
Cartoon – The Corporate Trust



On June 20, 2018, CMS and HHS issued a “request for information” (RFI) seeking input on strategies to reduce the burden of the federal physician self-referral law or “Stark Law,” including the law’s impact on the transition to value-based care.
In the RFI, CMS solicits information on the ways in which the Stark Law creates challenges for coordinated, value-based care, and the transition to alternative payment and delivery models; it also seeks ideas and input on how the Stark Law may be changed to facilitate these models.
What’s driving the RFI
The RFI is launched as part of the agency’s “Regulatory Sprint to Coordinated Care” led by HHS Deputy Secretary Eric Hargan, which is directed at addressing regulatory barriers to coordinated care. As such, the Regulatory Sprint and the RFI represent the administration’s efforts to reduce regulatory burden, while also demonstrating a commitment to the transition to more value-based, coordinated care and risk-based payment. In public statements, HHS and CMS officials have suggested that the Regulatory Sprint may support similar flexibility in other laws, including the Anti-Kickback Statute.
Although the agency does not commit to any specific regulatory changes in this document, it is notable that HHS issued a similar RFI in 2010 just before it issued sweeping waivers of the Stark Law and Anti-Kickback Statute for the Medicare Shared Savings Program. While many of the questions focus on “Alternative Payment Models” under the Quality Payment Program, the RFI is not limited to these programs. Instead, the RFI invites the public to propose new exceptions and revised interpretations of the statute to advance the goals of coordinated care.
What CMS wants to know
In the RFI, CMS poses twenty specific questions related to the Stark Law, Alternative Payment Arrangements, and delivery system innovation strategies. The topics and questions range from:
The RFI may represent an important opportunity for the healthcare industry to educate CMS on current experiences and challenges, and to shape the content of future rules implementing changes to the Stark Law, particularly in a time of industry integration across the continuum of care. The RFI also offers tangible evidence of the administration’s commitment to continue a migration to value-based care, and potentially reflects an enhanced commitment and desire to migrate away from fee-for-service payment to arrangements involving financial risk.

Value-based payment (VBP) models are an effort to rein in the growth of health care costs and improve quality. However, it’s unclear what overall impact VBP models are having on health care costs. Even though health care is provided at the local level, most evaluations examine health care spending at the national level. To address this disconnect, we conducted quantitative and qualitative market-level assessments. Our goals were to examine the impact of population-based, value-based care within a market; identify what measurable factors were associated with differing costs; and understand how business leaders are thinking about value-based care and cost reduction.
Leavitt Partners, the Healthcare Financial Management Association (HFMA), and McManis Consulting, with participation from Mark McClellan at Duke University, conducted three mixed-methods studies:
Key findings from the studies include:
VBP dates back to 2005 with the Physician Group Practice Demonstration. The Affordable Care Act (ACA) significantly accelerated the proliferation of VBP models with the creation of the Medicare Shared Savings Program(MSSP) and the Center for Medicare and Medicaid Innovation, which was tasked with developing and testing innovative new models. Commercial VBP arrangements have also taken hold in the years since the ACA’s passage.
Given the growth of VBP, we wanted to examine whether, in the first few years following the ACA, these models were influencing the total cost of care. We used Medicare data from 2012 to 2015 and commercial data from 2012 to 2014 to assess the early impact of these models. We restricted our study to population-based VBPs, which included models with upside risk only (shared savings), both upside and downside risk, and global budgets, but excluded episode-based (bundled) payments.
We did not find a statistical relationship between the level of penetration of population-based VBPs in a market and a decline in health care costs for Medicare or commercial payers. Nor did we find an improvement in quality. When we limited our analysis to just those markets with higher levels of population-based VBP penetration (at least 30 percent), our results suggested a very modest, not statistically significant, market-level decrease in cost growth. Despite this null finding, our results provide an important baseline for future research.
