A friend called me for medical advice two weeks ago. He’s single, in his thirties and generally healthy, but he’d developed a dry cough with mild congestion. After a self-administered Covid-19 test turned up negative results, he remained suspicious he could be infected.
He was set to fly west in a couple of days for a conference and dreaded the thought of infecting other passengers. I recommended a PCR test if he wanted to be more certain. When the lab results came back positive, he spent the next five days at home alone (per CDC guidance).
If you were in his shoes, chances are you, too, would make a reasonable effort to avoid infecting others. In the near future, that won’t be the case.
Americans are playing it safe—for now
A whopping 91% of Americans no longer consider Covid-19 a “serious crisis.” Social distancing has reached a low point as public-health restrictions continue to ease up.
Yet, there’s still one aspect of the pandemic Americans are taking very seriously.
As a society, we still expect people who test positive for Covid-19 to stay home and minimize contact with others. As a result of these expectations, 4 in 10 workers (including 6 in 10 low-income employees) have missed work in 2022. Overall, the nation’s No. 1 concern related to Omicron is “spreading the virus to people who are at higher risk of serious illness.”
Most Americans are eager to move on from the pandemic, but those who are sick continue to avoid actions that may potentially spread the virus.
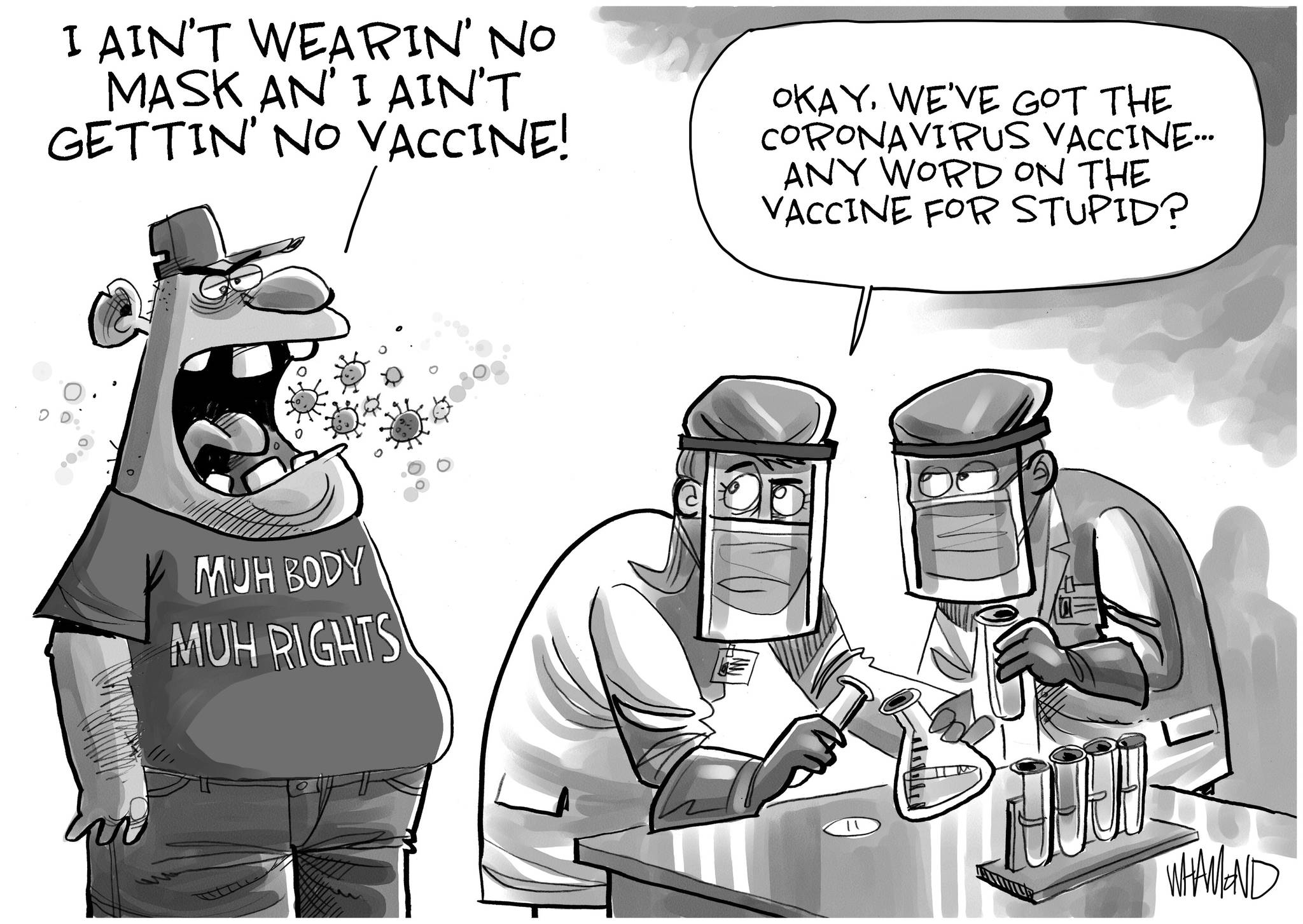
Call it what you will—group think, peer pressure or the fear of violating cultural taboos—people don’t want to put others in harm’s way. That’s true, according to polls, regardless of one’s party affiliation or vaccination status.
