
Cartoon – Shining a Fresh Light on the Same Ideas


Here’s a look at how the margins of the largest in the quarter, based on data compiled by Bloomberg:
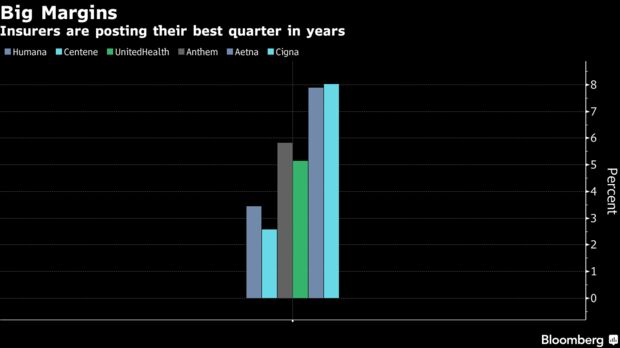
U.S. health insurers just posted their best financial results in years, shrugging off worries that the worst flu season in recent history would hurt profits.
Aetna Inc., for instance, posted its widest profit margin since 2004. Centene Corp. had its most profitable quarter since 2008. And Cigna Corp., which reported on Thursday, had its biggest margin in about seven years.
Analysts at Morgan Stanley, in a research note, said insurers are in the midst of a “hot streak.”
One big reason for the windfall is the tax cuts passed by Congress last year, which in some cases more than halved what the insurers owe the government. Aetna said its effective tax rate fell to 16.8 percent from 39.6 percent, for example. Many insurers also spent less on medical care than analysts had expected, even taking into account increased spending on flu treatments.
http://www.modernhealthcare.com/article/20180505/NEWS/180509944

Sending a senior executive off-site to expand his perspective was part of the Cincinnati-based health system’s leadership institute, which aims to develop the skills of some 1,000 administrative and physician executives and prepare them for new roles.
While many executives move around within their organization’s network, the approach aimed to expose the employee—who had spent much of his career at TriHealth—to another corporate culture and operations.
“We obsess about spending $2 million on a CT scanner, but we can’t find a way to spend $10,000 on investing in our leaders,” said TriHealth CEO Mark Clement, who launched the system’s leadership institute about ½ years ago. “I would argue that investments on improving talent within our organization produce dividends far greater than a piece of equipment.”
For many providers, it’s the end of an era. Hospital, health system and physician group executives are seeking new leaders. They are prompted by an exodus of top healthcare executives, a generational transfer of power highlighted by the departures of senior managers like Dr. Toby Cosgrove, former Cleveland Clinic CEO; Michael Murphy, CEO of Sharp HealthCare who is retiring in 2019; and outgoing Mayo Clinic CEO Dr. John Noseworthy.
Organizations are actively searching for what’s next and who will take them there. Industry consolidation is accelerating that conversation. But there is wide variation on their approach and level of preparation.
There’s a lot at stake, both from a cultural and financial perspective, said Mark Armstrong, vice president of consulting operations at Quorum Health Resources. Good managers translate to engaged employees, he said.
But only about 33% of U.S. workers are actively engaged in their jobs, and a mere 15% of employees strongly agree the leadership of their organization makes them enthusiastic about the future, according to a 2016 poll by Gallup. The firm estimates that disengaged employees cost the U.S. $483 billion to $605 billion each year in lost productivity.
“Even when systems know someone is retiring, it is interesting how few of them still don’t have an assertive plan in place,” Armstrong said. “Any kind of turnover can be disruptive, especially if there has been a trend of declining performance. It’s not unusual for a ratings agency to have heightened concerned when a CEO leaves.”
Almost every system grapples with a huge retention problem, which can make it difficult to plan ahead, said Alan Rolnick, CEO of Employee Engagement and Retention Advisors. The most costly departures are often experienced nurses, he said.
“It’s not just the cost of replacement but the loss of institutional knowledge,” Rolnick said.
TriHealth’s leadership program highlights potential candidates within the system who could fill upcoming vacancies. It puts executives on a multiyear track that assesses potential areas for improvement and exposes them to systemwide quarterly leadership training sessions and other development opportunities. The company’s vice president of finance, Brian Krause, spent a week at BJC HealthCare in St. Louis, relying on connections TriHealth had with the organization. Krause is also planning on spending some time at the University of Pennsylvania Health System, as well as a few other systems.
Since launching the institute—which is conducted with the help of the consultancy Studer Group—TriHealth’s employee engagement improved from the 26th to the 74th percentile, which has helped the organization generate a 3.5% operating margin—one of its highest margins in recent history, Clement said. Its patient experience scores are also up from the 50th percentile to the 75th, helping to drive an increase in admissions, bucking the national trend.
