Category Archives: Public Health
Cartoon – Sign of the Times (Dining Indoors)

We look at the need to accelerate the U.S. vaccination program.

| Three million shots a day |
| The Biden administration has been quite cautious in setting its public vaccination goals. |
| During the transition, officials said they hoped to give shots to one million Americans per day — a level the Trump administration nearly reached in its final days, despite being badly behind its own goals. In President Biden’s first week in office, he raised the target to 1.5 million, although his aides quickly added that it was more of a “hope” than a “goal.” Either way, the country is now giving about 1.7 million shots per day. |
| I have spent some time recently interviewing public-health experts about what the real goal should be, and I came away with a clear message: The Biden administration is not being ambitious enough about vaccinations, at least not in its public statements. |
| An appropriate goal, experts say, is three million shots per day — probably by April. At that pace, half of adults would receive their first shot by April and all adults who wanted a shot could receive one by June, saving thousands of lives and allowing normal life to return by midsummer. |
| Biden struck a somewhat more ambitious tone yesterday, telling CNN that anybody who wanted a vaccine would be able to get one “by the end of July.” But Dr. Anthony Fauci also said that the timeline for when the general population could receive shots was slipping from April to May or June. |
| The shots are on their way |
| The key fact is that the delivery of vaccine doses is on the verge of accelerating rapidly. Since December, Moderna and Pfizer have delivered fewer than one million shots per day to the government. |
| But over the next month and a half, the two companies have promised to deliver at least three million shots per day — and to accelerate the pace to about 3.3 million per day starting in April. Johnson & Johnson is likely to add to that total if, as expected, it receives the go-ahead to start distributing shots in coming weeks. |
| Very soon, the major issue won’t be supply. It will be logistics: Can the Biden administration and state and local governments administer the shots at close to the same rate that they receive them? |
| “I’m not hearing a plan,” Dr. Peter Hotez, a vaccine expert at Baylor College of Medicine, told me. “In the public statements, I don’t hear that sense of urgency.” |
| Bankers’ hours for vaccine clinics |
| The experts I interviewed said they understood why Biden had set only modest public goals so far. Manufacturing vaccines is complex, and falling short of a high-profile goal would sew doubt during a public-health emergency, as Barry Bloom, a Harvard immunologist, told me. If he were president, Bloom added, he would also want to exceed whatever goal was appearing in the media. |
| But setting aside public relations, experts say that the appropriate goal is to administer vaccine shots at roughly the same rate that drug makers deliver them — with a short delay, of a week or two, for logistics. Otherwise, millions of doses will languish in storage while Americans are dying and the country remains partially shut down. |
| “We should be doing more,” Jennifer Nuzzo, an epidemiologist at Johns Hopkins, said. “I am kind of surprised by how constrained we’ve been.” Many vaccine clinics operate only during business hours, she noted. And the government has not done much to expand the pool of vaccine workers — say, by training E.M.T. workers. |
| The newly contagious variants of the virus add another reason for urgency. They could cause an explosion of cases in the spring, Hotez said, and lead to mutations that are resistant to the current vaccines. But if the vaccines can crush the spread before then, the mutations may not take hold. |
| “We need to be laser focused on getting as many people vaccinated now as possible,” Dr. Paul Sax, a top infectious-disease official at Brigham and Women’s Hospital in Boston, told me. |
| As my colleague Katie Thomas, who covers the vaccines, said: “The future looks bright — if we can do vaccination quickly enough, if people actually want the vaccines and if the variants don’t mess with the plan.” |
| ‘Our historic moment of crisis’ |
| Nobody doubts that vaccinating three million Americans every day for months on end would be a herculean task. |
| When I asked Biden about his virus plan during a December phone call, he used the term “logistical nightmare” to describe a rapid national vaccination program. “This is going to be one of the hardest and most costly challenges in American history,” he said. |
