Category Archives: Leadership Vision
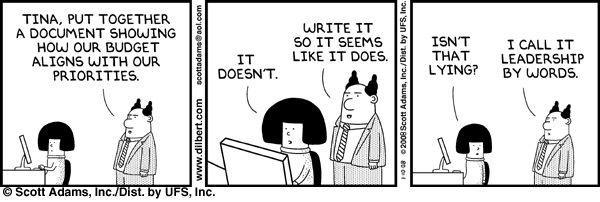
Cartoon – Leadership By Words
In Healthcare, Near-Sightedness is “Normalcy”
Like everyone else, I am thankful the election end is in sight and a degree of “normalcy” might return. By next week, we should know who will sit in the White House, the 119th Congress and 11 new occupants of Governors’ offices. But a return to pre-election normalcy in politics is a mixed blessing.
“Normalcy” in our political system means willful acceptance that our society is hopelessly divided by income, education, ethnic and political views. It’s benign acceptance of a 2-party system, 3-branches of government (Executive, Legislative, Judicial) and federalism that imposes limits on federal power vis a vis the Constitution.
Our political system’ normalcy counts success by tribal warfare and election wins. Normalcy is about issues de jour prioritized by each tribe, not longer-term concern for the greater good in our country. Normalcy in our political system is near-sightedness—winning the next election and controlling public funds.
Comparatively, “normalcy” in U.S. healthcare is also tribal:
while the majority of U.S. adults believe the status quo is not working well but recognize its importance, each tribe has a different take on its future. The majority of the public think price transparency, limits on consolidation, attention to affordability and equitable access are needed but the major tribes—hospitals, insurers, drug companies, insurers, device-makers—disagree on how changes should be made. And each is focused on short-term issues of interest to their members with rare attention to longer-term issues impacting all.
Near-sightedness in healthcare is manifest in how executives are compensated, how partnerships are formed and how Boards are composed.
Organizational success is defined by 1-access to private capital (debt, private equity, strategic investors), 2-sustainnable revenue-growth, 4- scalable costs, 4-opportunities for consolidation (the exit strategy of choice for most) and 5-quarterly earnings. A long-term view of the system’s future is rarely deliberated by boards save attention to AI or the emergence of Big Tech. A vision for an organization’s future based on long-term macro-trends and outside-in methodologies is rare: long-term preparedness is “appreciated” but near-term performance is where attention is vested.
It pays to be near-sighted in healthcare: our complex regulatory processes keep unwelcome change at bay and our archaic workforce rules assure change resistance. …until it doesn’t. Industries like higher education, banking and retailing have experienced transformational changes that take advantage of new technologies and consumer appetite for alternatives that are new and better. The organizations winning in this environment balance near-sightedness with market attentiveness and vision.
Looking ahead, I have no idea who the winners and losers will be in this election cycle. I know, for sure, that…
- The final result will not be known tomorrow and losers will challenge the results.
- Short-term threats to the healthcare status quo will be settled quickly. First up: Congress will set aside Medicare pay cuts to physicians (2.8%) scheduled to take effect in January for the 5th consecutive year. And “temporary” solutions to extend marketplace insurance subsidies, facilitate state supervision of medication abortion services and telehealth access will follow quickly.
- Think tanks will be busy producing white papers on policy changes supported by their funding sponsors.
- And trade associations will produce their playbooks prioritizing legislative priorities and relationship opportunities with state and federal officials for their lobbyists.
Near-term issues for each tribe will get attention: the same is true in healthcare. Discussion about and preparation for healthcare’s longer-term future is a rarity in most healthcare C suites and Boardrooms. Consider these possibilities:
- Medicare Advantage will be the primary payer for senior health: federal regulators will tighten coverage, network adequacy, premiums and cost sharing with enrollees to private insurers reducing enrollee choices and insurer profits.
- To address social determinants of health, equitable access and comprehensive population health needs, regional primary care, preventive and public health programs will be fully integrated.
- Large, organized groups/networks of physicians will be the preferred “hubs” for health services in most markets.
