https://www.axios.com/2026/02/03/trump-drug-price-deals-pfizer-eli-lilly

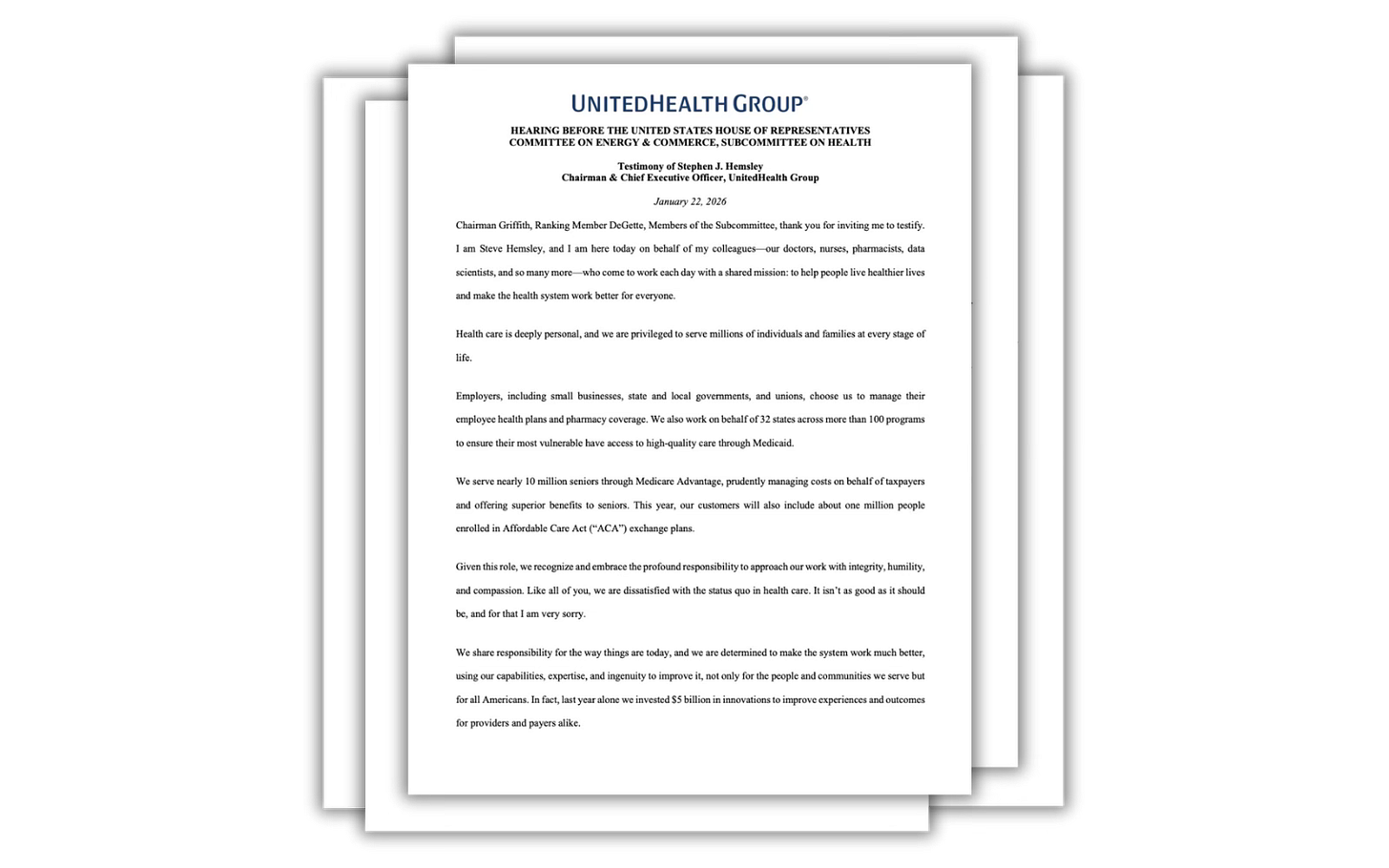
The Trump administration is facing new pressure to disclose details about its confidential pricing agreements with big drug companies and whether they meaningfully lower costs for patients.
Why it matters:
President Trump has touted the “most favored nation” drug pricing deals as one of his signature accomplishments, but most of the details have been kept under wraps, including how the new prices are calculated.
Driving the news:
The advocacy group Public Citizen filed a Freedom of Information Act suit last week, seeking the text of the deals the administration struck with Eli Lilly and Pfizer.