Ideally, promoting from within will ensure cultural and operational continuity and motivate executives, Clement said. “When you bring new senior executives in from other organizations, it can be a threat to the culture,” he said. “For an organization like ours that has invested a lot of money in building a culture based on value, engaging team members and flattening the organization, it’s often best to promote from within.”
Ascension also recently launched a diversity inclusion campaign that seeks to cultivate minority leaders.
“The types of leaders are changing,” Ascension CEO Anthony Tersigni said at the American College of Healthcare Executives’ 2018 Congress on Healthcare Leadership in March. “The time for guys like me who started as a hospital operator is passing.”
The CEO of a Fortune 100 company told Tersigni several years ago that he spends about 30% of his time on leadership development. Tersigni, who at the time only spent a fraction of that on cultivating executives, said that interaction completely changed his perspective. Ascension has since partnered with a number of universities to build a better leadership curriculum and management pipeline.
“Disruption in the healthcare industry is not going to come from the hospital across the street, it has been coming from outside the industry,” Tersigni said. “We need to understand how they think, how they act, how they make decisions, because it is a lot faster than healthcare can dream of.”
Renton, Wash.-based Providence St. Joseph in 2017 partnered with the University of Great Falls in Montana, in part, to create a stable pipeline of managers to feed into the integrated health system. The university, which was renamed University of Providence, will include professional and certificate programs for Providence St. Joseph’s more than 111,000 employees.
The health system has also implemented mentoring and leadership development programs that have increased its women executive cohort by 50% over a three-year period.
“Diversity begets diversity,” said Dr. Rod Hochman, CEO of Providence St. Joseph, adding that women and minority leaders will help the system better understand its most vulnerable populations. “We are looking for folks with different perspectives who can help lead us through this time of change.”
Whether the successors are internal or external, establishing a strong executive pipeline requires a proactive and standardized approach, and the board should take the lead, industry analysts said.
A health system should identify the competencies it needs to lead the team going forward and where the gaps are, said Craig Deao, a senior leader at Studer Group. “The three keys leaders of tomorrow need to have are getting people to do things better—performance improvement; getting them to do new things—innovation; and helping people do those things—engagement,” he said.
Managing the process rather than the people will translate to more innovative and engaged employees, according to Rolnick. It starts with communication, he said.
“Today, the average employee of a hospital has no idea of the strategic direction of their organization and what their role is,” Rolnick said. “You have to tell them as much as you can, and be open and honest.”
Beyond employee engagement, executives need to understand how to interact with patients. As the industry adapts to thinking of patients as consumers, that requires a different lens, Deao said.
“People need to understand how to shape behavior and apply concepts of psychology to running the business,” he said.
Healthcare is becoming more consumer- and technology-oriented. Health systems are also focusing more on nutrition, transportation, education, fitness and other social factors that influence an individual’s health.
Novant Health, for instance, is launching a new leadership program that looks to train untapped community leaders in Charlotte-Mecklenburg, N.C. The program involves a combination of teaching sessions and mentoring that aims to reach individuals who otherwise wouldn’t have access to programs that hone their leadership skills, said Tanya Blackmon, executive vice president and chief diversity and inclusion officer at Novant.
While there is a significant learning curve, experience in consumer insight, marketing or technology can better equip individuals to tackle healthcare’s current challenges, said David Schmahl, executive vice president of consultancy SmithBucklin and chief executive of its healthcare and scientific industry practice.
“The experience people are obtaining in leadership roles outside the healthcare field is critical,” he said.
The role of healthcare leadership has evolved into a platform used to convey a moral foundation, spanning conversations from racism to gun control. They have to balance their role as an influencer while dealing with budgets, managing their boardrooms, implementing both long-term visions and short-term goals, and maintaining an engaged workforce.
The average tenure of healthcare executives and managers is also decreasing, particularly among CEOs, nurses and physicians, which exacerbates labor shortages. A C-suite executive’s pay is still tied to financial metrics, but quality, safety and patient satisfaction are becoming a more prominent determinant.
While Novant’s initiative isn’t necessarily geared to develop successors, it signifies how the definition of a leader is evolving.
“We are looking at trying to tap talent across all spectrums,” Blackmon said. “We’re not leaving any area untapped.”

The high-profile investors, including Ms. DeVos and Mr. Murdoch, collectively invested about $600 million in the company Theranos
Even some of the world’s richest people may get duped, according to newly unsealed documents in a lawsuit filed on behalf of investors in the failing blood-testing company Theranos.
High-profile investors who collectively lost hundreds of millions of dollars included Walmart’s Walton family, the media mogul Rupert Murdoch, as well as Betsy DeVos, the secretary of education and her relatives.