| Since then, his aides have emphasized the challenges — the possibility of manufacturing problems, the difficulty of working with hundreds of local agencies, the need to distribute vaccines equitably. They also point out that they have nearly doubled the pace of vaccination in their first month in office, accelerated the pace of delivery from drugmakers and have plans to do more, like open mass-vaccination clinics and expand the pool of vaccine workers. |
| Part of me wonders whether the White House knows that three million shots per day is the right goal and simply doesn’t want to say so. |
| When Biden and his advisers talk about the fight against Covid-19, they sometimes compare it to wartime mobilization. And the U.S. has accomplished amazing logistical feats during wartime. A single Michigan auto plant figured out how to manufacture a new B-24 bomber plane every hour during World War II, and a network of West Coast factories built one warship per day — for four years. |
| “This is our historic moment of crisis and challenge,” Biden said during his inaugural address. “We have never, ever, ever failed in America when we have acted together.” |
| Near the end of the speech, he added a question: “Will we rise to the occasion?” |
CDC presses for schools to reopen with precautions

The Centers for Disease Control and Prevention (CDC) on Friday released long-awaited guidance on safely reopening schools, emphasizing the importance of having schools open as long as proper safety precautions are followed.
The guidance states it is “critical for schools to open as safely and as soon as possible,” given the benefits of in-person learning.
The top recommendations for doing so safely are universal wearing of masks by students, staff and teachers as well as distancing so that people are six feet apart.
Vaccination of teachers should be prioritized, the agency said, but “should not be considered a condition” of reopening schools.
Schools can adjust whether they are fully in-person or hybrid depending on the level of spread in the surrounding community and mitigation measures in place.
Schools are encouraged to use “podding” to separate students into smaller groups to help make contract tracing easier.
The pandemic’s coming new normal

As both vaccinations and acquired immunity spread, life will likely settle into a new normal that will resemble pre-COVID-19 days— with some major twists.
The big picture: While hospitalizations and deaths are tamped down, the novel coronavirus should recede as a mortal threat to the world. But a lingering pool of unvaccinated people — and the virus’ own ability to mutate — will ensure SARS-CoV-2 keeps circulating at some level, meaning some precautions will be kept in place for years.
Driving the news: On Tuesday, Johnson & Johnson CEO Alex Gorsky told CNBC that people might well need a new coronavirus vaccine annually in the years ahead, much as they do now for the flu.
- Gorsky’s comments were one of the clearest signals that even as the number of vaccinated people rises, the mutability of SARS-CoV-2 means the virus will almost certainly be with us in some form for years to come.
Be smart: That sounds like bad news — and indeed, it’s much less ideal than a world in which vaccination or infection conferred close to lifelong immunity and SARS-CoV-2 could be definitively conquered like smallpox.
- With more contagious variants spreading rapidly, “the next 12 weeks are likely to be the darkest days of the pandemic,” says Michael Osterholm, the director of the University of Minnesota’s Center for Infectious Disease Research and Policy.
- But the apparent effectiveness of the vaccines in preventing hospitalizations and death from COVID-19 — even in the face of new variants — points the way toward a milder future for the pandemic, albeit one that may be experienced very differently around the world.
Details: From studying what happened after new viruses emerged in the past, scientists predict SARS-CoV-2 will eventually become endemic, most likely in a seasonal pattern similar to the kind of coronaviruses that cause the common cold.
- That’s nothing to sneeze at — literally, it will make us sneeze — but as immunity levels accumulate throughout the population, our experience of the virus will attenuate, and we’ll be highly unlikely to experience the severe death tolls and overloaded hospitals that marked much of the past year.
Yes, but: The existence of a stubborn pool of Americans who say they won’t get vaccinated — as well as the fact that it may take far longer for children, whom the vaccines have yet to be tested on, to get coverage — will give the virus longer legs than it would otherwise have.
- “This will be with us forever,” says Osterholm. “That’s not even a debate at this point.”
