http://www.modernhealthcare.com/article/20171206/NEWS/171209899

Healthcare lobbyists are scrambling to win changes in congressional Republican tax legislation, as Senate and House GOP leaders race to merge their separate bills into something both chambers can pass on a party-line vote this month.
But provider, insurer and patient advocacy groups doubt they can convince Republicans to remove or soften the provisions they find most objectionable. They say GOP leaders are moving too fast and providing too little opportunity for healthcare stakeholders to provide input.
“It’s a madhouse,” said Julius Hobson, a veteran healthcare lobbyist with the Polsinelli law firm. “What you worry about is this will get done behind closed doors, even before they start the conference committee process.”
One factor that could slow the rush to pass the Tax Cuts and Jobs Act is the need to pass a continuing resolution this week to fund the federal government and prevent a shutdown. Unlike with the tax bill, Republicans need Democratic support for that, and it’s not clear they’ll make the concessions Democrats are demanding.
Industry lobbyists are particularly targeting provisions in the House and Senate tax bills limiting tax-exempt financing for not-for-profit hospitals and other organizations; repealing the Affordable Care Act’s tax penalty for not buying health insurance; ending corporate tax credits for the cost of clinical trials of orphan drugs; and taxing not-for-profit executive compensation exceeding $1 million.
If the ACA’s insurance mandate is repealed, “our plans will have to evaluate whether they can stay in the individual market or not based on what it does to enrollment and the risk profile of people who choose to stay,” said Margaret Murray, CEO of the Association for Community Affiliated Plans, which represents safety net insurers.
AARP and other consumer lobbying groups are fighting to save the household deduction for high healthcare costs, which the House version of the Tax Cuts and Jobs Act would abolish.
Healthcare lobbyists also are warning lawmakers that capping or ending the federal tax deduction for state and local taxes will force many states to cut Medicaid. Beyond that, they say slashing taxes and increasing the federal deficit will trigger immediate Medicare budget sequestration cuts that would hurt providers and patients, particularly in rural and low-income areas.
“One in three rural hospitals are at financial risk of closure, and sequestration would be devastating for them,” said Maggie Elehwany, vice president of government affairs for the National Rural Health Association. “I’d love to say our message is getting through. But Congress is completely tone-deaf on how troubling the situation in rural America is.”
Hospital groups, led by the American Hospital Association, are battling to preserve tax-exempt bond financing for not-for-profit organizations, which the House bill would zero out. While the Senate bill would keep the tax exemption for interest income on new municipal private activity bonds, both the Senate and House bills would prohibit advance re-funding of prior tax-exempt bond issues.
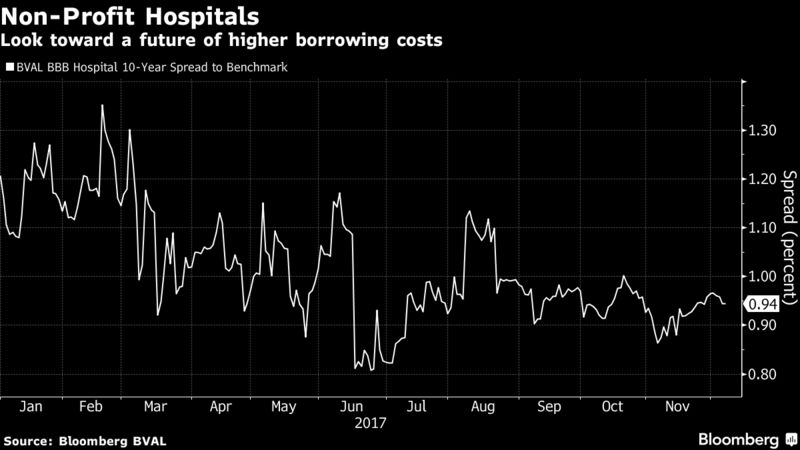
Hospitals say ending or limiting tax-exempt bond financing would jack up their borrowing costs and hurt their ability to make capital improvements, particularly for smaller and midsize hospital systems. The Wisconsin Hospital Association projected that ending tax-exempt bond financing would increase financing costs by about 25% every year.
According to Merritt Research Services, outstanding end-of-year hospital debt totaled nearly $301 billion in long-term bonds and nearly $21 billion in short-term debt. Nearly all of that debt was issued as tax-exempt bonds.
Suggesting a possible compromise, Rep. Kevin Brady (R-Texas), chairman of the House Ways and Means Committee, said Tuesday that he saw “a good path going forward” to preserve tax-exempt private activity bonds “that help build and enhance the national infrastructure.”
But Hobson raised questions about Brady’s comments. “What is his definition of infrastructure?” he asked. “It suggests they may move away from a blanket repeal, but it doesn’t tell me where they’re going.”
If Republicans decided not to repeal the tax exemption for municipal bond interest income, however, they would have to scale back some of their pet tax cuts for corporations and wealthy families, even as they feel pressure to ease unpopular provisions such as ending the deductibility of state and local taxes. That could make it hard for hospital lobbyists to gain traction on this issue.
“There are a lot of giveaways in the bills that don’t leave a lot of room to recoup the money you lose,” Hobson said.
Some lobbyists hold out a faint hope that the Republicans’ tax cut effort could collapse as a result of intra-party differences, as did their drive to repeal and replace the Affordable Care Act.
One possibility is that Maine Sen. Susan Collins flips and votes no on the tax cut bill emerging from the conference committee if congressional Republicans fail to pass two bipartisan bills she favors to stabilize the individual insurance market.
Collins said she’s received strong assurances from Senate Majority Leader Mitch McConnell and President Donald Trump that they will support the bills to restore the ACA’s cost-sharing reduction payments to insurers and establish a new federal reinsurance program that would lower premiums.
But the fate of those bills is in doubt, given that House Speaker Paul Ryan (R-Wis.) was noncommittal this week, while House ultraconservatives have come out strongly against them.
Collins conceivably could be joined by Alaska Sen. Lisa Murkowski, who also said she wants to see the market stabilization bills passed. If Tennessee Sen. Bob Corker, who voted no on the tax cut bill over deficit concerns, remains opposed, those three GOP senators could sink the tax bill.
“We’d all like to see Collins pull her vote,” Hobson said. “It was always clear that the deal she cut with McConnell won’t fly on the House side.”
One healthcare lobbyist who didn’t want to be named said there may be a deal in the works for House conservatives to support market-stabilization legislation in exchange for lifting budget sequestration caps on military spending.
But healthcare lobbyists are not holding their breath on winning major changes or seeing the tax bill collapse.
“There are chances they won’t reach a deal,” said Robert Atlas, president of EBG Advisors, which is affiliated with the healthcare law firm Epstein Becker Green. “By the same token, Republicans are so determined to pass something that they might just come together.”