There are several potential explanations for the null findings. For one, our study period (2012–15) may simply have been too early to see signs of population-based VBP lowering health care costs. Although today 561 MSSP accountable care organizations (ACOs) (the largest of Medicare’s ACO programs) cover 10.5 million beneficiaries, at the beginning of our study period in 2012 and 2013, only 220 MSSP ACOs covered 3.2 million beneficiaries. Many interviewees told us not enough lives were covered under VBP. Indeed, in some markets, less than 1 percent of lives were part of a VBP arrangement.
Second, although participation in population-based VBP models is growing, few models involve the provider taking on downside risk. As of 2018, the majority (82 percent) of MSSP ACOs were in the non-risk-bearing Track 1, which means they share in savings if they spend less money than their assigned benchmark, but they will not incur financial losses if they spend more than the benchmark. Our site visits found that although different markets had varying levels of population-based VBP activity, no market had significant numbers of providers participating in downside risk. Several interviewees stressed the need to take incremental steps to more risk.
Fee-for-service payment remains quite profitable for many providers and health systems. Even for those that have begun to take on risk-based contracts, fee-for-service payment represents the majority of total revenue. As long as the status quo remains lucrative, it’s difficult to make the business case for why a provider should undertake the effort to switch to a value-based focus that may lead to a reduction in use and total revenue.
Still, several interviewees said they believed the move toward paying for value would continue, even if there’s some uncertainty over whether Medicare or private payers will lead the movement. It’s possible that when VBP models outweigh fee-for-service payments in a market, we’ll reach a “tipping point” and health care cost growth will decline. Many interviewees expressed enthusiasm for other VBP models, such as those based on episodes of care (bundled payments) and those designed for specific populations (for example, the frail elderly). These models may make more sense for specialty providers who perform a certain type of procedure or care for a certain type of patient.
If these initial population-based VBPs results don’t show a relationship to health care cost growth, then which market-level factors do correlate? For our second quantitative analysis, we used a variety of public and private data sources to examine the relationship among several market-level factors beyond value-based payment and Medicare costs and cost growth between 2007 and 2015. All the factors together explained 82 percent of variation in baseline Medicare costs (Exhibit 1).
The prevalence of chronic diseases was the most influential predictor of market costs, accounting for 41.5 percent of the variance. Hospital quality metrics, market socioeconomic status, and the concentration of hospitals and insurers also helped explain market-level costs.
Using these same factors to predict Medicare cost growth was less fruitful, explaining only 27 percent of the variation in Medicare cost growth—substantially less than the 82 percent of baseline costs. As Exhibit 2 shows, a much weaker association exists between chronic disease prevalence and Medicare cost growth. Significant additional research should be done to identify factors that predict cost growth.
These findings matter for several reasons. First, they reinforce efforts currently underway to contain costs, including strategies to prevent and better manage chronic conditions, reduce hospital readmissions, and reduce the number of individuals without insurance. Second, although we know less about what drives health care cost growth in a market, meaningfully reducing spending in a market relies on developing strategies that target cost growth, instead of baseline costs. More research that focuses on what’s driving cost growth is needed.
The interviews we conducted add insights into these market-level findings. We identified two distinguishing characteristics of higher- and lower-cost markets: type of competition in the market and degree of transparency in the market. We recognize that while there are some common lessons, health care markets differ significantly and their approaches to care, costs, and VBP models will vary.
We know competition can help drive down costs and increase quality in health care markets. However, how much competition, and what type, seems to make a difference. For example, we found that the lower-cost markets in our nine site visits had at least one integrated delivery system. Consolidation in these markets had resulted in two to four health systems with geographic coverage across the market. In these markets, physicians were generally employed by the health system or worked in close alignment with it. Health plan competition matters as well, particularly with respect to innovation in new payment and care delivery models. Portland, Oregon, and Minneapolis-St. Paul, Minnesota, two of the lowest-cost markets, both had competitive health plan landscapes.
