On the morning of November 7, major news networks starting with CNN called the presidential election for Joe Biden. Although the election has yet to be officially certified, Biden and Vice President-elect Kamala Harris have wasted no time preparing their response to the rapidly worsening coronavirus pandemic.
Over the past week, the US has averaged more than 150,000 new COVID-19 cases per day, an increase of 81% from the average on November 1. The US had a record 181,200 new reported cases on November 13. Over 11 million Americans have been infected, and the nation is nearing a grim milestone of 250,000 deaths. Experts warn that the worst is yet to come. As temperatures drop and family-centric holidays approach, people are likely to spend more time socializing indoors with non-household members, increasing the risk for COVID-19 transmission.
Mitigating the spread of the coronavirus and preventing more deaths are top priorities for the incoming Biden-Harris administration. Biden’s campaign team published a seven-point plan to beat COVID-19, and on November 9, the Biden-Harris transition team named a COVID-19 Advisory Council tasked with guiding the federal response to the pandemic immediately after the inauguration.
The council “will be consulting with state and local officials to gauge public-health steps needed to bring the virus under control,” Evan Halper and Noam Levey reported in the Los Angeles Times. “The board will also focus on racial and ethnic disparities in how, where, and how quickly the virus is spreading.”
Innovative Plan: Tell the Truth
The Biden-Harris plan sets a new tone for the nation’s coronavirus response, using federal powers and leadership to centralize the acquisition and distribution of personal protective equipment (PPE), along with the coordination of testing and contact tracing, instead of leaving those vital resources to be led in 50 different ways by state governors. It emphasizes evidence-based guidance and empowers public health officials and scientists to guide and revise the nation’s reopening strategy as the pandemic evolves.
“You’ll immediately see a change of tone, a change in communication,” Ezekiel Emanuel, MD, PhD, the vice provost for global initiatives at the University of Pennsylvania, told Politico. “This is the stuff of real leadership: telling the truth, modeling the right behaviors like wearing a mask, only having small crowds, putting the scientists out there.”
The first priority in the plan is to ensure that all Americans have access to regular, reliable, and free coronavirus testing. Rapid testing is vital for identifying, isolating, and treating new cases of COVID-19, but the US has been crippled by continuing test shortages and long lag times before results are reported. Biden plans to double the number of drive-through testing sites while scaling up next-generation solutions like home tests.
Contact tracing goes hand-in-hand with testing in the public health response to COVID-19, and the plan would establish a US Public Health Job Corps to train and mobilize 100,000 Americans to perform culturally competent contact tracing in communities most affected by COVID-19.
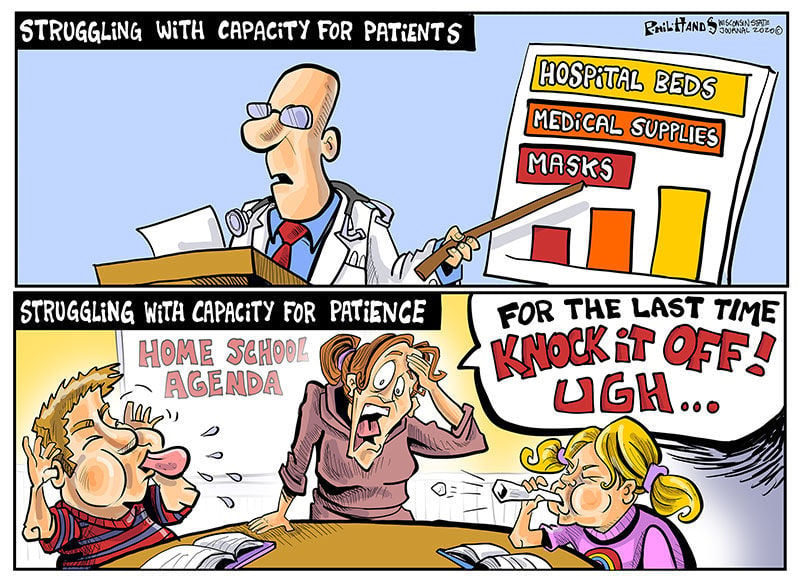
The second priority is to fix the nation’s PPE problems. N95 masks, gloves, gowns, and other PPE used by health care staff are still in short supply. AARP reported that one in four nursing homes ran short of PPE between August 24 and September 20. (Nursing homes continue to be a hot spot for coronavirus transmission.) Biden would use the Defense Production Act to increase production of PPE and distribute the supply to states instead of leaving states to fend for themselves.