- Interoperability will be fully implemented.
- Physicians will unionize to assert their clinical autonomy and advance their economic interests.
- The federal government (and some states) will limit tax exemptions for profitable not-for-profit health systems.
- The prescription drug patent system will be modernized to expedite time-to-market innovations and price-value determinations.
- The health insurance market will focus on individual (not group) coverage.
- Congress/states will impose price controls on prescription drugs and hospital services.
- Employers will significantly alter their employee benefits programs to reduce their costs and shift accountability to their employees. Many will exit altogether.
- Regional integrated health systems that provide retail, hospital, physician, public health and health insurance services will be the dominant source of services.
- Alternative-payment models used by Medicare to contract with providers will be completely overhauled.
- Consumers will own and control their own medical records.
- Consolidation premised on community benefits, consumer choices and lower costs will be challenged aggressively and reparation pursued in court actions.
- Voters will pass Medicare for All legislation.
And many others.
A process for defining of the future of the U.S. health system and a bipartisan commitment by hospitals, physicians, drug companies, insurers and employers to its implementation are needed–that’s the point.
Near-sightedness in our political system and in our health, system is harmful to the greater good of our society and to the voters, citizens, patients, and beneficiaries all pledge to serve.
As respected healthcare marketer David Jarrard wrote in his blog post yesterday “As the aggravated disunity of this political season rises and falls, healthcare can be a unique convener that embraces people across the political divides, real or imagined. Invite good-minded people to the common ground of healthcare to work together for the common good that healthcare must be.”
Thinking and planning for healthcare’s long-term future is not a luxury: it’s an urgent necessity. It’s also not “normal” in our political and healthcare systems.
The Four Questions Healthcare Boards must Answer
In 63 days, Americans will know the composition of the 119th Congress and the new occupants of the White House and 11 Governor’s mansions. We’ll learn results of referenda in 10 states about abortion rights (AZ, CO, FL, MD, MO, MT, NE, NV, NY, SD) and see how insurance coverage for infertility (IVF therapy) fares as Californians vote on SB 729. But what we will not learn is the future of the U.S. health system at a critical time of uncertainty.
In 6 years, every baby boomer will be 65 years of age or older. In the next 20 years, the senior population will be 22% of the population–up from 18% today. That’s over 83 million who’ll hit the health system vis a vis Medicare while it is still digesting the tsunami of obesity, a scarcity of workers and unprecedented discontent:
- The majority of voters is dissatisfied with the status quo. 69% think the system is fundamentally flawed and in need of major change vs. 7% who think otherwise. 60% believe it puts its profits above patient care vs. 13% who disagree.
- Employers are fed up: Facing projected cost increases of 9% for employee coverage in 2025, they now reject industry claims of austerity when earnings reports and executive compensation indicate otherwise. They’re poised to push back harder than ever.
- Congress is increasingly antagonistic: A bipartisan coalition in Congress is pushing populist reforms unwelcome by many industry insiders i.e. price transparency for hospitals, price controls for prescription drugs, limits on private equity ownership, constraint on hospital, insurer and physician consolidation, restrictions on tax exemptions of NFP hospitals, site neutral payment policies and many more.
Fanning these flames, media characterizations of targeted healthcare companies as price gouging villains led by highly-paid CEOs is mounting: last week, it was Acadia Health’s turn courtesy of the New York Times’ investigators.
Navigating uncertainty is tough for industries like healthcare where demand s growing, technologies are disrupting how and where services are provided and by whom, and pricing and affordability are hot button issues. And it’s too big to hide: at $5.049 trillion, it represents 17.6% of the U.S. GDP today increasing to 19.7% by 2032. Growing concern about national debt puts healthcare in the crosshairs of policymaker attention:
Per the Committee for a Responsible Federal Budget: “In the latest Congressional Budget Office (CBO) baseline, nominal spending is projected to grow from $6.8 trillion in Fiscal Year (FY) 2024 to $10.3 trillion in 2034. About 87% of this increase is due to three parts of the federal budget: Social Security, federal health care programs, and interest payments on the debt.”
