Category Archives: Uncategorized
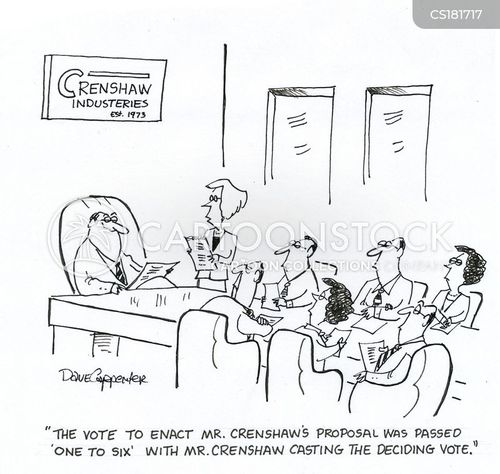
Cartoon – The Deciding Vote
Cartoon – A Stealth Layoff
Cartoon – My Dream
12 latest hospital bankruptcies
https://www.beckershospitalreview.com/finance/12-latest-hospital-bankruptcies-041019.html
From reimbursement landscape challenges to dwindling patient volumes, many factors lead hospitals to file for bankruptcy.
Here are 12 hospitals that filed for bankruptcy since Jan. 1, beginning with the most recent:
1. De Queen (Ark.) Medical Center filed for Chapter 11 bankruptcy on April 3. The hospital, owned by an affiliate of Kansas City, Mo.-based EmpowerHMS, entered bankruptcy after facing financial challenges for months. Electricity was temporarily shut off in some parts of the hospital in February due to nonpayment, and the hospital subsequently stopped providing patient care.
2. Prague (Okla.) Community Hospital, owned by an affiliate of EmpowerHMS, entered Chapter 11 bankruptcy on March 21. A judge allowed a new company to take over management of Prague Community Hospital in early March after the hospital experienced payroll issues and lacked funds for supplies.
3. I-70 Community Hospital in Sweet Springs, Mo., filed for Chapter 11 bankruptcy on March 21. The bankruptcy filing came after CMS ended its provider agreement with the hospital, which voluntarily suspended its license for 90 days on Feb. 15. I-70 Community Hospital is owned by an affiliate of EmpowerHMS.
4. Haskell County Community Hospital in Stigler, Okla., filed for Chapter 11 bankruptcy on March 17. The hospital, owned by an affiliate of EmpowerHMS, entered bankruptcy with less than $50,000 in assets and at least $1 million in liabilities.
5. Drumright (Okla.) Regional Hospital, owned by an affiliate of EmpowerHMS, filed for Chapter 11 bankruptcy on March 17. The hospital entered bankruptcy with less than $50,000 in assets and upward of $10 million in estimated liabilities.
6. Oswego (Kan.) Community Hospital entered Chapter 11 bankruptcy on March 17. The bankruptcy filing came after the hospital, owned by an affiliate of EmpowerHMS, abruptly closed Feb. 14.
7. Fairfax (Okla.) Community Hospital, owned by an affiliate of EmpowerHMS, filed for Chapter 11 bankruptcy March 17. The hospital entered bankruptcy with less than $50,000 in assets and at least $1 million in liabilities.
8. Horton (Kan.) Community Hospital entered Chapter 11 bankruptcy March 14, just two days after it closed. In its bankruptcy petition, the hospital said it has less than $50,000 in assets and liabilities of between $1 million and $10 million. Horton Community Hospital is owned by an affiliate of EmpowerHMS.
9. Hillsboro (Kan.) Community Hospital, owned by an affiliate of EmpowerHMS, filed for Chapter 11 bankruptcy on March 13. According to documents filed in the bankruptcy case, the hospital has at least $10 million in assets and at least $10 million in liabilities. The hospital owes more than $334,000 in real estate taxes, making the Marion County (Kan.) Treasurer the unsecured creditor with the largest claim against the hospital.
10. Lauderdale Community Hospital in Ripley, Tenn., filed for Chapter 11 bankruptcy on March 8. The hospital, owned by an affiliate of EmpowerHMS, has faced financial challenges for months, and a federal judge appointed a receiver to oversee the hospital’s finances in February.
11. Washington County Hospital in Plymouth, N.C., entered bankruptcy in February after creditors filed an involuntary Chapter 7 bankruptcy petition. The hospital, owned by an affiliate of EmpowerHMS, missed payroll Feb. 8 and suspended all medical services Feb. 14.
12. Penobscot Valley Hospital, a 25-bed critical access hospital in Lincoln, Maine, filed for Chapter 11 bankruptcy Jan. 29. “We have made tremendous strides over the last three years in bringing our operational costs in line with revenue,” Hospital CEO Crystal Landry said in a press release. “Legacy debt is the issue here, and Chapter 11 allows us to restructure that debt so we can keep our doors open and ensure that our community continues to have a hospital close to home.”
Private equity-owned hospital chain files for bankruptcy
New LifeCare Hospitals, a long-term acute care hospital operator based in Plano, Texas, filed for Chapter 11 bankruptcy protection May 6, according to The Wall Street Journal.