For the third priority, Biden would tap the nation’s wealth of science experts to provide clear public guidance on how communities should navigate the pandemic. The US Centers for Disease Control and Prevention (CDC) would lead this effort, with an emphasis on helping communities determine when it is safe to reopen schools and various types of businesses.
Navigating Hurdles to Safe, Effective, Accepted Vaccine
Although the pharmaceutical company Pfizer announced on November 9 that its coronavirus vaccine trial showed positive early results, the road to vaccinating all Americans is tortuous. Pfizer still needs to seek emergency use authorization from the Food and Drug Administration (FDA) and ramp up vaccine production to meet the global need. In the meantime, Biden plans to invest $25 billion in a vaccine manufacturing and distribution plan that ensures every American can get vaccinated for free. This fourth priority would make the vaccine accessible to all people and communities regardless of income or any other factor.
The fifth priority is to protect Americans who are at high risk of getting seriously ill or dying from COVID-19. This includes people over 65, nursing home residents, and people living in neighborhoods with higher rates of COVID-19. Biden would establish a COVID-19 Racial and Ethnic Disparities Task Force (PDF) to report on disparities in COVID-19 infection, hospitalization, and death rates, as well as to provide recommendations to Congress and the Federal Emergency Management Agency on how best to distribute resources and relief funds to combat these disparities. The plan also calls for strengthening the Affordable Care Act to ensure that during the pandemic, Americans have health insurance coverage.
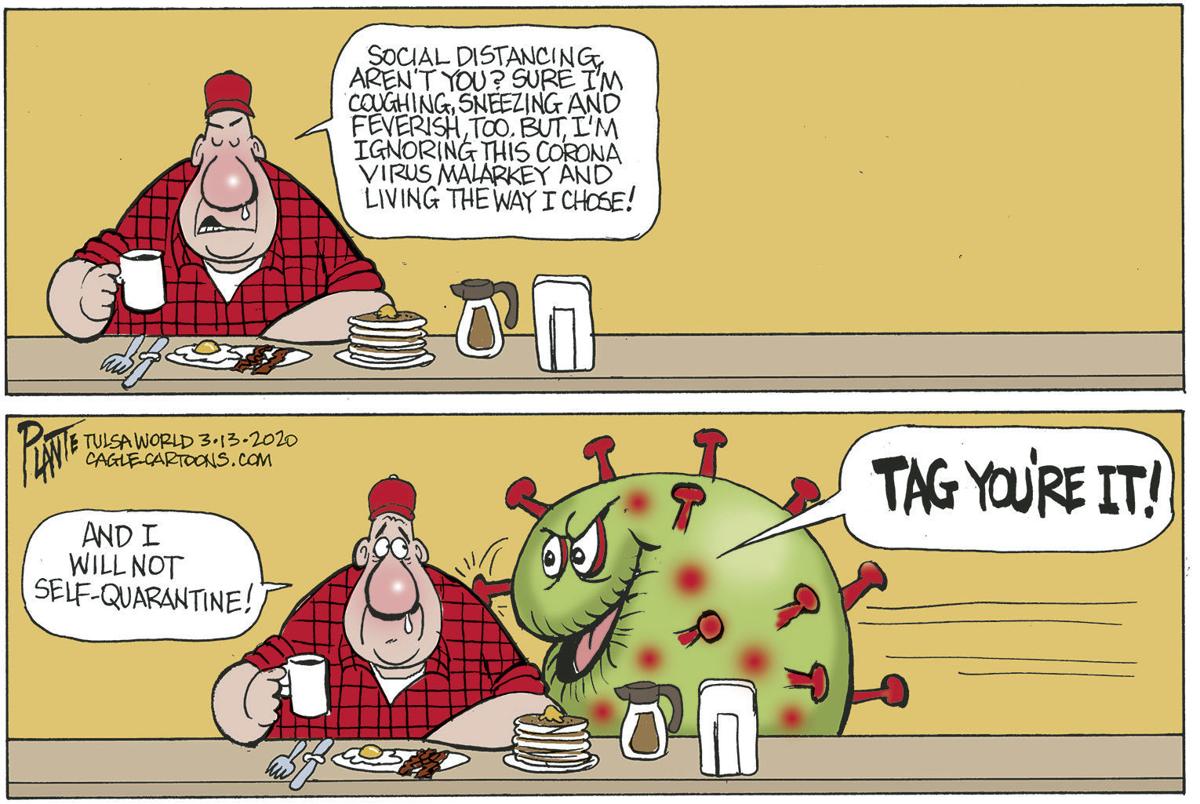
During the presidential campaign, Biden called for a national mask mandate based on the growing body of evidence that mask-wearing can considerably reduce the transmission of respiratory viruses like the one that causes COVID-19. Biden plans to coordinate with governors and mayors to convince Americans to wear a mask when they are around people outside their household. Currently, 34 states and the District of Columbia mandate face masks in public, but there is no nationwide requirement.
Finally, the plan takes the long view on pandemic threats by rebuilding and reinvesting in defenses that will help the world predict and prevent future pandemics. The Biden administration has declared that the US will rejoin the World Health Organization, restore the White House National Security Council Directorate for Global Health Security and Biodefense, which was eliminated by the Trump administration in 2018, and shore up CDC’s global corps of disease detectives.