The list of investors, which was first reported by The Wall Street Journal, came to light as part of a class-action lawsuit brought in 2016 by Robert Colman, a retired Silicon Valley investment banker, who claims that Theranos misled investors about its business and technology.
Theranos, founded by Elizabeth Holmes when she was a 19-year-old Stanford University dropout, promised to revolutionize the lab industry using a few drops of blood from a simple finger-prick to look for everything from diabetes to cancer, at a fraction of the cost of a traditional blood test.
The company became a Silicon Valley fairy tale, with investors awarding the privately held company a valuation of around $9 billion. But the story began to unravel in October 2015 after The Wall Street Journal, owned by Mr. Murdoch’s News Corp., began questioning whether the tests worked. Theranos became the subject of federal investigations into its testing and claims of proprietary technology, which were called “nanotainers.” Much of the time the company had to resort to using conventional blood testing methods, unable to get federal approval for any test but one for Herpes.
Theranos and its founder also became embroiled in a series of lawsuits, involving investors as well as one of its key partners, Walgreens, a large drugstore chain, where it offered its tests. The company reached a settlement with Walgreens last August.
In March, the Securities and Exchange Commission charged Ms. Holmes with fraud, accusing her of exaggerating and lying about her technology to attract investors. As part of the S.E.C. action, Ms. Holmes agreed to pay $500,000, give up control of her company, and is barred from serving as an officer or director of any public company for 10 years. She and Theranos did not admit nor deny the allegations.
Theranos still faces the class-action lawsuit, and may still be subject to a criminal investigation by the United States attorney in San Francisco. The company’s future is unclear. The company did not respond to requests for comment.
Theranos had always boasted a star-studded list of investors and directors — its board included the former secretaries of state George P. Shultz and Henry A. Kissinger, two former United States senators, and Gen. Jim Mattis, the current secretary of defense. But while some high-profile investors’ links to Theranos had been previously known, the new documents provide a detailed list of financial amounts.
The Walton family invested about $150 million in 2014 through two separate entities, according to the investor list. Mr. Murdoch put in about $125 million, and the extended family of Ms. DeVos invested about $100 million.
“It’s obvious that they are highly disappointed in them as a company and as an investment,” said Greg McNeilly, the chief operating officer of The Windquest Group, the holding company of Ms. DeVos and her husband. Mr. McNeilly said the $100 million was a joint investment across multiple generations and branches of her family, and described the share held by Ms. DeVos and her husband as “minor.”
Other prominent investors, according to the list, included the Cox family; the Atlanta billionaires who own the media conglomerate Cox Enterprises and who invested $100 million; and a company affiliated with Mexican billionaire Carlos Slim that put in about $30 million. Robert K. Kraft, the owner of the New England Patriots, invested $1 million.
Representatives for Mr. Kraft, the Walton family, Cox Enterprises and News Corp. declined to comment.

At a rally in Michigan a little over a week ago, President Trump assured his supporters that he had kept his promise to abolish the Affordable Care Act — even though Congress had failed to repeal the Obama-era health law.
“Essentially, we are getting rid of Obamacare,” Mr. Trump said, reminding a cheering crowd that the individual mandate that required most people to have health insurance or pay a penalty was scrapped as part of the Republican tax bill he signed into law last year. “Some people would say, essentially, we have gotten rid of it.”
But despite Mr. Trump’s longstanding desire to unwind the signature legislative achievement of his predecessor, many parts of the Affordable Care Act remain in place. And the Trump administration is even enforcing some of its provisions more aggressively than President Barack Obama did — a reality that has enraged business groups and Republicans in Congress who still want the law officially repealed.
While the individual mandate may be dead, the employer mandate — the requirement that many companies offer health insurance to their workers or pay a penalty — is very much alive. Under Mr. Trump, the Internal Revenue Service has been pursuing companies that fail to comply with the mandate and, according to the agency, was sending penalty notices to more than 30,000 businesses around the country.
Business groups are pushing for the I.R.S. to stop enforcing the mandate and House Republicans, who voted to repeal much of the Affordable Care Act a year ago, have proposed legislation to eliminate it. But most Democrats oppose major changes to the law and the Republican leaders in the Senate have shown no interest in tackling health care after last year’s stinging defeat.
The employer mandate requires companies with more than 50 full-time employees to provide health benefits to eligible employees or face fines of more than $2,000 per worker. The Congressional Budget Office predicted that these fines would total $12 billion in 2018.
The I.R.S. is working on settlements with some of the businesses that have had technical issues or paperwork glitches, according to David Kautter, the Treasury Department’s assistant secretary for tax policy and the acting I.R.S. commissioner.
But other companies that have failed to provide insurance will face stiff fines.