Conversely, the markets we visited with less integration and seemingly more provider competition actually had higher costs. These included Los Angeles, California (which had higher Medicare costs only), Baton Rouge, Louisiana, and Oklahoma City, Oklahoma. One reason for this may be that there is less focus on addressing unnecessary use in these markets.
Transparency is often cited as a strategy that will help contain costs. Similar to competition, the type of transparency effort matters. We found that some lower-cost markets seemed to benefit from organized transparency mechanisms, including state-sponsored or endorsed reporting agencies and employer coalitions that made information on provider quality and costs publicly available. For example, in 2005, the Minnesota Medical Association and health plans in the state together formed MN Community Measure, a nonprofit organization tasked with the collection and dissemination of data on the quality and cost of providers across the state. Today, providers are required to submit data to the organization. Our interviewees expressed optimism but acknowledged more work is needed to optimize consumer-oriented transparency tools, which research has so far shown to have had only minimal use.
Our research led us to three primary policy recommendations to help improve health care quality and lower costs (for additional ones, see the fullstudies).
Although differences exist among each health care market, all markets can act to improve quality and reduce costs. Our studies suggest several actions different stakeholders in each market can take to improve care for their populations.
Spin Belongs in The Gym, Not The Workplace – 4 Ways to Increase Transparency

I have a motto when it comes to honesty and transparency at work: Spin belongs in the gym, not the workplace.
Spinning the truth is a way of shaping our communications to make our self, the company, or the situation appear better than it is in reality. It’s become so commonplace in the corporate world that many times we don’t even realize we’re doing it. We “spin” by selectively sharing the facts, overemphasizing the positive, minimizing the negative, or avoiding the obvious, all in an attempt to manipulate the perception of others. See if a few of these spins on the truth sound familiar:
Spinning the truth is one of the most common ways leaders bust trust. It also leads to tremendous inefficiencies because people are confused about roles, they duplicate work, balls get dropped, and people resort to blaming others. Poor morale, cynicism, and political infighting become the norm when honesty and transparency are disregarded.
There are macro-level societal events and trends driving the need for greater transparency in the workplace. We’re all familiar with the digital privacy concerns related to the pervasiveness of technology in our lives, and we’ve witnessed the corporate scandals of blatant deceit and dishonesty that’s contributed to record low levels of trust. The global meltdown of trust in business, government, and other institutions over the last several years has generated cries for more transparency in communications, legislation, and governance. Oddly enough, research has shown that in our attempts to be more transparent, we may actually be suffering an illusion of transparency—the belief that people are perceiving and understanding our motivations, intents, and communications more than they actually are.
But at the individual, team, and organization levels, what can we do to build greater trust, honesty, and transparency? I have four suggestions:
Spin is a great activity for the gym and it keeps you in fantastic shape. However, in the workplace, spin is deadly to your health as a leader. It leads to low trust, poor morale, and cynicism in your team. Keep spin in the gym and out of the workplace.

https://www.huffingtonpost.com/entry/opinion-beggelman-price-gouging_us_5ab45270e4b008c9e5f5c47f

It’s hard to remember now, but there once was a time when pharmaceutical companies were considered heroes, not villains.
In the 1920s, Dr. Frederick Banting and Charles Best discovered insulin could be purified and administered to diabetes patients via injection. Before this groundbreaking discovery, people living with diabetes were placed on starvation diets as a form of treatment, and many patients died.
Banting and Best understood the enormity of their discovery and considered insulin a public good. But as these researchers soon realized, insulin wouldn’t be able to save lives if patients couldn’t access it. They sold the rights to the drug to the University of Toronto for $1. The university, in turn, gave it to pharmaceutical company Eli Lilly for a 5 percent royalty so the company could manufacture at scale to meet the enormous demand. In 1923, insulin became widely available and saved countless lives, thanks to Banting and Best – and Eli Lilly.
Now, just under a century later, Eli Lilly and other insulin manufacturers are taking the exact opposite approach.