In response, Boards in many healthcare organizations are hearing about the imperative for “transformational change” to embrace artificial intelligence, whole person health, digitization and more. They’re also learning about ways to cut their operating costs and squeeze out operating margins. Bold, long-term strategy is talked about, but most default to less risky, short-term strategies compatible with current operating plans and their leaders’ compensation packages. Thus, “transformational change” takes a back seat to survival or pragmatism for most.
For Boards of U.S. healthcare organizations, the imperative for transformational change is urgent: the future of the U.S. system is not a repeat of its past. But most Boards fail to analyze the future and construct future-state scenarios systematically. Lessons from other industries are instructive.
- Transformational change in mission critical industries occurs over a span of 20-25 years. It starts with discontent with the status quo, then technologies and data that affirm plausible alternatives and private capital that fund scalable alternatives. It’s not overnight.
- Transformational change is not paralyzed by regulatory hurdles. Transformers seek forgiveness, not permission while working to change the regulatory landscape. Advocacy is a critical function in transformer organizations.
- Transformation is welcomed by consumers. Recognition of improved value by end-users—individual consumers—is what institutionalizes transformational success. Transformed industries define success in terms of the specific, transparent and understandable results of their work.
Per McKinsey, only one in 8 organizations is successful in fully implementing transformational change completely but the reward is significant: transformers outperform their competition three-to-one on measures of growth and effectiveness.
I am heading to Colorado Springs this weekend for the Governance Institute. There, I will offer Board leaders four basic questions.
- Is the future of the U.S. health system a repeat of the past or something else?
- How will its structure, roles and responsibilities change?
- How will affordability, quality, innovation and value be defined and validated?
- How will it be funded?
Answers to these require thoughtful discussion. They require independent judgement. They require insight from organizations outside healthcare whose experiences are instructive. They require fresh thinking.
Until and unless healthcare leaders recognize the imperative for transformational change, the system will calcify its victim-mindset and each sector will fend for itself with diminishing results. No sector—hospitals, insurers, drug companies, physicians—has all the answers and every sector faces enormous headwinds. Perhaps it’s time for a cross-sector coalition to step up with transformational change as the goal and the public’s well-being the moral compass.
PS: Last week, I caught up with Drs. Steve and Pat Gabbe in Columbus, Ohio. Having served alongside them at Vanderbilt and now as an observer of their work at Ohio State, I am reminded of the goodness and integrity of those in healthcare who devote their lives to meaningful, worthwhile work. Steve “burns with a clear blue flame” as a clinician, mentor and educator. Pat is the curator of a program, Moms2B, that seeks to alleviate Black-White disparities in infant mortality and maternal child health in Ohio. They’re great people who see purpose in their calling; they’re what make this industry worth fixing!
Thought of the Day – What You Leave Behind
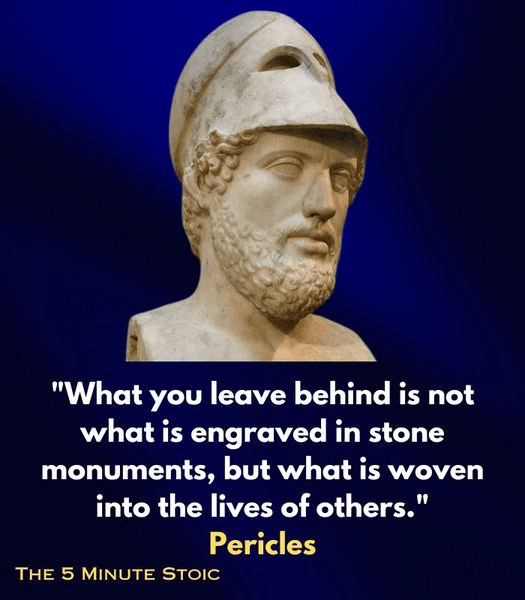
Pericles is perhaps best remembered for a building program centered on the Acropolis which included the Parthenon and for a funeral oration he gave early in the Peloponnesian War, as recorded by Thucydides. In the speech he honored the fallen and held up Athenian democracy as an example to the rest of Greece.
