Category Archives: Reputation
Health System Chief Strategy Officer Roundtable Assessment: ‘The Near-Term is Tough, the Long-Term is Uncertain and the Deck is Stacked against Hospitals’

On November 2-3 in Austin, I moderated the 4th Annual CSO Roundtable* in which Chief Strategy/Growth Officers from 12 mid-size and large multi-hospital systems participated. The discussion centered on the future: the issues and challenges they facing their organizations TODAY and their plans for their NEAR TERM (3-5 years) and LONG-TERM (8-10 years) future. Augmenting the discussion, participants rated the likelihood and level of disruptive impact for 50 future state scenarios using the Future State Diagnostic Survey. *
Five themes emerged from this discussion:
1-Major change in the structure and financing of U.S. health system is unlikely.
- CSOs do not believe Medicare for All will replace the current system. They anticipate the existing public-private delivery system will continue with expanded government influence likely.
- Public funding for the system remains problematic: private capital will play a larger role.
- CSOs think it is unlikely the public health system will be fully integrated into the traditional delivery system (aka health + social services). Most hospital systems are expanding their outreach to public health programs in local markets as an element of their community benefits strategy.
- CSOs recognize that states will play a bigger role in regulating the system vis a vis executive orders and referenda on popular issues. Price controls for hospitals and prescription drugs, restraints on hospital consolidation are strong possibilities.
- Consensus: conditions for hospitals will not improve in the immediate and near-term. Strategies for growth must include all options.
2-Health costs, affordability and equitable access are major issues facing the health industry overall and hospitals particularly.
- CSOs see equitable access as a compliance issue applicable to their workforce procurement and performance efforts and to their service delivery strategy i.e., locations, patient experiences, care planning.
- CSOs see reputation risk in both areas if not appropriately addressed in their organizations.
- CSOs do not share a consensus view of how affordability should be defined or measured.
- There is consensus among CSOs that hospitals have suffered reputation damage as a result of inadequate price transparency and activist disinformation campaigns. Executive compensation, non-operating income, discrepancies in charity care and community benefits calculations and patient “sticker shock” are popular targets of criticism.
- CSO think increased operating costs due to medical inflation, supply chain costs including prescription drugs, and labor have offset their efforts in cost reduction and utilization gains.
- CSO’s are focusing more of their resources and time in support of acute clinical programs where streamlining clinical processes and utilization increases are achievable near-term.
- Consensus: the current financing of the system, particularly hospitals, is a zero-sum game. A fundamental re-set is necessary.
3-The regulatory environment for all hospitals will be more challenging, especially for not-for-profit health systems.
- Most CSOs think the federal regulatory environment is hostile toward hospitals. They expect 340B funding to be cut, a site neutral payment policy in some form implemented, price controls for hospital services in certain states, increased federal and state constraints on horizontal consolidation vis a vis the FTC and State Attorneys General, and unreasonable reimbursement from Medicare and other government program payers.
- CSOs believe the challenges for large not-for-profit hospital systems are unique: most CSOs think not-for-profit hospitals will face tighter restrictions on their qualification for tax-exempt status and tighter accountability of their community benefits attestation. Most expect Congress and state officials to increase investigations about for-profit activities, partnerships with private equity, executive compensation and other issues brought to public attention.
- CSOs think rural hospital closures will increase without significant federal action.
- Consensus: the environment for all hospitals is problematic, especially large, not-for-profit multi-hospitals systems and independent rural facilities.
4-By contrast, the environment for large, national health insurers, major (publicly traded) private equity sponsors and national retailers is significantly more positive.
- CSOs recognize that current monetary policy by the Fed coupled with tightening regulatory restraints for hospitals is advantageous for national disruptors. Scale and access to capital are strategic advantages enjoyed disproportionately by large for-profit operators in healthcare, especially health insurers and retail health.
- CSOs believe publicly traded private equity sponsors will play a bigger role in healthcare delivery since they enjoy comparably fewer regulatory constraints/limitations, relative secrecy in their day-to-day operations and significant cash on hand from LPs.
- CSOs think national health insurer vertical consolidation strategies will increase noting that all operate integrated medical groups, pharmacy benefits management companies, closed networks of non-traditional service providers (i.e. supplemental services like dentistry, home care, et al) and robust data management capabilities.
- CSOs think national retailers will expand their primary care capabilities beyond traditional “office-based services” to capture market share and widen demand for health-related products and services
- Consensus: national insurers, PE and national retailers will leverage their scale and the friendly regulatory environment they enjoy to advantage their shareholders and compete directly against hospital and medical groups.
5-The system-wide shift from volume to value will accelerate as employers and insurers drive lower reimbursement and increased risk sharing with hospitals and medical groups.
- CSOs think the pursuit of value by payers is here to stay. However, they acknowledge the concept of value is unclear but they expect HHS to advance standards for defining and measuring value more consistently across provider and payer sectors.
- CSOs think risk-sharing with payers is likely to increase as employers and commercial insurers align payment models with CMS’ alternative payment models: the use of bundled payments, accountable care organizations and capitation is expected to increase.
- CSOs expect network performance and data management to be essential capabilities necessary to an organization’s navigation of the volume to value transition. CSOs want to rationalize their current acute capabilities by expanding their addressable market vis a vis referral management, diversification, centralization of core services, primary and preventive health expansion and aggressive cost management.
- Consensus: successful participation in payer-sponsored value-based care initiatives will play a bigger role in health system strategy.