What’s next: This means we can expect the K-shaped recovery that has marked the pandemic to continue, says Ben Pring, who leads Cognizant’s Center for the Future of Work.
- With the virus likely to remain a threat, even if a diminished one, “those who are more stuck in the analog world are really going to continue to struggle,” he says.
- Health security will also become a more ingrained part of daily life and work, which means temperature checks, masks, frequent COVID-19 testing and even vaccine passports for travel are here to stay.
The catch: That’s not all bad — the measures put in place to slow COVID-19 have stomped the flu and other seasonal respiratory viruses, and if we can hold onto some of those benefits in the future, we can save tens of thousands of lives and billions of dollars.
- If the inequalities seen in the early phase of the vaccine rollout persist, COVID-19 could become a disease of the poor and disadvantaged, argues Mark Sendak, the co-founder and scientific adviser for Greenlight Ready, a COVID-19 resilience system that grew out of Duke Health.
- Sendak points to the example of HIV, a disease that is entirely controllable with drugs but continues to exert a disproportionate toll on Black Americans, who take pre-exposure prophylactic medicine at much lower rates.
“If we go back to ‘normal,’ then we have failed.”
— Mark Sendak
What to watch: Whether the vaccine rollout can be adapted to reach hard to find and hard to persuade populations.
- The Biden administration announced yesterday that it will start delivering vaccines directly to community health centers next week in an effort to promote more equity in the vaccine distribution process.
- As the administration rolls out new COVID-19 plans, it needs to “invest in the community health care personnel” who can ensure that no one is left behind, says Sendak.
The bottom line: While SARS-CoV-2 has proven it can adapt to a changing environment, so can we. But we have to do so in a way that is fairer than our experience of the pandemic has been so far.
Where the pandemic has been deadliest

In the seven states hit hardest by the pandemic, more than 1 in every 500 residents have died from the coronavirus.
Why it matters: The staggering death toll speaks to America’s failure to control the virus.
Details: In New Jersey, which has the highest death rate in the nation, 1 out of every 406 residents has died from the virus. In neighboring New York, 1 out of every 437 people has died.
- In Mississippi, 1 out of every 477 people has died. And in South Dakota, which was slammed in the fall, 1 of every 489 people has died.
States in the middle of the pack have seen a death rate of around 1 in 800 dead.
- California, which has generally suffered severe regional outbreaks that don’t span the entire state, has a death rate of 1 in 899.
- Vermont had the lowest death rate, at 1 of every 3,436 residents.
The bottom line: Americans will keep dying as vaccinations ramp up, and more transmissible variants of the coronavirus could cause the outbreak to get worse before it gets better.
- Experts also say it’s time to start preparing for the next pandemic — which could be deadlier.
What happens after a year without the flu?
https://mailchi.mp/85f08f5211a4/the-weekly-gist-february-5-2021?e=d1e747d2d8
Doctors and scientists have been relieved that the dreaded “twindemic”—the usual winter spike of seasonal influenza superimposed on the COVID pandemic—did not materialize.
In fact, flu cases are at one of the lowest levels ever recorded, with just 155 flu-related hospitalizations this season (compared to over 490K in 2019). A new piece in the Atlantic looks at the long-term ramifications of a year without the flu.
Public health measures like masking and handwashing have surely lowered flu transmission, but scientists remain uncertain why flu cases have flatlined as COVID-19, which spreads via the same mechanisms, surged.
Children are a much greater vector for influenza, and reduced mingling in schools and childcare likely slowed spread. Perhaps the shutdown in travel slowed the viruses’ ability to hop a ride from continent to continent, and the cancellation of gatherings further dampened transmission.
Nor are scientists sure what to expect next year. Optimists hope that record-low levels of flu could take a strain out of circulation. But others warn that flu could return with a vengeance, as the virus continues to mutate while population immunity declines.