Public Health Experts at the Helm
The newly announced COVID-19 Advisory Council is a who’s who of public health experts, former government officials, and doctors, including several from California. The panel currently comprises 13 members, but Biden has said it may be expanded.
The three cochairs of the advisory board are former surgeon general Vivek Murthy, MD; former FDA commissioner David Kessler, MD, a UCSF professor of pediatrics, and of epidemiology and biostatistics; and Marcella Nunez-Smith, MD, MPH, an associate professor of internal medicine, public health, and management at Yale University whose research focuses on health disparities.
The other members appointed so far include:
- Luciana Borio, MD, vice president at the venture capital firm In-Q-It. Borio served in multiple leadership roles in the Trump and Obama administrations in the National Security Council and FDA.
- Rick Bright, PhD, director of the Biomedical Advanced Research and Development Authority under Trump and Obama. Bright resigned from the government in October after being removed from his vaccine development role by President Trump.
- Ezekiel Emanuel, MD, PhD, the vice provost for global initiatives at the University of Pennsylvania. Emanuel served in the Obama administration as special advisor for health policy to Peter Orszag, PhD, the former director of the Office of Management and Budget.
- Atul Gawande, MD, MPH, a professor at Harvard Medical School and the Harvard T.H. Chan School of Public Health. Gawande is a staff writer covering health and medicine at the New Yorker and served in the Clinton administration as senior adviser in the Department of Health and Human Services.
- Eric Goosby, MD, a professor of medicine at UCSF. Goosby, an expert on HIV/AIDS, led policy work in this field under Clinton and Obama.
- Celine Gounder, MD, a clinical assistant professor of internal medicine and infectious diseases at New York University.
- Julie Morita, MD, executive vice president of the Robert Wood Johnson Foundation and former commissioner of the Chicago Department of Public Health.
- Michael Osterholm, PhD, MPH, director of the Center for Infectious Disease Research and Policy at the University of Minnesota.
- Loyce Pace, MPH, president and executive director of the Global Health Council.
- Robert Rodriguez, MD, a professor of emergency medicine at UCSF.


/cloudfront-us-east-1.images.arcpublishing.com/sltrib/N2O6A445TNBPTN7OGAFQO4ONLY.jpg)