https://www.healthleadersmedia.com/dinged-dented-defiant-aca-still-standing

Texas v. Azar is the latest in a long line of lawsuits and legislation that Republicans have used to undermine the Affordable Care Act, which has shown itself to be remarkably resilient.
KEY TAKEAWAYS
A federal judge in Texas could slap a preliminary injunction on the ACA.
The case is the latest in a long string of efforts to dismantle the ACA since its inception in 2010.
A federal judge in Texas is poised to drop a ruling that could determine the future of the Affordable Care Act.
Or, maybe not.
The Republican plaintiffs from 20 states in Texas v. Azar argued before U.S. District Judge Reed O’Connor in early September that the entire ACA became unconstitutional when Congress zeroed out the individual mandate penalty, effective 2019.
Led by Texas Attorney General Ken Paxton, the Republican plaintiffs are asking for a preliminary injunction. The Department of Justice, which declined to defend portions of the ACA, also urged O’Conner to delay any injunction until after the enrollment period, saying any attempts to impose the injunction during the enrollment period would invite “chaos.”
If the injunction goes through, it could end premium subsidies for ACA beneficiaries and cripple enrollment. The Urban Institute has estimated that 17 million people would lose their health insurance coverage if the ACA was overturned.
As potentially catastrophic as this sounds, the healthcare sector doesn’t seem to be overly concerned. In fact, business couldn’t be better.
A report in Axios shows that many players in the healthcare sector are prospering under the ACA. The website notes that S&P 500 healthcare index of 63 major companies has grown by 186% since the ACA became law in 2010, outstripping the S&P 500 and the Dow Jones.
In addition, health insurance companies are flush. Shares of UnitedHealth Group have gone up more than 700% since 2010, and the stock price of ACA marketplace insurer Centene has gone up 1,100% over the same period, Axios reports.
While hospitals have had a tougher time of it, especially in states that refused to expand Medicaid, they’re still seeing reductions in charity care and bad debt owing.
Regardless of how O’Connor rules in Texas v. Azar, ACA payers, providers, and other stakeholders will continue to presume that the law isn’t going anywhere, says healthcare economist Gail Wilensky.
“They’re assuming it’ll be around, or something very similar will be,” says Wilensky, a former director of Medicare and Medicaid, and a former chair of the Medicare Payment Advisory Commission.
“I don’t think people are regarding any serious likelihood of it going away again,” she says.
Even if O’Connor, appointed to the court in 2007 by President George W. Bush, agrees with the severability arguments raised by the Republican governors and attorneys general in 20 states who brought the suit, the matter likely would get shot down on appeal, Wilensky says.
” I would be surprised if it doesn’t get reversed someplace else,” says Wilensky, now a senior fellow at Project HOPE.
“If it had go all the way to the Supreme Court, the Supreme Court isn’t going to tolerate it, but I don’t know that it would even get that far,” she says.
The case is just one in a long string of legal and legislative actions Republicans are taking at the state and federal level to either undermine or bolster the ACA.
Earlier this year, O’Connor sided with Texas and five other states and threw out an Obama administration tax on states receiving Medicaid funds.
The Republican-controlled Congress has tried more than 50 times to repeal Obamacare, and Senate Majority Leader Mitch McConnell said this week that Republicans may try again in 2019.
While the signature legislation of the Obama era has been dinged and dented, it’s also proven to be remarkably resilient.
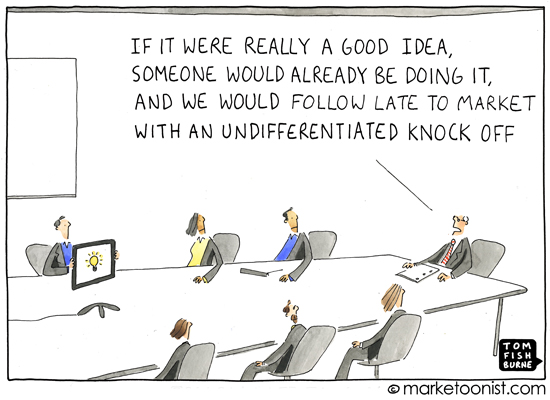
Wilensky says the ACA is resilient because it solves a problem “for a small but non-trivial group of people,” and that Republicans don’t have a credible alternative.
“Once a benefit is in place for any measurable amount of time, certainly two or three years would qualify, there’s no precedent for removing it,” she says.
“And most of the proposals that had come up did not seriously get the job done,” Wilensky says.
“They really weren’t effective as an alternative and you simply aren’t going to take away a benefit, like the extension of insurance to people who are above the poverty line and not offered traditionally employer sponsored insurance without having a credible alternative.”
“It’s just not going to happen because there are too many issues that have already been adjudicated at a more serious level,” Wilensky says. “I don’t know why they did this other than that this is 20 attorneys general and they’re running for something.”