Researchers developing next year’s vaccines, meanwhile, face a lack of data on what strains and mutations to target—although many hope the mRNA technologies that proved effective for COVID will enable more agile flu vaccine development in the future.
Regardless, renewed vigilance in flu prevention and vaccination next fall will be essential, as a COVID-fatigued population will be inclined to breathe a sigh of relief as the current pandemic comes under control.
“I got the vaccine…now what can I do?”
https://mailchi.mp/85f08f5211a4/the-weekly-gist-february-5-2021?e=d1e747d2d8

A family member in her 70s called with the great news that she received her first dose of the COVID vaccine this week. She mentioned that she was hoping to plan a vacation in the spring with a friend who had also been vaccinated, but her doctor told her it would still be safest to hold off booking travel for now: “I was surprised she wasn’t more positive about it. It’s the one thing I’ve been looking forward to for months, if I was lucky enough to get the shot.”
It’s not easy to find concrete expert guidance for what it is safe (or safer?) to do after receiving the COVID vaccine. Of course, patients need to wait a minimum of two weeks after receiving their second shot of the Pfizer or Moderna vaccines to develop full immunity.
But then what? Yes, we all need to continue to wear masks in public, since vaccines haven’t been proven to reduce or eliminate COVID transmission—and new viral variants up the risk of transmission. But should vaccinated individuals feel comfortable flying on a plane? Visiting family? Dining indoors? Finally going to the dentist?
It struck us that the tone of much of the available guidance speaks to public health implications, rather than individual decision-making. Take this tweet from CDC director Dr. Rochelle Walensky. A person over 65 asked her if she could drive to visit her grandchildren, whom she hasn’t seen for a year, two months after receiving her second shot. Walensky replied, “Even if you’ve been vaccinated, we still recommend against traveling until we have more data to suggest vaccination limits the spread of COVID-19.”
From a public health perspective, this may be correct, but for an individual, it falls flat. This senior has followed all the rules—if the vaccine doesn’t enable her to safely see her grandchild, what will? It’s easy to see how the expert guidance could be interpreted as “nothing will change, even after you’ve been vaccinated.”
Debates about masking showed us that in our individualistic society, public health messaging about slowing transmission and protecting others sadly failed to make many mask up.
The same goes for vaccines: most Americans are motivated to get their vaccine so that they personally don’t die, and so they can resume a more normal life, not by the altruistic desire to slow the spread of COVID in the community and achieve “herd immunity”.
In addition to focusing on continued risk, educating Americans on how the vaccinated can make smart decisions will motivate as many people as possible to get their shots.
Disparities may worsen as vaccine eligibility widens
https://mailchi.mp/85f08f5211a4/the-weekly-gist-february-5-2021?e=d1e747d2d8

Early data on vaccine distribution by race and ethnicity show a mismatch between those population groups receiving the vaccine, and those that have been hardest hit by the pandemic. As the graphic above shows, Black and Hispanic Americans have thus far been vaccinated at considerably lower rates in many states compared to their share of population as a whole—and these disparities are likely to worsen as states shift focus to senior populations for priority access, moving away from prioritizing essential workers, who tend to be more racially diverse.
The White population skews older, which stands to widen disparities in the near-term. Another compounding issue: vaccine hesitancy.
A recent Morning Consult poll found that, despite an overall increase in overall vaccine willingness, Black Americans remain the most hesitant, with only 48 percent willing to get the vaccine.
Meanwhile, Black and Hispanic Americans continue to be disproportionately impacted by COVID, with hospitalization and death rates nearly three to four times greater than those of White Americans.
Hesitancy will become an increasingly urgent problem as larger swathes of the population become eligible for vaccination, especially given that communities of color tend to be younger, as shown above.