“I think it is horribly unfair and unjust,” Representative Jody Hice, a Republican from Georgia who has been a leading voice in the opposition to the employer mandate, said at a hearing where Mr. Kautter testified in April. “What I am asking at this point is for the I.R.S. to continue not to enforce it, as is what took place under the Obama administration,” he said, referring to a reprieve that was granted while businesses and the government sorted out compliance details.
Some lawyers contend that the I.R.S. is on shaky ground in trying to enforce the employer mandate penalties, arguing that the government has not followed proper procedures, like notifying employers that they were in violation of the law.
“The Affordable Care Act and federal regulations clearly state that a health insurance exchange must notify an employer that one or more employees qualified for premium tax credits before the I.R.S. can impose penalties,” said Christopher E. Condeluci, an employee benefits lawyer. “Most of the employers subject to penalties for 2015 never received the notices required under the law.”
E. Neil Trautwein, a vice president of the National Retail Federation, said some penalties resulted from an employer’s failure to check a particular box on a government form indicating that it had offered coverage to eligible employees.
In one case, Mr. Trautwein said, a $20 million penalty was imposed on a restaurant chain because one of its vendors had failed to check the proper box. “The penalty was negotiated down to zero,” Mr. Trautwein said. “It was an inadvertent mistake in filling out a complicated new form.”
John D. Arendshorst, an employee benefits attorney at Varnum, said he has been busy fielding questions from companies that have received proposed assessments from the I.R.S. and said the government has shown a willingness to reduce penalties when appropriate. In one case, a business with about 500 employees received an assessment for $1.9 million. That was ultimately reduced to $20,000 because the penalty was caused by a computer error.
“They were shocked for sure,” Mr. Arendshorst said of the initial penalty letter. “They felt it was a big mistake and it turned out to be.”
Under the Affordable Care Act, the employer mandate was to take effect in 2014. The Obama administration delayed enforcement for an additional year after employers said they needed more time to comply with rules requiring them to report on the coverage they provided to employees. And the Treasury Department needed more time to clarify the requirements. It was not until late last year that the I.R.S. had the capacity to determine which businesses were in violation of the mandate, and the agency is just now sending penalty letters related to the 2015 tax year. Penalty letters for the 2016 and 2017 tax years are expected to follow soon.
Republicans criticized the decision to begin enforcing the mandate as a parting shot by the former I.R.S. commissioner John Koskinen, whom they had previously assailed over the agency’s scrutiny of conservative nonprofit organizations. While Mr. Trump had issued an executive order that called for easing the Affordable Care Act’s regulations, the Treasury Department, which oversees the I.R.S., said it was required to abide by the law and enforce the employer mandate.
Mr. Koskinen pushed back against the idea that he was attempting to punish conservatives by jump-starting enforcement of the employer mandate, and he said that companies had been given plenty of notice that they needed to provide insurance to their employees.
“The I.R.S. does not have the authority not to collect the money,” Mr. Koskinen said in an interview, adding that there was no reason to hold off on penalizing companies. “Delaying wouldn’t accomplish anything except delay.”
Business groups have been lobbying Congress to repeal the employer mandate or to get the I.R.S. to stop enforcing it. They argue that companies did not receive sufficient notice that they needed to comply with a provision of the health law that had not been enforced for seven years.
“The employer mandate always existed to support the individual mandate,” said Jim Klein, president of the American Benefits Council. “There’s no logic or fairness in having an employer mandate in the absence of having an individual mandate.”
Mr. Klein said he would like to see a legislative fix to address the situation.
Mr. Trump himself has added to the confusion over the mandate by repeatedly asserting that the Affordable Care Act had been essentially eliminated because Republicans did away with the individual mandate.
“It’s yet another reason why the employer mandate needs to go,” Representative Kevin Brady of Texas, the Republican chairman of the House Ways and Means Committee, said of the penalties.
https://www.beckershospitalreview.com/finance/kaiser-s-operating-income-climbs-to-1-1b-in-q1.html

Oakland, Calif.-based Kaiser Permanente reported higher revenues and operating income for its nonprofit hospital and health plan units in the first quarter of 2018, according to recently released financial documents.
Kaiser saw revenues increase to $20.3 billion in the first quarter of this year. That’s up about 12 percent from revenues of $18.1 billion in the same period of 2017.
The boost was attributable in part to the system’s health plan unit. Since Dec. 31, Kaiser has added approximately 472,000 health plan members. As of March 31, Kaiser had about 12.2 million members.
Kaiser reported operating income of $1.1 billion in the first quarter of this year, up from $1.04 billion in the same period of 2017.
After factoring in nonoperating income, which declined year over year, Kaiser ended the first quarter of 2018 with net income of $1.4 billion. That’s compared to the same period of 2017, when the organization reported net income of $1.6 billion.