What’s immoral today will be appropriate tomorrow
Don’t get used to these polite and socially conscious behaviors. All of it is about to change in the not-distant future. Let me paint a picture of tomorrow’s new normal:
- A factory worker tests positive over the weekend for Covid-19 and comes to work on Monday without a mask, informing no one of his infection.
- A vacationer with mild Covid-19 symptoms refuses to postpone her spa weekend, availing herself of massages, facials and group yoga classes.
- A couple plans an indoor wedding for 200-plus, knowing the odds are likely that dozens of people will get infected and that some of those guests will be elderly and immunosuppressed.
These actions, which seem inappropriate and immoral now, will become typical. It’s not that people will suddenly become less empathetic or more callous. They’ll simply be adjusting to new social mores, brought about by a unique viral strain and an inevitable evolution in American culture.
A crash course in a unique virus
To understand why people will behave in ways that seem so unacceptable today, you must understand how the Omicron variant spreads compared to other viruses.
Scientists now know that Omicron (and its many decimal-laden strains: BA.2, BA.2.12.1, BA.4, BA.5, etc.) is the most infectious, fastest-spreading respiratory virus in world history. The Mayo Clinic calls this Covid-19 variant “hyper-contagious.”
“A single case could give rise to six cases after four days, 36 cases after eight days, and 216 cases after 12 days,” according to a report in Scientific American. As a result, researchers predict that 100 million Americans will become infected with Omicron this year alone—via new infections, reinfections and vaccination breakthroughs.
In addition to Omicron’s high transmissibility, the virus is also season-less. Whereas influenza arrives each winter and exits in the spring, Americans will continue to experience high levels of Covid-19 infection year-round—at least for the foreseeable future.
With its 60-plus mutations, immense transmissibility and lack of seasonality, Omicron is an exceptional virus: one that will infect not only our respiratory systems but also our culture.
Over time, Omicron’s unique characteristics will drive Americans to deny and ignore the risks of infection. In the near future, they’ll make decisions and take actions that they’d presently deem wrong.
A culture shock is coming
Culture—which comprises the shared values, norms and beliefs of a group of people—doesn’t change because someone decides it should. It evolves because circumstances change.
The pandemic has no doubt been a culture-changing event and, as the circumstances of Covid-19 have changed, so too have our underlying values, beliefs and behaviors.
If 100 million Americans (one-third of the population) were to become infected with Omicron this year, we can expect that everyone will know someone with the disease. And when dozens of our friends or colleagues say they’ve had it, we will begin to see transmission as inevitable. And since, statistically, most Americans won’t die from Omicron, people will see infection as relatively harmless and they’ll be willing to drop their guard.
We’ll see more and more people going to work even when they’re infected. We’ll see more people on trains and planes, coughing and congested, having never taken a Covid-19 test. And we’ll see large, indoor celebrations taking place without any added safety measures, despite the risks to the most vulnerable attendees.
Amid these changes, health officials will continue to urge caution, just as they have for more than two years. But it won’t make a difference. Culture eats science for breakfast. Americans will increasingly follow the herd and stop heeding public-safety warnings.
The process of change has begun
Cultural shifts happen in steps. First, a few people break the rules and then others follow.
Recall my friend, the one who took two tests out of an abundance of caution. Next time, perhaps he’ll decide he’d rather not miss the conference. Perhaps when he returns home, he will tell his friends that he felt sick the whole trip. Perhaps they’ll ask, “Do you think you might have had Covid?” And perhaps he will reply: “What difference would it have made? I’m fully vaccinated and boosted.”
And so, it will go. The next time someone in his social circle feels under the weather, he or she won’t even bother to do the first test.
This change process has already begun. Take the White House Correspondents’ Dinner, for example. Last year, the event was cancelled. This year, guests had to show proof of vaccination or a negative same-day test. However, that rule didn’t apply to staff at the hotel who worked the event. Unsurprisingly, several high-profile attendees got Covid-19 but, so far, no reports of anyone being hospitalized. A year from now, assuming no major mutations cause the virus to become more lethal, we can expect all restrictions will be dropped.
Culture dictates how people behave. It influences their thoughts and actions. It alters their values and beliefs. The unique characteristics of Omicron will lead people to ignore the harm it inflicts. They won’t act with malicious intent. They’ll just be oblivious to the consequences of their actions. That’s how culture works.