https://www.politico.com/story/2017/12/08/susan-collins-obamacare-deal-213254

House conservatives thumb their nose at the Maine moderate’s bid to slow the demise of the health law.
Sen. Susan Collins is barreling toward yet another health care showdown with her own party. But this time, she might not have the leverage to get what she wants.
Republicans who watched Collins lead the rebellion over the GOP’s Obamacare repeal effort just three months ago are playing tough on yet another high-stakes bill, wagering they can do without the Maine moderate’s swing vote and still claim a narrow year-end legislative win on tax reform.
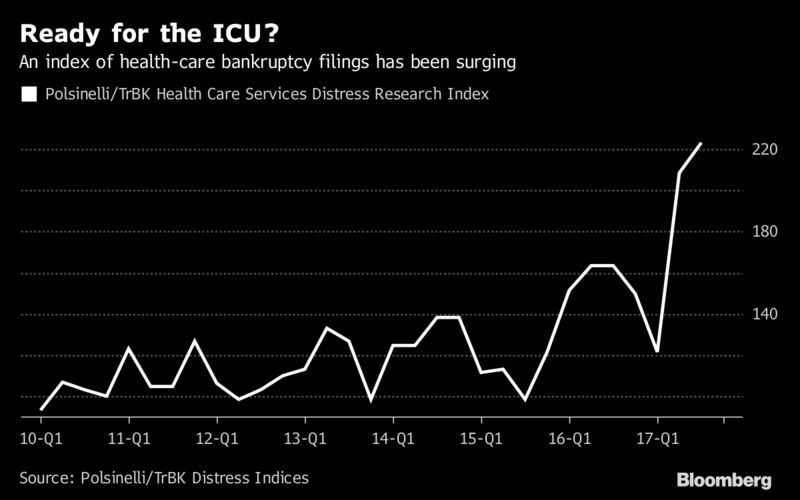
Collins went along with the tax bill that repeals Obamacare’s individual mandate after Senate Majority Leader Mitch McConnell pledged to pass a pair of bills propping up Obamacare’s shaky insurance markets, including a bipartisan deal resuming payments on key subsidies that President Donald Trump halted in October.
But Speaker Paul Ryan has made clear he’s not bound by the deal, and there’s little urgency among House Republicans to do much of anything on health care before the end of the year. On Thursday, Republican Study Committee Chairman Mark Walker said conservatives received assurances that talks on a spending package to keep the government open won’t address Obamacare.
“The three things we were told are not gonna happen as part of our agreement: no CSRs, no DACA, no debt limit,” he said, referring to efforts to fund Obamacare’s cost-sharing subsidies.
That could cost Collins’ support after she signaled that her vote on the final bill may hinge on the fate of the health care measures.
She told a Maine CBS affiliate Thursday night that she’d wait to see the final language from the conference committee working on the tax bill before committing her vote.
“I won’t make a final decision until I see what that package is,” Collins told CBS WABI 5.
One bill, known as Alexander-Murray, would temporarily restore subsidies to insurers. The second would fund a two-year reinsurance program helping health plans cover particularly expensive patients.
Senate Republicans can only afford two defections and still pass the tax bill using a fast-track procedure that requires a simple majority, with Vice President Mike Pence ready to cast the tie-breaking vote. The margin would become razor thin if Collins holds out, and Sen. Bob Corker maintains his opposition over concerns about the bill’s impact on the deficit.
Yet House Republicans still chafing over the Senate’s failure to repeal Obamacare insist they won’t bend to Collins’ demands. And while Senate Republicans are trying to keep Collins in the fold, there’s little apparent worry so far that her opposition would sink the tax effort.
“I think you guys have to find something else to be concerned about,” said Sen. Tim Scott, one of the 17 GOP lawmakers assigned to merge the House and Senate versions of the tax plan.
Sen. Lamar Alexander, who coauthored Alexander-Murray and has championed its inclusion in a year-end agreement, also waved off the need to pressure House Republicans on the issue.
“The House knows our position,” he said. “When they see that they can lower premiums 18 percent … reduce the debt, reduce the amount of money going to Obamacare subsidies, I think it’ll be a Christmas present they’ll want to give to their constituents.”
One of the few moderates in a Republican conference that narrowly controls the Senate, Collins has regularly used her voice and vote to extract concessions from GOP leaders and ensure she’s a central figure in negotiations.
During the health care debate, she urged the GOP to protect Medicaid and preserve more subsidies for people to buy insurance. When they stuck with their blueprint, Collins joined fellow Republicans Lisa Murkowski and John McCain in a dramatic vote that killed the months-long repeal bid.
And in the run-up to the Senate’s late-night tax vote, she secured three late changes to the bill, including the expansion of a provision allowing people to deduct hefty medical bills that House Republicans had voted to eliminate entirely.
That was on top of McConnell’s “ironclad commitment” to tackle the two health care bills at year’s end — measures that Collins claims will help offset premium increases stemming from the bill’s repeal of Obamacare’s mandate that most Americans be insured.
Collins said Thursday she considers House passage of those Obamacare bills part of that commitment, even though McConnell has only publicly agreed to “supporting passage” of them and can’t singlehandedly force the House to take up legislation.
Ryan hasn’t officially ruled out the possibility, but declined to commit to rolling either of the bills into upcoming spending agreements. Conservatives have loudly opposed any aid for Obamacare, and even moderates who support stabilizing the health law have shrugged at the exact timing.
“What the vehicle is to get it through the system, in the House and the Senate to the president’s desk, I’ll leave that to our leadership,” said Rep. Tom Reed, who co-chairs the bipartisan Problem Solvers Caucus.
Collins insists she’s taking the long view, claiming progress Thursday on trying to win over House Republicans during rounds of private negotiations.
“I remain confident, despite your skepticism, that we will eventually get that,” she said.
And as the GOP learned during the repeal debate, the whip count could shift suddenly. Sens. Jeff Flake and Ron Johnson remain wild cards, and either could conceivably join Corker and Collins in torpedoing the tax bill if they dislike the final version.
For now though, Republican leaders are signaling once again that Collins may not get everything she wants on health care — and gambling it won’t cost them a second time.
“I think that these are separate issues,” said Sen. David Perdue. “I’m hopeful that that won’t derail this [tax bill]. We’ve got to get it this done and get it on the president’s desk.”