https://www.healthcarefinancenews.com/news/how-medicareadvantage-steers-silver-tsunami-coordinated-value-based-care

Today’s Medicare Advantage plans are flourishing and the Silver Tsunami is among the reasons.
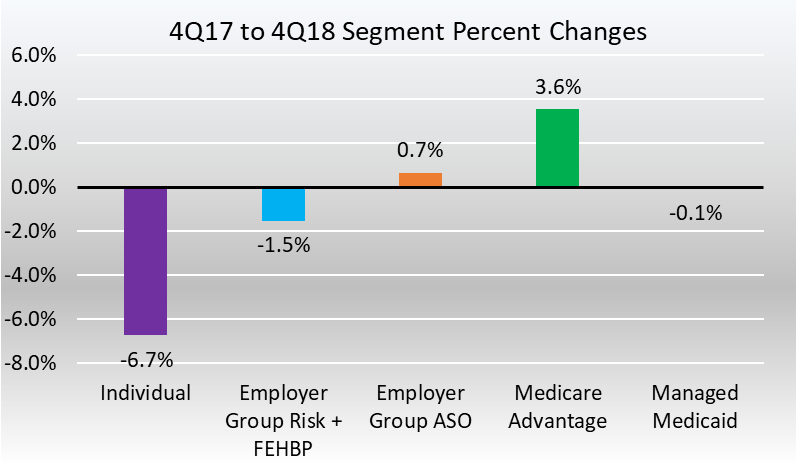
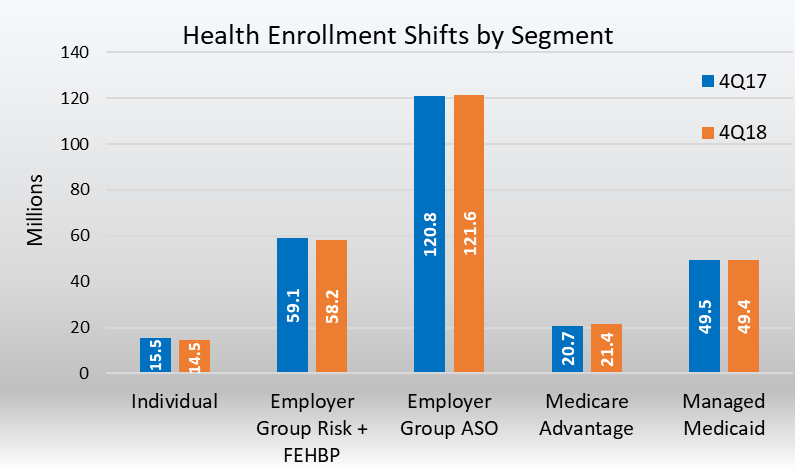
“Over the last four years, Medicare Advantage enrollment increased by more than 30 percent, while the number of people eligible for Medicare grew by about 18 percent,” said Steve Warner, vice president of Medicare Advantage Product for UnitedHealthcare Medicare and Retirement.
Other reasons for the growth: Innovative models from big insurers and upstarts alike that improve care for health plan members and drive revenue for payers as they look beyond fee-for-service.
IT STARTS WITH THE CONSUMER
Consumers are finding unique value in MA, both in terms of the quality of care and in the financial value.
Medicare Advantage, in fact, makes it easier for consumers to navigate the healthcare system and choose providers, in a way that traditional Medicare does not, said those interviewed.
“Actually it’s pretty hard to navigate the healthcare system on your own,” said Tip Kim, chief market development officer at Stanford Health Care. “Most Medicare Advantage plans have some sort of care navigation.”
Warner of UnitedHealth’s Warner added that Medicare Advantage also offers value and simplicity.
“It provides the convenience of combining all your coverage into one plan so you have just one card to carry in your wallet and one company to work with,” Warner said. “Most plans also offer prescription drug coverage and additional benefits and services not available through original Medicare, including dental, vision and fitness.”
REBRANDING FOR THE NEW ERA
MA plans did not emerge out of thin air. By another name, Medicare Advantage is managed care, a term that was the bane of healthcare during the height of HMOs in the 1980s.
“Medicare Advantage has rebranded ‘managed care’ to ‘care coordination,'” said consultant Paul Keckley of The Keckley Report. “Humana and a lot of these folks have done a pretty good job. Coordinating care is a core competence. Managed care seems to be working in this population.”
MA came along at the right time for CMS’s push to value-based care.
“I would suggest on the providers’ side, embracing Medicare Advantage is an opportunity to get off the fee-for-service mill,” said Jeff Carroll, senior vice president of Health Plans for Lumeris, which recently paired with Stanford Health Care on the Medicare Advantage plan, Stanford Health Care Advantage.
“Provider-sponsored Medicare Advantage plans are a way to put teeth into an accountable care organization,” Keckley added. “Medicare Advantage success is a silver tsunami among major tsunamis. Obviously it’s a profitable plan for seniors and profitable for underwriters. The winners in the process will get this to scale.”
MA is an innovative model that is not a government-run system, but a privately-run system essentially funded by the government.
PAYERS IN THE MA GAME
UnitedHealthcare has the largest MA market share of any one insurer. Twenty-five percent of Medicare Advantage enrollees are in a UnitedHealthcare MA plan, followed by 17 percent in Humana, 13 percent in a Blue Cross Blue Shield and 8 percent in Aetna, according to the Kaiser Family Foundation.
Numerous insurers, in fact, have gotten into the MA market, including Clover Health in San Francisco, a five-year-old startup which has Medicare Advantage as its only business.
