https://www.bloomberg.com/view/articles/2017-03-17/the-wrong-way-to-lower-health-insurance-premiums

For proponents of the American Health Care Act, perhaps the most encouraging nugget in the Congressional Budget Office’s otherwise critical analysis is that insurance premiums could fall by 10 percent on average by 2026. Even this prediction is more mirage than reality, however, in part because of an obscure concept known as “actuarial value.”
As many opponents of the Republicans’ Obamacare replacement legislation have already noted, for many people, the decline in premiums would be smaller than the cutback in their subsidies, so they would still end up paying more. And in any case, the predicted fall in premiums partly reflects a troubling rise in the share of older Americans without insurance, a change that would shift the enrollment pool to younger, less expensive beneficiaries.
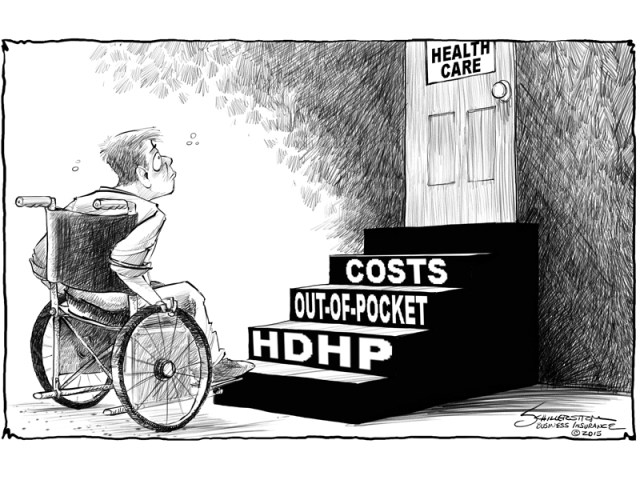
Another factor, however, has received less attention, though it is hidden in plain sight in the CBO analysis: The premium reduction would occur in no small part because the insurance products wouldn’t be as good. In other words, their actuarial value would fall.
An insurance policy’s actuarial value is the share of total health-care costs paid by the plan rather than the policy holder, through deductibles and copayments. A plan with an actuarial value of 80 percent will pick up, on average, 80 percent of the cost of care. Plans with higher actuarial values have higher premiums, not surprisingly, because they provide deeper insurance. And if a plan’s actuarial value is very low, it may not really qualify as insurance at all.
The Affordable Care Act sets minimum actuarial values for each of the four tiers of plans that can be sold on the exchanges; the lowest, for bronze plans, is about 60 percent. The new legislation would repeal these minimums.
In its analysis of the Republican proposal, the CBO found that insurers would offer lower-value policies “because they could offer a plan priced closer to the amount of the premium tax credit so that a younger person would have low out-of-pocket costs for premiums and would be more likely to enroll.” Similarly, insurers would hesitate “to offer plans with high actuarial values out of a fear of attracting a greater proportion of less healthy enrollees to those plans.” Since plans would still be required to cover 10 categories of essential health benefits, and since out-of-pocket limits would remain in place, plans would not dip too far below 60 percent, in the CBO’s estimation. But more plans would drop toward that level.
To see how big a deal this is, it is instructive to study the table toward the end of the CBO’s analysis, which calculates premiums under current law and under the AHCA. A 40-year-old single person could see his or her premium fall 7 percent — to $6,050, from $6,500. That’s only slightly less than the average 10 percent premium decline. Yet the actuarial value of the person’s plan would decline to 65 percent, from 70 percent or 87 percent, depending on his or her income.
To get some sense of what these lower actuarial values mean in terms of higher deductibles, we can look to the most recent Centers for Medicare and Medicaid Services calculator. It suggests that a plan with a $1,500 deductible, an 80 percent coinsurance rate (the plan pays 80 percent of costs above the deductible and below the maximum out-of-pocket threshold), and a $7,200 maximum out-of-pocket limit would have an actuarial value of 73 percent. The same plan with a $5,000 deductible would have an actuarial value of 61 percent. In other words, a decline in actuarial value of about 12 percentage points (not far from the average decline in the CBO examples) would raise the policy’s deductible by $3,500.
It’s no wonder that the premium for such a plan would be lower — in the same way that it’s no wonder a 12-ounce can of soda costs less than a 35-ounce bottle. It’s no great accomplishment to lower premiums by increasing other consumer costs.
As the CBO concluded, under the Republicans’ system, “individuals’ cost-sharing payments, including deductibles, in the nongroup market would tend to be higher than those anticipated under current law.” Indeed, according to an analysis from the Center for American Progress, average total costs to consumers would be significantly higher.
If you think that competition can fix this, note another problem that the CBO points out: Under Obamacare, the actuarial value requirements allow for easy comparison shopping; plan A can be directly compared with plan B. Under the Republican system, it would be harder to shop for a policy based on price.
Health-care reform is indeed complicated. Esoteric concepts like actuarial value have big effects on every family’s bottom line.