My take:
The role of Chief Strategy Officer in a multi-hospital system setting is multi-functional and unique to each organization. Some have responsibilities for M&A activity; some don’t. Some manage marketing, public relations and advocacy activity; others don’t. All depend heavily on market data for market surveillance and opportunity assessments. And all have frequent interaction with the CEO and Board, and all depend on data management capabilities to advance their recommendations about risk, growth and the future. That’s the job.
CSOs know that hospitals are at a crossroad, particularly not-for-profit system operators accountable to the communities they serve. In the 4Q Keckley Poll, 55% agreed that “the tax exemption given not-for-profit hospitals is justified by the community benefits they provide” but 45% thought otherwise. They concede their competitive landscape is more complicated as core demand shifts to non-hospital settings and alternative treatments and self-care become obviate traditional claims-based forecasting. They see the bigger players getting bigger: last week’s announcements of the Cigna-Humana deal and expansion of the Ascension-LifePoint relationship cases in point. And they recognize that their reputations are under assault: the rift between Modern Healthcare and the AHA over the Merritt Research ’s charity care study (see Hospital section below) is the latest stimulant for not-for-profit detractors.
In 1937, prominent literary figures Laura Riding and Robert Graves penned a famous statement in an Epilogue Essay that’s especially applicable to hospitals today: “the future is not what it used to be.”
For CSO’s, figuring that out is both worrisome and energizing.
Thought of the Day: On Reputation
Why this insurance CEO thinks big healthcare brands are losing significance

Legacy health brands are losing their significance as healthcare consumers place higher value on convenience than reputation. That’s the idea behind a July 1 tweet by Sachin Jain, MD, the CEO of Scan Group and Scan Health Plan.
“We are in an era of the declining significance of big healthcare brands,” he said.
To Dr. Jain, big healthcare brands are the ones commonly known for being the best in a specific specialty or renowned in their region. While many big healthcare brands have high quality performance metrics to hang their clout on, Dr. Jain believes reliance on name alone is problematic.
“There’s been an arrogance by a lot of healthcare organizations that have kind of sold on brand. There’s going to be a reckoning for some of those organizations. My personal view is that the next generation of healthcare consumers is going to be less aligned to think about brands in the same way,” Dr. Jain told Becker’s.
Today’s patients are paying more attention to convenience, digital access and price than reputation. Cost of care, ease of scheduling and accessibility are beating out recognition, Dr. Jain said.
At Scan, Dr. Jain said the Long Beach, Calif.-based Medicare Advantage insurer that serves more than 220,000 members is hyperfocused on staying as human as possible and fulfilling unmet needs for its community.
“Elite healthcare brands are entering this fun phase where they are becoming underdogs. They need to have a chip on their shoulders almost to thrive and perform in this next phase,” Dr. Jain said. “Because I’m not sure payers are necessarily going to continue to pay the same premiums per brand.”
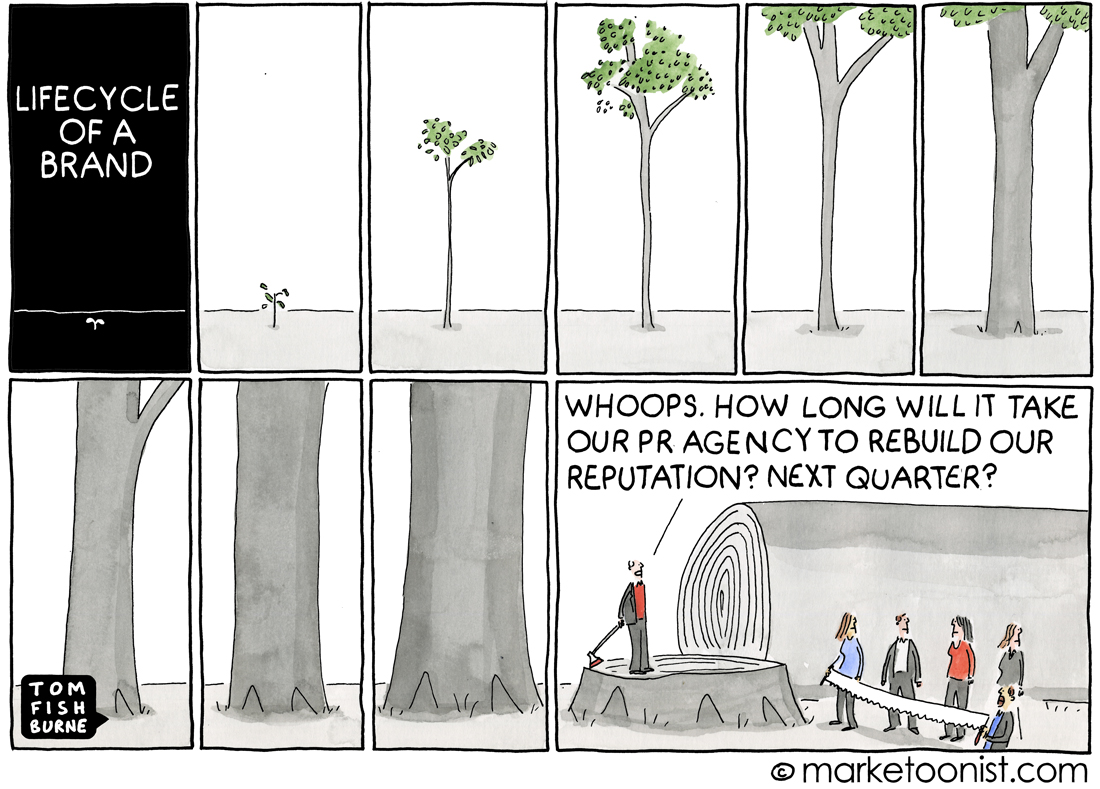
Cartoon – Lifecycle of a Brand