Big Pharma is pushing every scheme imaginable to squeeze money from the pockets of patients who need insulin to survive. Many with diabetes, faced with tripling insulin prices ($200 to $700 per month), are now forced to choose between life and rent. Some patients ― like 26-year-old Alec Raeshawn Smith, who aged out of his parents’ health insurance plan and whose job didn’t offer comprehensive coverage ― have died from a lack of affordable insulin.
Pharmaceutical companies can become heroes again, but only if they stop taking advantage of the patients who need them.
Eli Lilly says the company strives “to make life better for all those affected by diabetes around the world.” And because drug companies do save and improve lives (or, at least, are supposed to), the U.S. government allows them special privileges and protections. This includes tax breaks, government subsidies, extensive patent protection, free access to publicly funded scientific discoveries and more.
However, when drug companies use empty words to make promises they have no intentions of honoring, they do not deserve the public’s largesse.
Big Pharma has not shown any inclination to change its price gouging practices. On the contrary, drug companies continue to push higher costs despite the horrific impact this has both on human life and the U.S. economy. Price freezes in the U.S. are rare (and are exclusively voluntary). They also tend to be set at high levels, like the price “freeze” for the HIV drug Isentress, which caused a stir among HIV patients because of its exorbitant cost compared to competitive products.
Some companies have rolled back drug prices but typically only in response to public humiliation. Doctors at Memorial Sloan-Kettering publicly rejected Sanofi’s Zaltrap, a colon cancer drug, because it was priced twice as high as a competing product. Three weeks after the doctors’ announcement, Sanofi cut its price in half. This is why consumers shouldn’t be satisfied with price freezes; only rolling back prices will return us to reasonable drug costs.
Pharmaceutical companies do sometimes offer “solutions” to runaway drug prices, like value-based pricing and discount cards, but though these practices may help some, they are generally gimmicks meant to distract the public. Value-based pricing sets prices according to a drug’s perceived value rather than according to the actual costs of developing and manufacturing it. Such a practice can put a limit on the price of marginally effective drugs, but on the other hand, it increases the price of medications like insulin ― drugs that save lives but have been around for years and are cheap to produce. Discount cards are sometimes offered to a small subset of insured patients and do very little to help the vast majority of users or those who need the drugs most.
In the U.S., our 20 top-selling medications cost consumers three times more than the exact same drugs cost in Britain. I once paid $36 for a medication in Canada that costs me more than $700 here at home. In many European countries, government committees calculate “reference prices” for classes of drugs with similar ingredients, based on the costs to develop and manufacture them and their clinical effectiveness. That said, it’s probably not realistic to expect our politicians to agree to this kind of approach; in the U.S., pharmaceutical companies are some of the largest contributors to political campaigns, giving more than $2.3 billion over the past 10 years.
Big Pharma is pushing every scheme imaginable to squeeze money from the pockets of patients who need insulin to survive.
Our legislators, too afraid to challenge Big Pharma’s pocketbooks, continue to propose tepid solutions, like price transparency, that only work around the edges. Pharmacy benefit managers ― the industry middlemen who play a role in drug pricing ― take a piece of the pie, but how large a piece remains a secret. Legislation around transparency regarding undisclosed PBM deals could drive down drug prices somewhat, but it likely wouldn’t affect the baseline prices set by drug manufacturers.
The Right Care Alliance ― a group of patients, physicians, nurses, patient advocates, students and other community members with chapters around the country ― is currently organizing a campaign to target price gouging in the pharmaceutical industry. We are planning year-long grassroots actions, including town hall meetings, marches and demonstrations, to pressure Big Pharma to stop predatory pricing, particularly for life-saving medications.
We must force companies like Eli Lilly to address the gap between what they say they stand for and their actions. We must be loud with our demands to counterbalance the hold Big Pharma has on U.S. politics. Drug companies can become heroes again but only if they stop taking advantage of the patients who need them.

Dallas-based Tenet Healthcare announced March 5 that its board of directors has approved several changes to the company’s corporate governance.
