House Republicans are demanding the Biden administration starts winding down the COVID-19 public health emergency, while hospital lobbying groups are pressing it to do the opposite.
A group of more than 70 House Republicans wrote Thursday to Department of Health and Human Services (HHS) Secretary Xavier Becerra asking to start the process to wind down the COVID-19 public health emergency (PHE), which was recently extended until April. At the same time, several hospital advocacy groups are hoping the agency keeps the PHE beyond this spring and wants a 60-day notice as to when it will end.
“Although the PHE was certainly necessary at the outset of the pandemic, it was always meant to be temporary,” according to the GOP letter led by Rep. Cathy McMorris Rodgers, R-Washington, ranking member of the House Energy and Commerce Committee.
Republicans want HHS to release a concrete timeline for when the agency plans to exit the PHE.
“We recognize that the PHE cannot end overnight, and that certain actions must be taken to avoid significant disruption to patients and healthcare providers, including working with Congress to extend certain policies like maintaining access to telehealth services for our nation’s seniors,” the letter added.
The PHE granted major flexibilities for providers to get reimbursed by Medicare for telehealth, but those powers will go away after the PHE. It also gave flexibility on several reporting requirements and eased other regulatory burdens.
Another major issue is that states are going to be able to start eligibility redeterminations for Medicaid, which have been paused since the PHE went into effect in January 2020. State Medicaid directors are seeking a heads-up on when the emergency will go away, as states can start to disenroll ineligible beneficiaries after the PHE expires.
Republicans also want Becerra to cite any programs that should be made permanent, and they want “swift action” to lift all COVID-19 vaccine mandates.
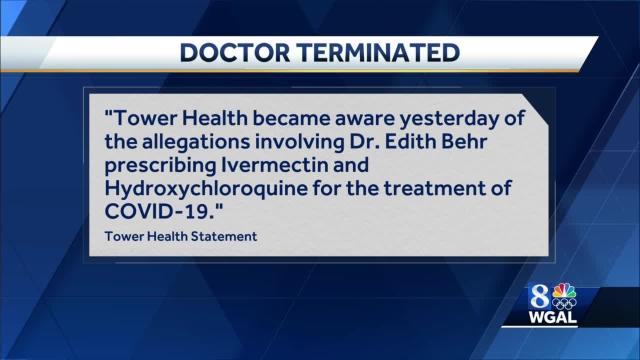
The Supreme Court upheld the Biden administration’s healthcare worker vaccine mandate, overturning a lower court’s stay that affected half of the country. The Centers for Medicare & Medicaid Services has deadlines for states to comply with the vaccination mandate, and facilities that don’t fully comply could risk losing participation in Medicare and Medicaid.
The Republicans charge that the mandates have not “stopped the spread of COVID-19 but have alienated many Americans and have caused staff shortages at hospitals and other healthcare facilities.”
Key drivers of the staff shortages, however, have been a massive surge of the virus overwhelming facilities caused by the omicron variant along with increased expenses facilities have faced for temporary nursing staff. Those lingering expenses are the reason hospital groups are pressing for HHS to do the opposite and extend the PHE beyond April.
The Federation of American Hospitals (FAH) also wrote to Becerra Thursday (PDF) seeking to continue to extend the PHE “well beyond its current expiration date in April 2022.” Even though the omicron surge appears to be easing, the virus is still creating major operational challenges for providers, FAH said.
It also wants the administration to give hospitals a 60-day heads-up when it plans to end the PHE.
“Unwinding the complex web of PHE waiver-authorized operations, programs and procedures—which will have been in place and relied on for more than two years—is a major undertaking that, if rushed, risks destabilizing fragile healthcare networks that patients rely on for care,” the letter said.
The American Hospital Association also wrote to congressional leaders Tuesday seeking for more relief from Congress to help systems overcome staffing shortages that have exacerbated due to the omicron surge.
“The financial pressures hospitals and health systems faced at the beginning of the public health emergency continue, with, for example, ongoing delays in non-emergent procedures, in addition to increased expenses for supplies, medicine, testing and protective equipment,” the letter said.
FAH President Chip Kahn told Fierce Healthcare on Friday that the issues Republicans address in the letter are different from the priorities of the FAH, namely that the association doesn’t focus on mask or vaccine mandates.
“What we are saying is that the PHE has many aspects to it, and so … we think [it] should be extended, but if you don’t then we need to have a lengthy or carefully thought through transition,” Kahn said.
He added that Becerra’s predecessor, acting Secretary Eric Hargan, told providers that they would get a 60-day notice before the end of the PHE. That deadline for such a 60-day notice is Feb. 15.
Kahn said he understands the administration may be under political pressure to end the emergency, but prior notice is absolutely needed.
“I don’t know how they will respond but if they do choose to pull out, we just want to make sure that it doesn’t leave anything behind,” he said.