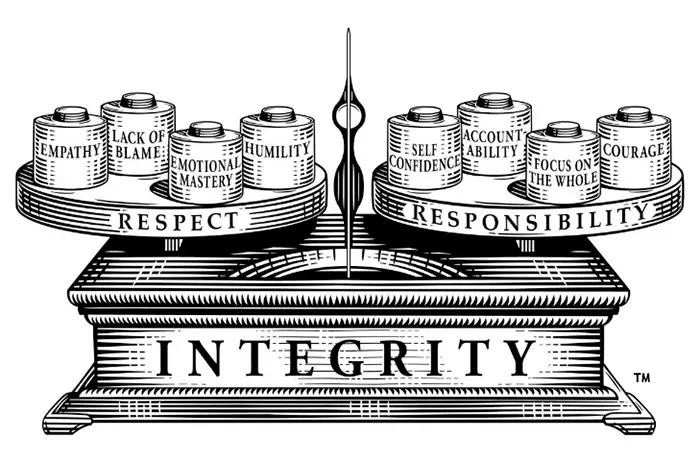
Leadership Integrity
Quote of the Day – On Actions, Habits and Character
Steward Files for Bankruptcy and It Feels All Too Familiar
https://www.kaufmanhall.com/insights/blog/steward-files-bankruptcy-and-it-feels-all-too-familiar

Steward Health Care’s Chapter 11 bankruptcy filing on May 6, 2024, brought back bad memories of another large health system bankruptcy.
On July 21, 1998, Pittsburgh-based Allegheny Health and Education Research Foundation (AHERF) filed Chapter 11. AHERF grew very rapidly, acquiring hospitals, physicians, and medical schools in its vigorous pursuit of scale across Pennsylvania. Utilizing debt capacity and spending cash, AHERF quickly ran out of both, defaulted on its obligations, and then filed for bankruptcy. It was one of the largest bankruptcy filings in municipal finance and the largest in the rated not-for-profit hospital universe.
Steward Health Care is a for-profit, physician-owned hospital company, but its long-standing roots were in faith-based not-for-profit healthcare. Prior to the acquisition by Cerberus Capital Management in 2010, Caritas Christi Health Care System was comprised of six hospitals in eastern Massachusetts. Caritas was a well-regarded health system, providing a community alternative to the academic medical centers in downtown Boston. Over the next 14 years, Steward grew rapidly to 31 hospitals in eight states, most recently bolstered through an expansive sale-leaseback structure with a REIT. Per the bankruptcy filings, the company reported $9 billion in secured debt and leases on $6 billion of revenue.
Chapter 11 bankruptcy filings in corporate America are a means to efficiently sell assets or a path to re-emergence as a new streamlined company. A quick glance at Steward’s organizational structure shows a dizzying checkerboard of companies and LLCs that will require a massive untangling. Further, its capital structure includes both secured debt for operations and a separate and distinct lease structure for its facilities, and in bankruptcy, that signals significant complexity. Bankruptcy filings in not-for-profit healthcare are less common, although it is surprising that the industry did not see an increase after the pandemic. Not-for-profit hospitals that are in distress seem to hang on long enough to find a buyer, gain increased state funding, attain accommodations on obligations, or find some other escape route to avoid a payment default or filing.
Details regarding Steward’s undoing will unfold in the coming weeks as it moves through an auction process. But there are some early takeaways the not-for-profit industry can learn from this:
- Remain essential in your local market. Hospitals must prove their value to their constituents, including managed care payers, especially in competitive urban markets, as Steward may have learned in eastern Massachusetts and Miami. Prior strategies of making a margin as an out-of-network provider are no longer viable as patients must shoulder more of the financial burden. Simply put, your organization should be asking one question: does a managed care plan need our existing network to sell a product in our market? If the answer is no, you need to develop strategies that make your hospital essential.