Here are five things to know about the changes.
1. The board approved changes to Tenet’s bylaws that allow shareholders with a 25 percent stake in the company to request a special meeting. The move comes after the board approved amendments to the company’s bylaws in January that allowed majority shareholders to request special meetings.
2. Tenet approved a short-term shareholder rights plan in August 2017, which was designed to protect $1.7 billion in net operating loss carryforwards and ensure the board could protect all shareholder interests as it executed CEO and board changes. Under the poison pill, if any person or entity acquired 4.9 percent or more of Tenet stock, all holders of rights issued under the plan are entitled to acquire shares of common stock with a 50 percent discount.
3. Tenet terminated the poison pill March 5. “The board made this decision based upon the reduced value of the NOL shareholder rights plan following recent tax law changes and an increase in the company’s stock price since the NOL shareholder rights plan was adopted, as well as shareholder feedback,” Tenet said in a statement. The poison pill was originally slated to expire following Tenet’s 2018 annual meeting of stockholders, which is typically held in May.
4. Tenet announced March 5 that it also eliminated the executive committee as a standing committee of the company’s board of directors.
5. “The board of directors and management have spent considerable time in recent weeks engaging with shareholders representing a majority of our outstanding stock and we received constructive input regarding Tenet and our objective to lead with best corporate governance practices,” said Ronald A. Rittenmeyer, executive chairman and CEO of Tenet. “We believe the actions which we are taking today demonstrate our continued commitment to being responsive in a timely manner to shareholder feedback and to implementing measures that increase transparency and accountability.”
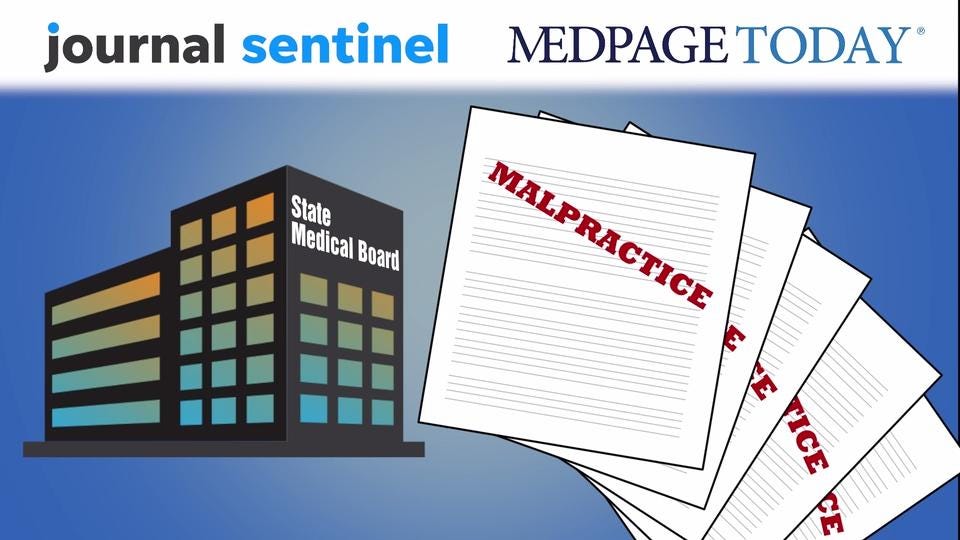
Like traveling medicine hucksters of old, doctors who run into trouble today can hopscotch from state to state, staying ahead of regulators.
Instead of snake oil, some peddle opioids. Others have sex with patients, bungle surgeries, misdiagnose conditions or are implicated in patient deaths.
Even after being caught in one state, they can practice free and clear in another; many hold a fistful of medical licenses.
Stories about individual doctors avoiding discipline in a second state have been reported before. An investigation by the Milwaukee Journal Sentinel and MedPage Today shows how widespread the problem is: At least 500 physicians who have been publicly disciplined, chastised or barred from practicing by one state medical board have been allowed to practice elsewhere with a clean license.