- Those and other agreements were touted in high-profile Oval Office ceremonies as a step toward lowering U.S. drug prices and aligning them with what’s paid in other developed countries.
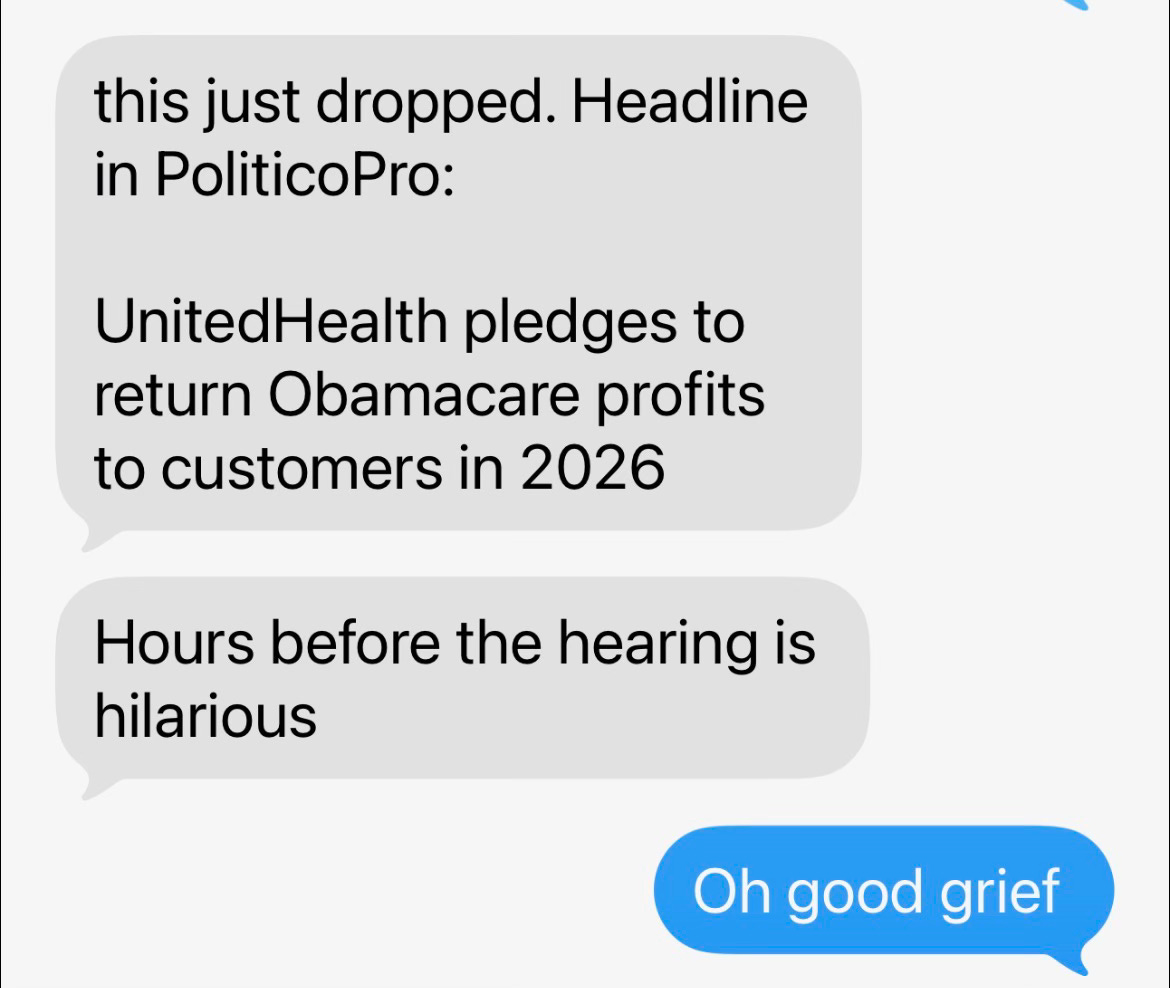
- The deals have been described in broad terms, but questions remain about basic matters like what exactly the companies agreed to.
- The administration is “shaking hands with pharma CEOs and telling us they fixed drug pricing and then not disclosing any text,” said Peter Maybarduk, access to medicines director at Public Citizen. “It makes it hard to believe, makes it hard to understand, makes it hard to assess.”
Congressional Democrats also wrote to Pfizer, Eli Lilly, AstraZeneca and Novo Nordisk in December asking for details of their respective agreements.
