WASHINGTON — If President Trump allows states to convert Medicaid into a block grant with a limit on health care spending for low-income people, he will face a firestorm of opposition in Congress, House Democrats told the nation’s top health official on Tuesday.
The official, Alex M. Azar II, the secretary of health and human services, endured more than four hours of bipartisan criticism over the president’s budget for 2020, which would substantially reduce projected spending on Medicaid, Medicare and biomedical research. Democrats, confronting Mr. Azar for the first time with a House majority, scorned most of the president’s proposals.
But few drew as much heat as Mr. Trump’s proposed overhaul of Medicaid. His budget envisions replacing the current open-ended federal commitment to the program with a lump sum of federal money for each state in the form of a block grant, a measure that would essentially cap payments and would not keep pace with rising health care costs.
Congress rejected a similar Republican plan in 2017, but in his testimony on Tuesday before the Health Subcommittee of the House Energy and Commerce Committee, Mr. Azar refused to rule out the possibility that he could grant waivers to states that wanted to move in that direction.
Under such waivers, Mr. Azar said, he could not guarantee that everyone now enrolled in Medicaid would keep that coverage.
“You couldn’t make that kind of commitment about any waiver,” Mr. Azar said. He acknowledged that the president’s budget would reduce the growth of Medicaid by $1.4 trillion in the coming decade.
Representative G. K. Butterfield, Democrat of North Carolina, said that “block-granting and capping Medicaid would endanger access to care for some of the most vulnerable people” in the country, like seniors, children and the disabled.
Mr. Trump provoked bipartisan opposition by declaring a national emergency to spend more money than Congress provided to build a wall along the southwestern border. If the president bypasses Congress and allows states to convert Medicaid to a block grant, Mr. Butterfield said, he could face even more of an outcry.
“You just wait for the firestorm this will create,” Mr. Butterfield said, noting that more than one-fifth of Americans — more than 70 million low-income people — depend on Medicaid.
As a candidate, Mr. Trump said he would not cut Medicare, but his new budget proposes to cut more than $800 billion from projected spending on the program for older Americans in the next 10 years. Mr. Azar said the proposals would not harm Medicare beneficiaries.
“I don’t believe any of the proposals will impact access to services,” Mr. Azar said. Indeed, he said, the cutbacks could be a boon to Medicare beneficiaries, reducing their out-of-pocket costs.
After meeting an annual deductible, beneficiaries typically pay 20 percent of the Medicare-approved amount for doctor’s services and some prescription drugs administered in doctor’s offices and outpatient hospital clinics.
Mr. Azar defended a budget proposal to impose work requirements on able-bodied adults enrolled in Medicaid. Arkansas began enforcing such requirements last year under a waiver granted by the Trump administration. Since then, at least 18,000 Arkansans have lost Medicaid coverage.
Mr. Azar said he did not know why they had been dropped from Medicaid. It is possible, he said, that some had found jobs providing health benefits.
Representative Joseph P. Kennedy III, Democrat of Massachusetts, said it would be reckless to extend Medicaid work requirements to the entire country without knowing why people were falling off the rolls in Arkansas.
If you are receiving free coverage through Medicaid, Mr. Azar said, “it is not too much to ask that you engage in some kind of community engagement.”
Representative Fred Upton, Republican of Michigan, expressed deep concern about Mr. Trump’s proposal to cut the budget of the National Cancer Institute by $897 million, or 14.6 percent, to $5.2 billion.
Mr. Azar said the proposal was typical of the “tough choices” in Mr. Trump’s budget. He defended the cuts proposed for the National Cancer Institute, saying they were proportional to the cuts proposed for its parent agency, the National Institutes of Health.
The president’s budget would reduce funds for the N.I.H. as a whole by 12.6 percent, to $34.4 billion next year.
Mr. Azar was also pressed to justify Mr. Trump’s proposal to cut federal payments to hospitals serving large numbers of low-income patients. Representative Eliot L. Engel, Democrat of New York, said the cuts, totaling $26 billion over 10 years, would be devastating to “safety net hospitals” in New York and other urban areas.
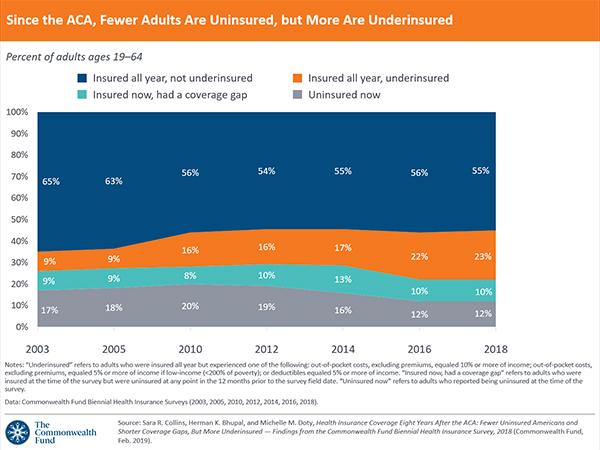
Mr. Azar said that the Affordable Care Act, by expanding coverage, was supposed to “get rid of uncompensated care” so there would be less need for the special payments.
While Democrats assailed the president’s budget, Mr. Azar relished the opportunity to attack Democrats’ proposals to establish a single-payer health care system billed as Medicare for all.
Those proposals could eliminate coverage provided to more than 20 million people through private Medicare Advantage plans and to more than 155 million people through employer-sponsored health plans, he said.
But Mr. Azar found himself on defense on another issue aside from the president’s budget: immigration. He said he was doing his best to care for migrant children who had illegally entered the United States, were separated from their parents and are being held in shelters for which his department is responsible.
He said he was not aware of the “zero tolerance” immigration policy before it was publicly announced in April 2018 by Attorney General Jeff Sessions. If he had known about the policy, Mr. Azar said, “I could have raised objections and concerns.”
Representative Anna G. Eshoo, Democrat of California and the chairwoman of the subcommittee, summarized the case against the president’s budget.
“The Trump administration,” she said, “has taken a hatchet to every part of our health care system, undermining the Affordable Care Act, proposing to fundamentally restructure Medicaid and slashing Medicare. This budget proposes to continue that sabotage.”