital finances. There’s also a CMS proposal to allow hip and knee replacement surgeries for Medicare patients on an outpatient basis. Those kinds of surgeries are often the most profitable for hospitals, which means they may soon lose another revenue driver.
Beyond those direct payer impacts, health systems are looking to protect themselves against a changing industry in which market share isn’t as important as flexibility and efficiency. “As all of these changes are occurring, the systems are strategically moving and gathering their assets to be able to deal with expected changes,” Gundling said.
Gundling said another issue facing large systems that may lead to divestiture is cultural mismatch. A large system may have swooped in and bought a 100- or 150-bed community hospital as part of a larger purchase. The hospital’s community may have bristled at the idea of a large out-of-state corporate entity buying a mainstay of their community. Plus, physicians may dislike a new system’s clinical protocols.
“There might be times when you say it might not be the right fit for us after all … That can lead to a divestiture decision,” Gundling said.
How are health systems handling divestitures?
Health systems are taking different avenues to deal with possible divestitures. Some systems want to completely rid themselves of certain hospitals. Others look to repurpose small hospitals for outpatient, skilled nursing facilities, labs or imaging while maintaining a large regional hospital. Still others forge partnerships, so they don’t completely sell the properties.
Allen said many health systems see their small community hospitals aren’t bringing in enough revenue and can’t be competitive in every service line and business. So, instead, they are dropping unprofitable services and sticking with what works for them.
Gundling compared health systems’ decisions about divestiture to an individual creating the right investment balance. For health systems, divestitures are not about selling properties, but strategically managing risk. “They aren’t just selling off to sell off. All have different strategies,” said Gundling.
Allen said divestitures are a balancing act for systems. They can shed debt and assets, but that comes with revenue loss. “The balance is always what is the right sale price for the exchange of cash flow when it becomes less than profitable. Balancing those two are always tough,” said Allen.
When deciding on whether to divest, merge or partner with other facilities, Allen said systems need to figure out the community’s needs, the area’s business climate, what the facility wants to be and potential partnership opportunities. Allen, whose company works mostly with nonprofit systems, said many are repurposing underutilized facilities into other uses like rehab, skilled nursing facilities, labs and imaging.
“Once you have a handle on what the market needs and what the market provides, then you can make strategies to get you there,” he said.
Another issue facing health systems is infrastructure. Many smaller hospitals don’t meet today’s care delivery system. “A lot of hospitals don’t lend themselves very efficiently to quality care based on their 30- and 40-year old design,” said Hagood. “That factor can accelerate their repurposing.”
The results and future of the divestiture trend
Allen said divestitures have resulted in systems being able to reallocate capital and move forward with less debt. However, Hagood said one major reason health systems have for divestitures — shedding debt — hasn’t completely worked. Part of the problem is that the new investors aren’t paying top dollar for a struggling community hospital with debt.
“The biggest challenge so far is that they have struggled to get value for those assets to effectively repay that debt,” he said.
Gundling said health systems that have shed debt have followed the divestitures by focusing on cost efficiencies, supply chain management and revenue cycle management.
The hospital divestiture trend has led to sales, mergers and partnerships, with repurposed or downsized facilities, but it hasn’t closed many facilities. That may be coming soon, though.
Hagood said pending mergers, including the Mountain States Health Alliance and Wellmont Health System deal in Tennessee and Virginia, will likely lead to facility closures. There aren’t enough healthcare dollars to support the number of facilities in some of the Appalachian communities involved, he said.
Most of the large divestiture action has been centered around for-profit systems, but Hagood said to watch for more nonprofit action, including Catholic Health Initiatives (CHI), which recently reported a $585.2 million operating loss for fiscal year 2017 after losing $371.4 million in 2016.
Earlier this year, Moody’s Investor Service downgraded CHI’s rating on long-term debt and variable rate demand bonds because of poor operating performance since 2012 and a relatively low level of liquid assets. Moody’s warned that further downgrades could occur unless CHI improves its operating performance.
CHI divested its KentuckyOne facilities earlier this year, a move expected to bring in $534.9 million. Given the company’s finances and healthcare environment, Hagood said there could be more divestitures.
“Nonprofits are going to move slower, but I think you’re going to see them (divest) as economics continue to shift,” he said.
Experts agree the divestiture trend is just heating up as health systems deal with the greater emphasis on outpatient care and freestanding centers. Hagood predicted 24-7 inpatient facilities with full emergency rooms and surgical facilities will continue to dwindle in the coming years as systems repurpose facilities.
“There are 5,000-plus hospitals today. I think you’re going to see that consolidate down,” he said.