And their patients are kept in the dark — even as more become victims — thanks to an antiquated system shrouded in secrecy.
In Colorado, Gary Weiss’ care of a multiple sclerosis patient prompted four doctors to complain to the state medical board when the patient died in 2011. The board and Weiss agreed that he was “permanently inactivating” his license in 2014, meaning he could never get it back.
But in Florida, where Weiss has a long-standing practice, officials applied no restrictions despite malpractice lawsuits from seven other patients in two states, all accusing him of misdiagnosing them with multiple sclerosis.
Plastic surgeon John Siebert had sex with a patient in New York, got his license suspended for three years and was permanently ordered to have a chaperone in the room with any female patients. But he operates free of medical board restrictions in Wisconsin. In fact, he was appointed to an endowed chair at the University of Wisconsin-Madison, funded in part by billionaire Diane Hendricks, a patient and a major political contributor to Gov. Scott Walker.
Look up Jay Riseman on the website of the Division of Professional Registration in Missouri, where he practices as a hospice doctor: It lists no disciplinary history, no red flags.
But in Illinois, where a medical board official once called him an “imminent danger to the public,” the families of three patients who died remain haunted by what he did. Riseman continues to practice, despite having prescribed massive amounts of pre-surgery laxatives to infants and failing to act in the case of an older woman with a blood infection.
Among the more than 500 doctors identified by the Journal Sentinel and MedPage Today, the single biggest reason for board action was medical errors or oversights. One fifth of the cases were a result of putting patients in harm’s way.
All have slipped through a system that makes it difficult for patients, employers and even regulators in other states to find out about their troubling pasts.

As CEO incentive pay packages bring attention to transparency issues in executive compensation, a group of directors and chief risk officers from The Directors and Chief Risk Officers Group published a set of guiding principles for compensation committees around the governance of risk related to pay and performance.
The report aims to give a company’s board of directors and board-level compensation committees guidelines for the governance of risks linked to an organization’s compensation culture.
Here are 10 guidelines for compensation committees to best guide executive pay and performance, according to the report.
1. Compensation committees must fulfill both direct and indirect pay governance responsibilities to define the best compensation culture for the company. Under direct governance responsibilities, CEOs must establish and continually review company-wide compensation philosophy. To fulfill indirect pay governance responsibilities, a company’s executives must ensure adequate resources and processes are in place for the organization’s incentive plans.
2. Committees should emphasize incentive pay for corporate performance when designing and communicating the company’s compensation philosophy. Incentive pay for an individual’s performance must be carefully applied when it is appropriate to fulfilling the individual’s role.
3. A CEO’s total compensation should be driven by how they impact the long-term interests of the company, which includes how effectively the organization takes risk.
4. A company should minimize use of external benchmarking, or the comparison of its statistical data with other organizations in the same industry, for executive pay. Instead, companies should work to incorporate internally-focused pay evaluation for executive pay.
5. Incentive-based compensation should always be considered to be “at risk,” subject to deferral periods and influenced by the company’s long-term performance.
6. Compensation committees must continually use discretion in determining an executive’s final incentive pay package. In this way, committees must make rules for determining these pay packages subject to discretionary override when the compensation culture of the organization appears to be violated.
7. When considering performance reviews and compensation design for an organization’s CEO and individuals in the succession plan, the compensation committee must provide complete transparency to the entire board. This includes the board’s approval of full details of the CEO’s performance and any final awards given to the executive.
8. Compensation committees should obtain public certification that ensures their processes of governing pay risk and compensation philosophy are “fit for purpose,” which entails executing a statement that verifies a company has performed due diligence on its pay governance processes.
9. The members of a company’s compensation committee should have diverse backgrounds and experience, expertise in risk, finance, and management and should cross-populate the company’s risk and audit committees.
10. To ensure proper compensation risk governance, companies must incorporate collaboration, feedback and review among board committee’s and the firm’s social network to maintain a properly established compensation culture.