https://gisthealthcare.com/weekly-gist/

Here’s a question we get all the time, and one that I heard again this week from one of our partner health systems: “We’re working on [initiative X]. What have other health systems like us done about that?” We hear it in any number of situations, from hospitals developing clinical protocols to strategic planners putting together business plans for service line growth. Sometimes the question comes in different forms: “Do you have a white paper on [topic X]?”; or “What research do you have on [issue X]?”; or our favorite, “What’s the best practice for [activity X]?”
It’s not surprising, given our past history, that we’d frequently be asked to provide research or best practice information. But as we’ve grown our own business at Gist Healthcare and developed our own independent perspective on where our industry needs to go, we’ve become less and less impressed by “best practice” as a concept. In fact, I’d go so far as to say that “best practice” has become at best a crutch, and in many cases a hindrance, to real progress in healthcare. As we sometimes tell our clients now, healthcare has outgrown “best practice”, at least as we used to understand it.
Don’t get me wrong. Medicine should absolutely be evidence-driven, and clinical care should always be firmly grounded in proven practice. If anything, the actual clinical practice of medicine is one area where our industry must become more, not less, best-practice based.
But as to system strategy, payment innovation, service improvement, and a host of other business and operational issues, simply imitating what other “successful” organizations are doing leads inevitably to reversion to the mean, groupthink, and (most troubling) fad-driven “bubbles” of activity. It’s no surprise, given the pervasive culture of “best practice”, when suddenly every health system’s top priority turns to creating a patient portal, or hiring a chief experience officer, or starting a proton beam center, or opening freestanding EDs.
Healthcare delivery is a highly fragmented, insular business, with little visibility across markets and across institutions. That makes it very susceptible to white paper-driven trend chasing, which tends to outsource innovation to the “wisdom of the crowd”.
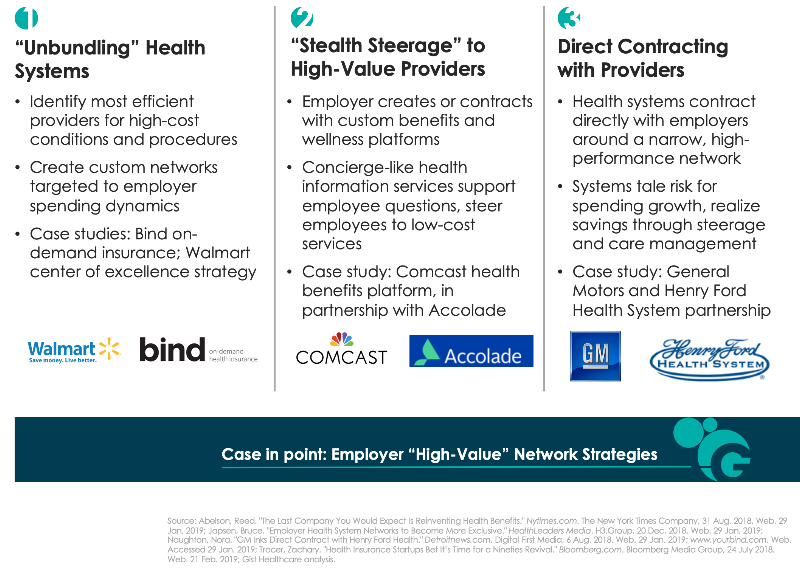
It’s pretty rare to find mavericks, following their own innovation instincts without getting caught up in trying to mimic what other “leaders” are doing. That’s why when a delivery organization takes a risk on a truly new strategic innovation—Geisinger’s money-back guarantee, Cleveland Clinic’s promise of same-day access, Presbyterian’s direct contract to manage Intel employees’ health—it immediately sends shock waves across the industry.
Those ideas didn’t come from a white paper. We’re often asked whether we’re building a “best-practice research” capability in our new company. While we’re not quite ready to talk about our upcoming service offerings, the answer to that question is a definitive “no”.