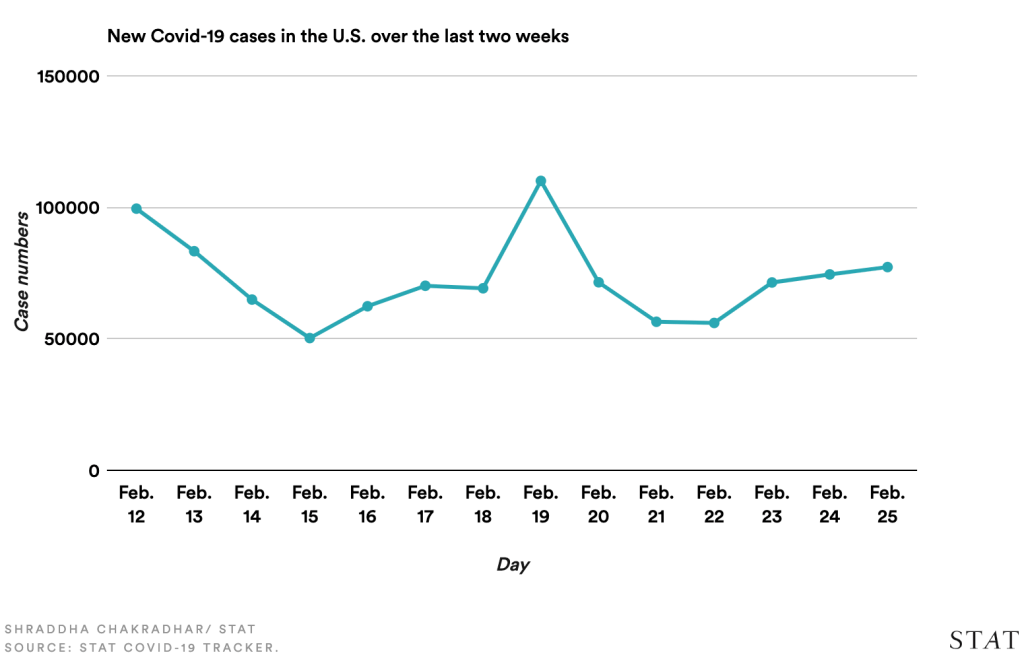
Turning the tide in the battle against the virus
https://mailchi.mp/85f08f5211a4/the-weekly-gist-february-5-2021?e=d1e747d2d8
The national COVID indicators all continued to move in the right direction this week, with new cases down 16 percent, hospitalizations down 26 percent, and deaths (while still alarmingly high at more than 3,000 per day) down 6 percent from the week prior.
More good news: both nationally and globally, the number of people vaccinated against COVID now exceeds the total number of people infected with the virus, at least according to official statistics—the actual number of coronavirus infections is likely several times higher.
On the vaccine front, Johnson & Johnson filed with the Food and Drug Administration (FDA) for an Emergency Use Authorization for its single-dose COVID vaccine, which could become the third vaccine approved for use in the US following government review later this month. The J&J vaccine is reportedly 85 percent effective at preventing severe COVID disease, although it is less effective at preventing infection than the Pfizer and Moderna shots.
Elsewhere, TheLancet reported interim Phase III results for Russia’s Sputnik V vaccine trials, showing it to be 91 percent effective at preventing infection, and a new study found the Oxford-AstraZeneca vaccine to be 75 percent effective against the more-contagious UK virus variant.
Amid the positive vaccine news, the Biden administration moved to accelerate the vaccination campaign, invoking the Defense Production Act to boost production and initiating shipments directly to retail pharmacies. With the House and Senate starting the budget reconciliation process that could eventually lead to as much as $1.9T in stimulus funding, including billions more for vaccines and testing, it feels as though the tide may be finally turning in the battle against coronavirus.
While the key indicators are still worrisome—we’re only back to Thanksgiving-week levels of new cases—and emerging variants are cause for concern, it’s worth celebrating a week that brought more good news than bad.
Best to follow Dr. Fauci’s advice for this Super Bowl weekend, however: “Just lay low and cool it.”