- Embrace financial planning for long-term viability. Without it, a hospital or health system will be unable to afford the capital spending it needs to maintain attractive, patient-friendly, state-of-the art facilities or absorb long-term debt to fund the capital. Annual financial planning is more than just a trendline going forward. The scenarios and inputs must be well-founded, well-grounded in detail, and based on conservative assumptions. Increasing attention has to be paid to disrupters, innovators, specialized/segmented offerings, and expansion plans of existing and new competitors. Investors expect this from not-for-profit borrowers. Higher-performing hospitals and health systems of all sizes do this well.
- Build capital capacity through improved cash flow. It is undoubtedly clear that Steward, like AHERF, was unable to afford the capital and debt they thought they could, either through flawed financial planning of its future state or, more concerning, the complete absence of it. Or they believed that rapid growth would solve all problems, not detailed financial planning, the use of benchmarks, or a sharp focus on operations. Increasing that capacity through sustained financial performance will allow an organization to de-leverage and build capital capacity.
When the case studies are written about Steward, a fact pattern will be revealed that includes the inability or unwillingness to attain synergies as a system, underspending on facility capital needs given a severe liquidity crunch, labor challenges, and a rapid payer mix shift.
Underlying all of this will undoubtedly be a failure of governance and leadership as we saw with AHERF. It will also likely indicate that one of the most precious assets healthcare providers may have is the management bandwidth to ensure strategic plans are appropriately made, tested, monitored, and executed.
While Steward and AHERF may be held up as extreme cases, not-for-profit hospital governance must continue to focus on checks-and-balances of management resources. Likewise, management must utilize benchmarks, data, and strong financial planning, given the challenges the industry faces.
Hospitals at a Crossroad: Reactive Navigation or Proactive Orchestration?

This is National Hospital week. It comes at a critical time for hospitals:
The U.S. economy is strong but growing numbers in the population face financial insecurity and economic despair. Increased out-of-pocket costs for food, fuel and housing (especially rent) have squeezed household budgets and contributed to increased medical debt—a problem in 41% of U.S. households today. Hospital bills are a factor.
The capital market for hospitals is tightening: interest rates for debt are increasing, private investments in healthcare services have slowed and valuations for key sectors—hospitals, home care, physician practices, et al—have dropped. It’s a buyer’s market for investors who hold record assets under management (AUM) but concerns about the harsh regulatory and competitive environment facing hospitals persist. Betting capital on hospitals is a tough call when other sectors appear less risky.
Utilization levels for hospital services have recovered from pandemic disruption and operating margins are above breakeven for more than half but medical inflation, insurer reimbursement, wage increases and Medicare payment cuts guarantee operating deficits for all. Complicating matters, regulators are keen to limit consolidation and force not-for-profits to justify their tax exemptions. Not a pretty picture.
And, despite all this, the public’s view of hospitals remains positive though tarnished by headlines like these about Steward Health’s bankruptcy filing last Monday:
- Who is Ralph de la Torre? The CEO of Steward Health Care with a $40 million yacht (msn.com)
- The Private-Equity Deal That Flattened a Hospital Chain and Its Landlord – WSJ
- One of the Biggest Hospital Failures in Decades Raises Concerns for Patient Care – WSJ
- Steward Health Care files for Chapter 11 bankruptcy | Healthcare Dive
- Steward plans sale of all hospitals, reports $9B in debt (beckershospitalreview.com)
- What Steward Health Care’s bankruptcy means for patient care | Modern Healthcare
- As Steward Ship Was Sinking, CEO Bought $40M Yacht | MedPage Today
- Steward files for bankruptcy: What physicians need to know (beckersphysicianleadership.com)
- Why is Healey saying everything at Steward hospitals will be OK? (bostonglobe.com)
- Bankrupt Steward Health puts its hospitals up for sale, discloses $9 bln in debt | Reuters
- Steward Health Care bankruptcies: Can they get that process right? (bostonglobe.com)
The public is inclined to hold hospitals in high regard, at least for the time being. When asked how much trust and confidence they have in key institutions to “to develop a plan for the U.S. health system that maximizes what it has done well and corrects its major flaws,” consumers prefer for solutions physicians and hospitals over others but over half still have reservations:
| A Great Deal | Some | Not Much/None | |
| Health Insurers | 18% | 43% | 39% |
| Hospitals | 27% | 52% | 21% |
| Physicians | 32% | 53% | 15% |
| Federal Government | 14% | 42% | 44% |
| Retail Health Org’s | 21% | 51% | 28% |
The American Hospital Association (AHA) is rightfully concerned that hospitals get fair treatment from regulators, adequate reimbursement from Medicare and Medicaid and protection against competitors that cherry-pick profits from the health system.