The company, owned mostly by affiliates of Blue Mountain Capital, Monarch Alternative Capital and Twin Haven Special Opportunities Fund, cited declining reimbursement due to Medicare changes as the reason for the bankruptcy filing.
Prior to entering bankruptcy, New LifeCare, which operates 17 facilities in nine states, closed some hospitals and took other steps to cut costs.
New LifeCare is in discussions with potential buyers, and CEO James Murray expects the company to be auctioned through the bankruptcy process later this year, according to The Wall Street Journal, which cited bankruptcy court documents.
Hedge fund manager predicts CHS will go bankrupt
https://www.beckershospitalreview.com/finance/hedge-fund-manager-predicts-chs-will-go-bankrupt.html
Firefly Value Partners Co-Founder and Portfolio Manager Ryan Heslop is bearish on Franklin, Tenn.-based Community Health Systems, according to Reuters.
Mr. Heslop, who was one of several hedge fund managers to present May 6 at the Ira Sohn Investment Conference in New York, announced a short position in CHS during the conference.
He said CHS will likely go bankrupt over the next few years due to rising debt costs and dwindling revenue per hospital bed.
The company’s “pile of debt and the declining profitability of hospitals make it almost certain that this patient will die,” Mr. Heslop said, according to Reuters.
CHS didn’t immediately respond to Reuters’ request for comment.
During the conference, other discussions about for-profit hospital operators were positive. Glenview Capital Management Founder and CEO Larry Robbins said he’s bullish on hospitals overall, and owning stock in Nashville, Tenn.-based HCA Healthcare, King of Prussia-based Universal Health Services and Dallas-based Tenet Healthcare is a wise decision, according to Barron’s.
Judge Rules 340B Cuts Unlawful, Decision Applauded by Industry Stakeholders

A federal judge reaffirmed his view that the cuts by HHS to the discount drug program are unlawful.
KEY TAKEAWAYS
In a joint statement, three hospital plaintiffs urged HHS to follow the judge’s directive.
340B Health added their approval in a statement, asking the agency to “act quickly.”
A status report regarding HHS’ progress remedying the situation must be submitted to U.S. District Court Judge Rudolph Contreras by August 5.
U.S. District Court Judge Rudolph Contreras again ruled Monday evening that the 340B drug reimbursement rate that Health and Human Services set in the 2019 Outpatient Prospective Payment System (OPPS) rule is unlawful, a decision that earned praise from various industry stakeholders.
Five months after first vacating the 22% cut in 340B payments that HHS Secretary Alex Azar proposed late last year, Contreras reiterated that the cuts were implemented “in contravention of the Medicare Act’s plain text.”
Medicare Part B will sell prescription drugs to hospitals participating in the program at the average selling price plus 6%, well above the average selling price minus 22.5% as HHS had proposed.
“The Court also concludes that, despite the fatal flaw in the agency’s rate adjustments, vacating HHS’ 2018 and 2019 rules is not the best course of action, given the havoc vacatur may wreck on Medicare’s administration,” Contreras wrote in the 22-page ruling.
HHS will have “first crack” at crafting appropriate remedies for the two rules, according to the ruling.
Tuesday, three hospital plaintiffs applauded the ruling as a positive development for the embattled federal program, which has been deemed wasteful and rife with abuse by critics who demand additional oversight and accountability.
“America’s 340B hospitals are pleased with the District Court’s decision and urge HHS to follow the judge’s directive to promptly resolve the harm caused by its unlawful cuts to Medicare reimbursement for certain 340B hospitals,” the American Hospital Association, Association of American Medical Colleges, and America’s Essential Hospitals said in a joint statement. “The ruling reaffirmed that the 2018 cuts were unlawful and extended that ruling to the 2019 cuts. Owing to the complexity of the Medicare program, the judge gave HHS first crack at fashioning a remedy for its unlawful actions. He also asked for a report from HHS on its progress on or before August 5, 2019. We urge HHS to promptly comply with the judge’s ruling and restore to 340B hospitals all funds that have been unlawfully withheld.”
HHS has not issued a statement regarding Monday’s ruling and did not respond to a request for comment by time of publication.
The December ruling by Contreras did have a material impact on nonprofit hospitals, according to Moody’s Investor Service, which determined in early January that the reversion of the cuts would lead to improved operating performance.
340B Health, an advocacy group for the federal program, also issued a statement Tuesday afternoon applauding Contreras’ ruling.
“On behalf of the nearly 1,400 hospitals we represent that participate in 340B, we are pleased that the court has, once again, found that HHS exceeded its statutory authority by cutting what Medicare pays for outpatient drugs delivered to their patients,” Maureen Testoni, CEO of 340B Health, said in a statement. “The cuts made in 2018 and again in 2019 have reduced hospitals’ ability to care for those in need. The sooner this policy is reversed, the better hospitals will be able to serve the needs of patients with low incomes and those in rural communities. HHS must act quickly, as any further delay will only harm patients and the hospitals they rely on for care.”
Nearly 2,500 hospitals currently participate in the 340B Drug Pricing Program, which was created in 1992 to assist safety-net and low-income providers purchase prescription drugs.
A status report regarding HHS’ progress remedying the situation must be submitted to Judge Contreras by August 5.
