http://www.healthcarefinancenews.com/news/benefits-bankruptcy-how-one-hospital-found-redemption-chapter-11?mkt_tok=eyJpIjoiWkRObE1XWmhNemt3TjJFNCIsInQiOiJuWXNFaDk2M2RINGpwRlZ6ck1oekJyVkg0clVSUjlQek9TUExrdVVYUlNubjAzU2pkS0FtNndPODc0dVpBaTkvUEFKd05aK01mMXp6dDc5NzVTNDVQZmVZWmFXTjFCd08xMnRKWGljZzNGTEFPSHFIY21UT1Y2TnYwTk5QWWVGUCJ9

Filing for bankruptcy might make hospital finance executives cringe with desperation, if not failure, but strategically pursuing Chapter 11 can actually lay the foundation for a brighter future.
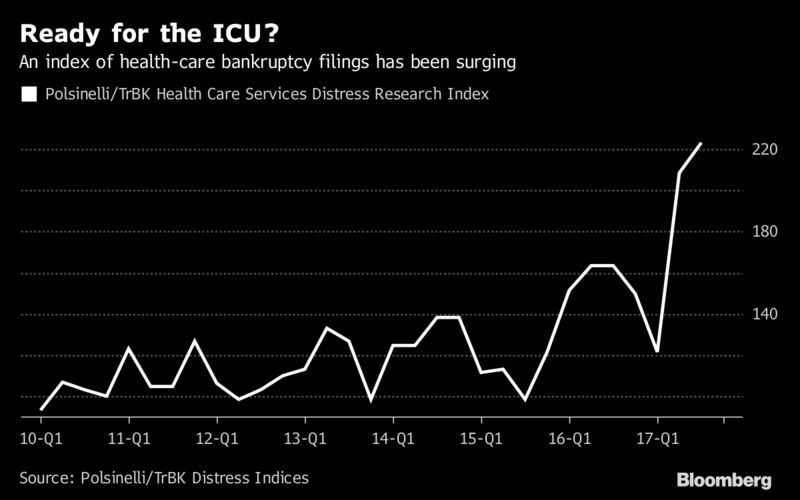
In fact, Morehead Memorial Hospital in Eden, North Carolina, actually owes its future to its leader’s decision to file for Chapter 11. Like so many rural hospitals, whose ranks are shrinking fast, Morehead faced common problems including flat or declining populations, migration of patients who find work in other communities and get care there, as well as the prevalence of Medicare and Medicaid in payer mixes that cause financial losses and vulnerabilities.
The albatross: Old debt
Morehead CEO Dana Weston’s original inclination was to look for a buyer, but after a year of searching a realization sunk in: the large amount of debt attached to the hospital was a liability akin to a brick wall between Morehead and a path forward.
Weston said they got consistent feedback that organizations felt it wasn’t in their current strategy to acquire a struggling rural hospital, since many systems already have more than one such facility under their umbrella. Most of the debt was at least a decade old, and addressing it was really the only way to make themselves attractive to potential buyers.
So Weston and the executive team did something that sounded more like an end than a beginning: Morehead filed for Chapter 11 bankruptcy on July 10.
Navigating Chapter 11, especially for a struggling rural hospital with limited resources and personnel must be done properly for the strategy to succeed.
And Morehead had some unique complexities, according to Ron Winters, managing director of hospital and healthcare services management firm Healthcare Management Partners. Winters has followed Morehead’s case and pointed out that the hospital is near a state border so they deal with different insurers from other states and are within 90 minutes of several larger competing hospitals, which didn’t help. Even worse, the size and scope of the their complex debt picture, including a $34 million U.S. Department of Housing and Urban Development loan that offered limited flexibility on repayment, really limited their options, Winters said.
“You couldn’t just go to HUD and say let’s make a deal,” Winters explained. “You needed the bankruptcy code to make a transaction happen.”
That’s because when a hospital enters bankruptcy, Winters said it is effectively drawing a line in the sand on the very day it files. Chapter 11 code dictates that any obligation incurred after the petition date is superior to anything owed prior to the petition date. So new debt legally takes priority over old in terms of what will be covered by proceeds from a transaction. Moreover, bankruptcy rules state that any buyer that acquires an entity that went through chapter 11 proceedings is assured no creditor can come after them for the acquired hospital’s debt. They only pay what they agreed to for the transaction, providing security and alleviating risk.
Eliminating the risk of old debt is the precise upside Morehead leveraged to make itself attractive to a prospective buyer.
Common misperceptions
The phrase Chapter 11, and this is true in any industry, hits an organization’s reputation pretty hard.
The legalese is hard to translate to employees and the community, and Weston said the sale of assets, which is how their bankruptcy transaction is referred to, caused quite a stir because it sounded like a liquidation.
“People had this picture in their mind of an auction where the furniture, equipment, everything was just gonna be sold off to the highest bidder,” Weston said. “That’s not the case at all.”
She insisted that the board’s decision to file for Chapter 11 was the right one because it removed one of the major barriers to interest in buying Morehead by addressing the debt through bankruptcy and shedding that liability.
Without a partner, Morehead simply had no future.
Avoiding bankruptcy’s downside
Winters warned that there is a risk to bankruptcy and two main drawbacks are costs and the consequences of not being prepared with a plan. First, a debtor must hire a bankruptcy lawyer and other experts such as a patient care ombudsman to monitor the care provided to patients and look after patient rights. If a hospital doesn’t have available assets to pay for those things, that’s a problem.
“It’s ideal to have some unpledged assets to use as liquidity for the proceedings or have a buyer lined up the very first day,” Winters said.
Having a buyer lined up on the first day would seem an ideal scenario, and is called a stalking horse purchaser. Bankruptcy code provides that a debtor must create protections so that the stalking horse can’t be easily outbid or outbid at all. A winning bidder that beats the stalking horse must do so by a minimum amount, for instance, and reimburse them for costs related to establishing stalking horse status.
Without a buyer ready to go or other financing plans laid out, creditors get worried, Winters said. “With financing, your creditors should be satisfied that all obligations following the bankruptcy petition will be satisfied.”
Hospitals would do well to start thinking about options like seeking a partner or bankruptcy while they still have some amount of liquidity and unpledged assets. “When you have none left you’re not going to be able to drive an attractive transaction and you run the greatest risk of collapsing,” Winters said.
The new future
Weston’s plan worked and Morehead’s survival is now all but assured.
On Nov. 13, a federal bankruptcy judge chose UNC Health Care as the winning bidder for Morehead, setting a course for emergence from Chapter 11 for early 2018.
The closing is expected to take 60 days, and Morehead will operate as usual during the transition. UNC personnel will be visiting Morehead in the coming weeks to start building relationships with hospital staff and the community.
Collapsing was never an option, according to Weston. The first-time CEO said there was far too much at stake. She said what keeps her up at night are the employees at Morehead and the community it serves. The hospital is vitally important to its hometown and to Rockingham County. It’s the biggest employer in Eden and the 4th or 5th largest in the county.
“The most valuable thing for me in this role is for the 700 who work here to trust that I am in this with them,” Weston said. “This community is my family.”