It can rightfully assert that declining operating margins in hospitals are symptoms of larger problems in the health system: flawed incentives, inadequate funding for preventive and primary care, the growing intensity of chronic diseases, medical inflation for wages, drugs, supplies and technologies, the dominance of ‘Big Insurance’ whose revenues have grown 12.1% annually since the pandemic and more. And it can correctly prove that annual hospital spending has slowed since the pandemic from 6.2% (2019) to 2.2% (2022) in stark contrast to prescription drugs (up from 4% to 8.4% and insurance costs (from -5.4% to +8.5%). Nonetheless, hospital costs, prices and spending are concerns to economists, regulators and elected officials.
National health spending data illustrate the conundrum for hospitals: relative to the overall CPI, healthcare prices and spending—especially outpatient hospital services– are increasing faster than prices and spending in other sectors and it’s getting attention: that’s problematic for hospitals at a time when 5 committees in Congress and 3 Cabinet level departments have their sights set on regulatory changes that are unwelcome to most hospitals.
My take:
The U.S. market for healthcare spending is growing—exceeding 5% per year through the next decade. With annual inflation targeted to 2.0% by the Fed and the GDP expected to grow 3.5-4.0% annually in the same period, something’s gotta’ give. Hospitals represent 30.4% of overall spending today (virtually unchanged for the past 5 years) and above 50% of total spending when their employed physicians and outside activities are included, so it’s obvious they’ll draw attention.
Today, however, most are consumed by near-term concerns– reimbursement issues with insurers, workforce adequacy and discontent, government mandates– and few have the luxury to look 10-20 years ahead.
I believe hospitals should play a vital role in orchestrating the health system’s future and the role they’ll play in it. Some will be specialty hubs. Some will operate without beds. Some will be regional. Some will close. And all will face increased demands from regulators, community leaders and consumers for affordable, convenient and effective whole-person care.
For most hospitals, a decision to invest and behave as if the future is a repeat of the past is a calculated risk. Others with less stake in community health and wellbeing and greater access to capital will seize this opportunity and, in the process, disable hospitals might play in the process.
Near-term reactive navigation vs. long-term proactive orchestration–that’s the crossroad in front of hospitals today. Hopefully, during National Hospital Week, it will get the attention it needs in every hospital board room and C suite.
PS: Last week, I wrote about the inclination of the 18 million college kids to protest against the healthcare status quo (“Is the Health System the Next Target for Campus Unrest?” The Keckley Report May 6, 2024 www.paulkeckley.com). This new survey caught my attention:
According to the Generation Lab’s survey of 1250 college students released last week, healthcare reform is a concern. When asked to choose 3 “issues most important to you” from its list of 13 issues, healthcare reform topped the list. The top 5:
- Health Reform (40%)
- Education Funding and access (38%)
- Economic fairness and opportunity (37%)
- Social justice and civil rights (36%)
- Climate change (35%)
If college kids today are tomorrow’s healthcare workforce and influencers to their peers, addressing the future of health system with their input seems shortsighted. Most hospital boards are comprised of older adults—community leaders, physicians, et al.
And most of the mechanisms hospitals use to assess their long-term sustainability is tethered to assumptions about an aging population and Medicare.
College kids today are sending powerful messages about the society in which they aspire to be a part. They’re tech savvy, independent politically and increasingly spiritual but not religious. And the health system is on their radar.