Category Archives: Uncategorized
Cartoon – The Deciding Vote
Cartoon – Everything is Negotiable
GAO: rural hospital closures increasing, South hardest hit
https://www.healthcaredive.com/news/gao-rural-hospital-closures-increasing-south-hardest-hit/538604/

Dive Brief:
- Hospitals across the U.S. are being battered by financial headwinds, and rural hospitals are vulnerable because they don’t have capital or diversified services to fall back on when the going gets rough. Between 2013 and 2017, 64 rural hospitals closed due to financial distress and changing healthcare dynamics, more than twice the number in the previous five years, a new Government Accountability Office analysis shows.
- Rural hospital closures disproportionately occurred in the South, among for-profit hospitals and among organizations with a Medicare-dependent hospital payment designation.
- One potential lifeline was Medicaid expansion. According to GAO, just 17% of rural hospital closures occurred in states that had expanded Medicaid as of April 2018.
Dive Insight:
Declining inpatient admissions and reimbursement cuts have taken a toll on rural hospitals. Since 2010, 86 rural hospitals have closed, and 44% of those remaining are operating at a loss — up from 40% in 2017.
CMS Administrator Seema Verma released a rural health strategy in May aimed at improving access and quality of care in rural communities. Among its objectives are expanding telemedicine, empowering patients in rural areas to take responsibility for their health and leveraging partnerships to advance rural health goals.
The agency also expanded its Rural Community Hospital Demonstration from 17 to 30 hospitals. The program reimburses hospitals for the actual cost of inpatient services rather than standard Medicare rate, which could be as little as 80% of actual cost.
Such initiatives can be helpful, but if a hospital can’t make ends meet on its Medicare and Medicaid businesses and has only a modicum of privately insured patients, “that’s just not a balance that works financially,” Diane Calmus, government affairs and policy manager at the National Rural Health Association, told Healthcare Dive recently.
In all, 49 rural hospitals closed in the South, or 77% of rural hospital closures from 2013 through 2017, according to GAO. Texas had the most closures with 14, followed by Tennessee with eight and Georgia and Mississippi, each with five. By contrast, there were eight rural hospital closures in the Midwest and four each in the West and Northeast.
GAO also looked at closures by Medicare rural hospital payment designation. Critical access hospitals made up 36% of rural hospital closures, 30% were hospitals receiving Medicare standard inpatient payment, 25% had Medicare-dependent hospital designation and 9% were sole community hospitals.
To aid rural hospitals and ensure access for patients, NRHA has urged CMS to adopt a common sense approach to the “exclusive use” standard and lobbied lawmakers to pass legislation eliminating the 96-hour condition of payment requirement, two policies that are particularly hard on rural providers.
Another bill, the Save Rural Hospitals Act, would reverse reimbursement cuts to rural hospitals, provide other regulatory relief and establish the community outpatient hospital, a new provider type offering 24/7 emergency services plus outpatient and primary care.
1 big thing: Out-of-network coverage is disappearing
One reason surprise medical bills are going up: Coverage for out-of-network care is going down, according to the Robert Wood Johnson Foundation.
Per RWJF:
- Just 29% of insurance plans in the individual market provide any benefits for out-of-network providers. That’s down from 58% a mere three years ago.
- Coverage is also declining in the market for small businesses, but not nearly as dramatically — 64% of small-group plans offer some out-of-network coverage, down from 71% in 2015.
- Those small-group numbers are probably roughly in line with where things stand among large employers’ plans.
Why it matters: The burgeoning controversy over surprise hospital bills stems partly (though not exclusively) from the bills patients receive when they’re treated by an out-of-network provider — even without their knowledge, often within an in-network facility.
- Out-of-network coverage has obviously never been as generous as in-network coverage (that’s the whole point of creating a network), but as insurers pull back even further, more patients will likely find themselves on the hook for even bigger bills.
Hospitals led healthcare industry hiring in September
http://www.modernhealthcare.com/article/20181005/NEWS/181009931
Month after month this year, the ambulatory sector has led the pack when it comes to healthcare industry hiring. But hospitals managed to push ahead in September to take the top spot.
Hospitals added 12,000 jobs last month, 47% of total healthcare hiring, and easily beating out ambulatory’s 10,300 jobs. Healthcare overall added a healthy 25,700 jobs in September, 23% fewer than the 33,200 jobs added in August, but still well above July’s 16,700 new hires, according to the U.S. Bureau of Labor Statistics’ newest jobs report released Friday.
The September jobs report ticked the U.S. unemployment rate down to 3.7%, the lowest it’s been since 1969. A total of 134,000 new jobs were added to the U.S. economy last month. Healthcare hiring trailed that of professional and business services, which added 54,000 jobs, but beat out transportation and warehousing, which added 23,800 new jobs. The construction industry made 23,000 new hires.
Ambulatory sector hiring was weak in September compared with its robust showing for much of the year. Physicians’ offices added the most jobs, at 4,100—800 fewer than in August. Home health added 2,200 jobs, 72% fewer than the month before. Dental office hiring, which has been weak in recent months, shed 500 jobs.
Outpatient care centers added 1,000 jobs in September, while offices of other health practitioners added 2,000.