Clover is a tech-oriented company that boasts machine learning models that can accurately predict and identify members at risk of hospitalization.
Because Clover focuses only on MA, it can do a better job at problem solving the needs of an older population, said Andrew Toy, president and CTO of Clover Health.
“The problems we face in Medicare Advantage are very different from a younger generation,” Toy said.
Forty percent of the older population is diabetic. Most seniors will be dealing with a chronic disease as they get older.
In other insurance, whether its individual or commercial, the lower cost of the healthier population offsets the cost of the sicker population. MA has no way to offset these costs. Plans can’t cherry-pick consumers or raise premiums for a percentage of the population.
What MA plans can do is design plans that fit the varying needs of the population. A plan can be designed for diabetics. For younger seniors or those not dealing with a chronic disease, a plan can be designed that includes a gym membership.
“All these plans are regulated,” Toy said. “We have the flexibility to move dollars around. We can offer a higher deductible plan, or a nutrition plan. The incentives for us in Medicare Advantage are different than the incentives in Medicare. CMS has explored giving us more leeway for benefits. Consumers have a choice while still having the guarantees of Medicare.”
Toy believes regular Medicare is more expensive because MA offers a more affordable plan based on what an individual needs.
“When you need it, we get more involved in that care,” Toy said, such as “weight control issues for diabetics.”
The drawbacks are narrower networks, though Toy said Clover offers an out-of-network cost sharing that is pretty much in line with being in-network.
UnitedHealthcare’s Medicare Advantage LPPO plans offer out-of-network access to any provider who accepts Medicare, Warner said.
UnitedHealthcare also offers a wide variety of low and even zero-dollar premium Medicare Advantage plans and annual out-of-pocket maximums, Warner said. By contrast, original Medicare generally covers about 80 percent of beneficiaries’ healthcare costs, leaving them to cover the remaining 20 percent out-of-pocket with no annual limit.
“From a consumer value proposition, it makes Medicare Advantage a better deal,” Kim said. “One is Part B, 20 percent of an unknown number. Knowing what the cost will be in a predictable manner is a preferable manner.”
Stanford Health Care launched a Medicare Advantage plan in 2013. Lumeris owned and operated its own plan, Essence Healthcare, for more than eight years. Stanford and Lumeris partnered on Stanford Health Care Advantage in northern California, using Lumeris technology to help manage value-based reimbursementand new approaches to care delivery through artificial intelligence-enabled diagnostic tools and other methods.
“We are not a traditional insurance company,” Kim said. “We’re thinking about benefits from a provider perspective. It’s a different outlook than an insurance company. By definition we’re local.”
MA MARKET STILL HAS ROOM TO GROW
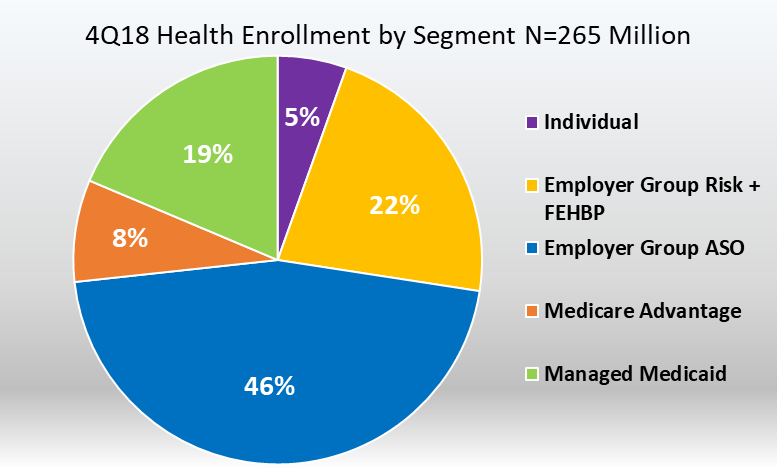
While the Medicare Advantage market is competitive, it is also under-penetrated, Brian Thompson, CEO for UnitedHealthcare Medicare & Retirement, said during a 2018 earnings report.
Currently, about 33 percent of all Medicare beneficiaries are in an MA plan, he added, but UnitedHealth sees a path to over 50 percent market concentration in the next 5-10 years.
It’s a path not so subtly promoted by the Centers for Medicare and Medicaid Services.
As a way to encourage insurers to take risk and get in the market, around 2009, CMS gave MA insurers 114 percent of what it paid for fee-for-service Medicare. The agency began decreasing those payments so that by 2017, traditional Medicare and MA became about even.
MA insurers instead thrive on their ability to tailor benefits toward wellness, coordinate care and contain costs within the confines of capitated payments, the essence of value-based care.
They have received CMS support in recent rate notices that gives them the ability to offer supplemental benefits, such as being able to target care that addresses the social determinants of health. Starting in 2020, telehealth is being added to new flexibility for these plans.
WHAT THE FUTURE MAY HOLD FOR MA
Medicare Advantage plans have expanded and, in so doing, opened innovative new options for plans and their customers alike at the same time that the ranks of people eligible for Medicare continues to swell.
So where is it all going?
Medicare Advantage is changing the way healthcare is paid and delivered to the point that Keckley and Toy agreed the future may not lie in Medicare for All, but in Medicare Advantage for all.
“I think a reasonable place to end, is in some combination where the government is involved in price control, combined with the flexibility of Medicare Advantage,” Toy said. “That’s really powerful.”