For the First Time, Employed Docs Outnumber Self-employed Docs
https://www.healthleadersmedia.com/first-time-employed-docs-outnumber-self-employed-docs
The milestone continues a long-term trend that has shifted the distribution of physicians away from ownership of private practices.
KEY TAKEAWAYS
Employed physicians were 47.4% of all patient care physicians in 2018, up 6% points since 2012.
Self-employed physicians were 45.9% of all patient care physicians in 2018, down 7% points since 2012.
In the aggregate, 34.7% of physicians worked either directly for a hospital or in a practice at least partly owned by a hospital in 2018, up from 29.0% in 2012.
Employed physicians outnumber self-employed physicians for the first time in the United States, according to an updated study on physician practices by the American Medical Association.
“Transformational change continues in the delivery of healthcare and physicians are responding by reevaluating their practice arrangements,” AMA President Barbara L. McAneny, MD, said in a media release.
Employed physicians were 47.4% of all patient care physicians in 2018, up 6% points since 2012.
Self-employed physicians were 45.9% of all patient care physicians in 2018, down 7% points since 2012.
Such a dramatic shift is not unprecendented. Older AMA surveys show the share of self-employed physicians fell 14% points during a six-year span between 1988 and 1994.
Given the rate of change in the early 1990s, it appeared a point was imminent when employed physicians would outnumber self-employed physicians, but the shift took much longer than anticipated.
The AMA’s researchers said that history suggests that “caution should be taken in assuming current trends will continue indefinitely.”
The majority of patient care physicians (54%) worked in physician-owned practices in 2018 either as an owner, employee, or contractor. Although this share fell from 60% in 2012, the trend away from physician-owned practice appears to be slowing since more than half of the shift occurred between 2012 and 2014, the study said.
At the same time, there was an increase in the share of physicians working directly for a hospital or in a practice at least partly owned by a hospital.
Physicians working directly for a hospital were 8% of all patient care physicians, an increase from 5.6% in 2012. Physicians in hospital-owned practices were 26.7% of all patient care physicians, an increase from 23.4% in 2012.
In the aggregate, 34.7% of physicians worked either for a hospital or in a practice at least partly owned by a hospital in 2018, up from 29.0% in 2012.
Younger physicians and women physicians are more likely to be employed. Nearly 70% of physicians under age 40 were employees in 2018, compared to 38.2% of physicians age 55 and over.
Among female physicians, more were employees than practice owners (57.6% vs. 34.3%). The reverse is true for male physicians, more were practice owners than employees (52.1% vs. 41.9%).
As in past AMA studies, physicians’ employment status varied widely across medical specialties in 2018.
The surgical subspecialties had the highest share of owners (64.5%) followed by obstetrics/gynecology (53.8%) and internal medicine subspecialties (51.7%).
Emergency medicine had the lowest share of owners (26.2%) and the highest share of independent contractors (27.3%). Family practice was the specialty with the highest share of employed physicians (57.4%).
Most physicians still work in small practices, but this share has fallen slowly but steadily since 2012. In 2018, 56.5% of physicians worked in practices with 10 or fewer physicians compared to 61.4% in 2012.
The AMA report said the transition has been driven primarily by the shift away from very small practices, especially solo practices, in favor of very large practices of 50 or more physicians.
The new study is the latest addition to the AMA’s Policy Research Perspective series that examines long term changes in practice arrangements and payment methodologies.
“Transformational change continues in the delivery of healthcare and physicians are responding by reevaluating their practice arrangements. ”
Breaking: CPR to Require Prior Authorization
“No!” cries ICU physician
In breaking news that will infinitely complicate the already difficult process of attempting to resuscitate a patient, cardiopulmonary resuscitation (or CPR) will now require prior authorization.
The prevailing reaction to this news is best captured by Felicia Martin-Lowry, MD, a critical care physician at James Monroe University Hospital in Washington, as she crumbled into a burbling mess of defeat: “No … no … NOOOOOOOO!!!!”
Much like prior authorization requests for medications or other services, health care professionals will only learn about the need for a prior authorization right when CPR is initiated. The insurer will block CPR from continuing and the health care professional will need to go through the lengthy prior authorization process.
“We need to make sure that the health care team tried some other interventions before jumping straight into CPR,” explained a spokesperson for a major national health insurance company, who insisted on anonymity. “Expect us to ask questions like, did you try oxygen? Did you try IV fluids? Did you try an antibiotic? Did you try bicarb?”
The spokesperson went on to say that the checklist of questions will border on somewhere between 700 and 800 questions.
Insurance companies understand that CPR can be a life-saving measure. For that reason, if the insurer finds that all the appropriate steps were taken prior to the patient’s death, then they will be sure to expedite the prior authorization as an urgent request and make the decision on whether or not to approve CPR in no less than 14 days.
“Time is of the essence,” the spokesperson added, before reminding everyone that prior authorizations for CPR will only take place weekdays from 9 a.m. to 5 p.m.
In other news, Gomerblog has learned that insurers will soon require prior authorizations before physical exams and IV placement.
Once again, this post is from GomerBlog, a satirical site about healthcare.