Nursing and residential care facilities added 3,400 jobs in September, 13% fewer than in August. Within that sector, other residential care facilities added 1,400 jobs, and community care facilities for the elderly made 1,100 new hires. Nursing care facilities, a typically weak hiring area this year, made 200 new hires in September. Residential mental health facilities added 700 jobs.
Cleveland Clinic may grow to 15 hospitals
The boards of Cleveland Clinic and Vero Beach, Fla.-based Indian River Medical Center voted to approve a series of agreements allowing IRMC to integrate into the Cleveland Clinic, the organizations announced Oct. 3.
Here are five things to know:
1. The advisers and legal teams of both organizations shared details of the agreements with board members during a public meeting Sept. 25. Board members and trustees spent the last week analyzing the details and finalized their decision Oct. 3. Officials from both organizations will formally sign the agreements later this week.
2. Under the deal, IRMC and its affiliates will become part of the Cleveland Clinic, which also agreed to commit at least $250 million to IRMC over the next 10 years.
3. Cleveland Clinic will maintain full governance over IRMC and has committed to maintaining maternity care, inpatient well-baby care/pediatrics and gynecology services, behavioral health services, and other inpatient and outpatient services for at least 10 years. However, the hospital district will phase out support for indigent care at IRMC during the three years after the transaction closes.
4. The deal is still pending regulatory approval.
5. Cleveland Clinic recently inked a definitive agreement to purchase Martin Health System, a three-hospital institution in Stuart, Fla. If both deals are successful, Cleveland Clinic will comprise 15 hospitals in addition to its main campus.
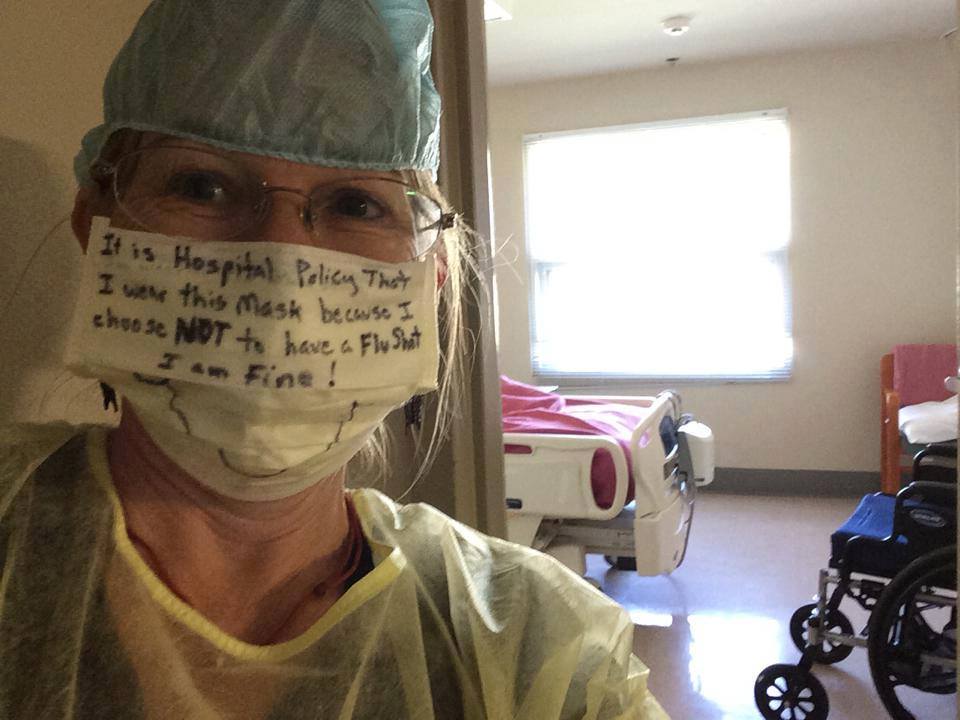
EEOC sues Saint Thomas Health over mandatory flu shot policy
The U.S. Equal Employment Opportunity Commission filed a lawsuit against Nashville, Tenn.-based Saint Thomas Health Sept. 28, alleging Murfreesboro, Tenn.-based Saint Thomas Rutherford Hospital violated federal law by ordering an employee to receive a flu shot despite his religious beliefs.
Saint Thomas Health requires all workers to receive an annual flu shot, which includes employees from TouchPoint Support Services — one of the Saint Thomas Rutherford Hospital’s food and environmental services providers, according to the EEOC.
In 2013 and 2014, Saint Thomas Health allowed the TouchPoint employee at the center of the lawsuit to wear a protective mask, instead of receiving a flu shot, due to his religious beliefs. When the employee requested to again forego the flu shot in 2015, Saint Thomas Health turned down his request and fired the employee after he refused to get vaccinated, according to the EEOC.
“For several years, [Saint Thomas Health] accommodated the employee’s religious belief,” Delner Franklin-Thomas, director of the EEOC’s Memphis District Office, said in the press release. “Then, [Saint Thomas Health] refused to accommodate his religious belief. An employer should not force an employee to choose between employment and his religious belief unless doing so would cause an undue hardship to the employer.”
Becker’s Hospital Review reached out to St. Louis-based Ascension, which owns Saint Thomas Health, for comment on the suit and will update the article as more information becomes available.
Cartoon – Modern Pediatric Exam

Cartoon – Who ever heard of linking pay to performance?