- The letter to Pfizer said the company and the administration seem to be “attempting to shield themselves from oversight, accountability, and specifics that could inform consumers about whether this agreement will save money.”
- An administration official said: “Because the drug pricing agreements contain confidential, proprietary and commercially sensitive information, they will not be released publicly.”
- None of the four companies provided more details when asked about the agreements. A Novo Nordisk spokesperson said “this agreement will bring semaglutide medicines to more American patients at a lower cost,” referring to the active ingredient in its blockbuster weight-loss drugs.
Between the lines:
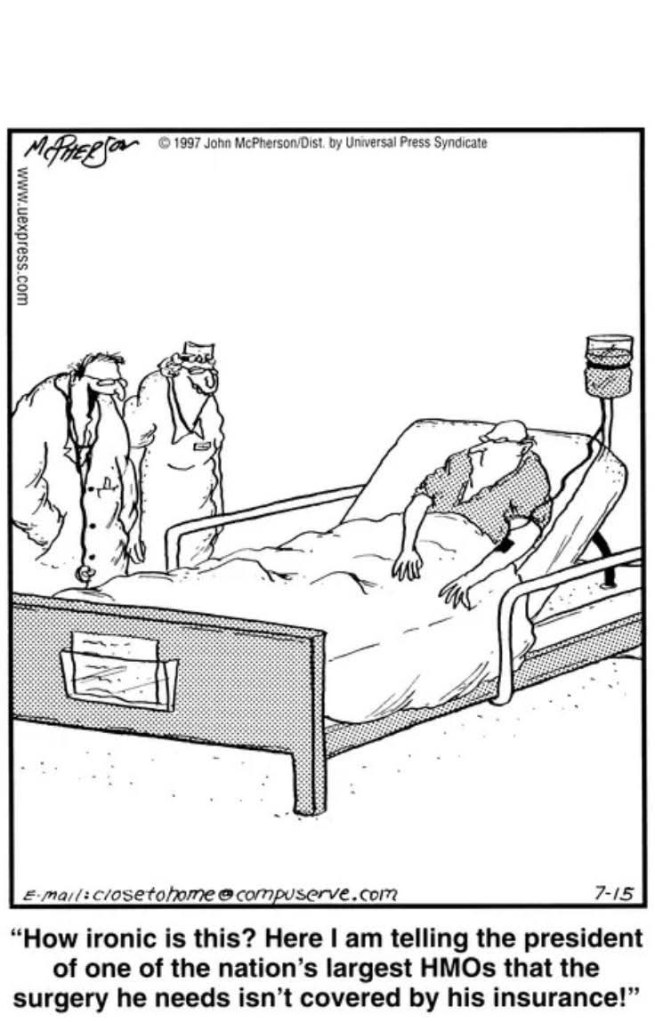
The deals would for the most part not lower existing drug prices for a huge segment of the public that gets coverage through Medicare or workplace insurance.
- Instead, the most-favored nation prices would apply to Medicaid. One unanswered question is how much lower would those prices be, since drugmakers already are required to have low prices for Medicaid.
- The deals also anticipate most-favored nation prices for newly launched drugs in future years. But it’s not fully clear how that would work, since drugs are usually launched in the United States first and there wouldn’t yet be prices abroad to use as a comparison.
- There would also be discounted drugs sold through the government’s direct-to-consumer website TrumpRx. But the portal is built around cash purchases, which many cannot afford.
The big picture:
Trump has railed against what he calls “global freeloading” and ending the way the U.S. pays more for drugs than other developed countries. But policy experts have questioned whether manufacturers will only meet him halfway, raising prices abroad without cutting them in the U.S.
- “You can kind of see why the pharmaceutical industry wouldn’t be so opposed if what they end up getting is maybe a slightly lower price in the U.S. and higher prices in other countries,” said Juliette Cubanski, deputy director of the Program on Medicare Policy at KFF.
- The Trump administration has also proposed new payment models to incorporate most-favored nation pricing into Medicare, which would lead to savings.
- But the changes are tests that would only apply in certain geographic areas, and analysts say they would not have a drastic impact on Medicare spending.
The bottom line:
Maybarduk, of Public Citizen, acknowledged that the goals of the drug pricing efforts are laudable, even if the practical effects remain unclear.
- “The thing that we agree with here, of course, is that Americans pay too much for drugs, and we pay more than other countries for drugs.”