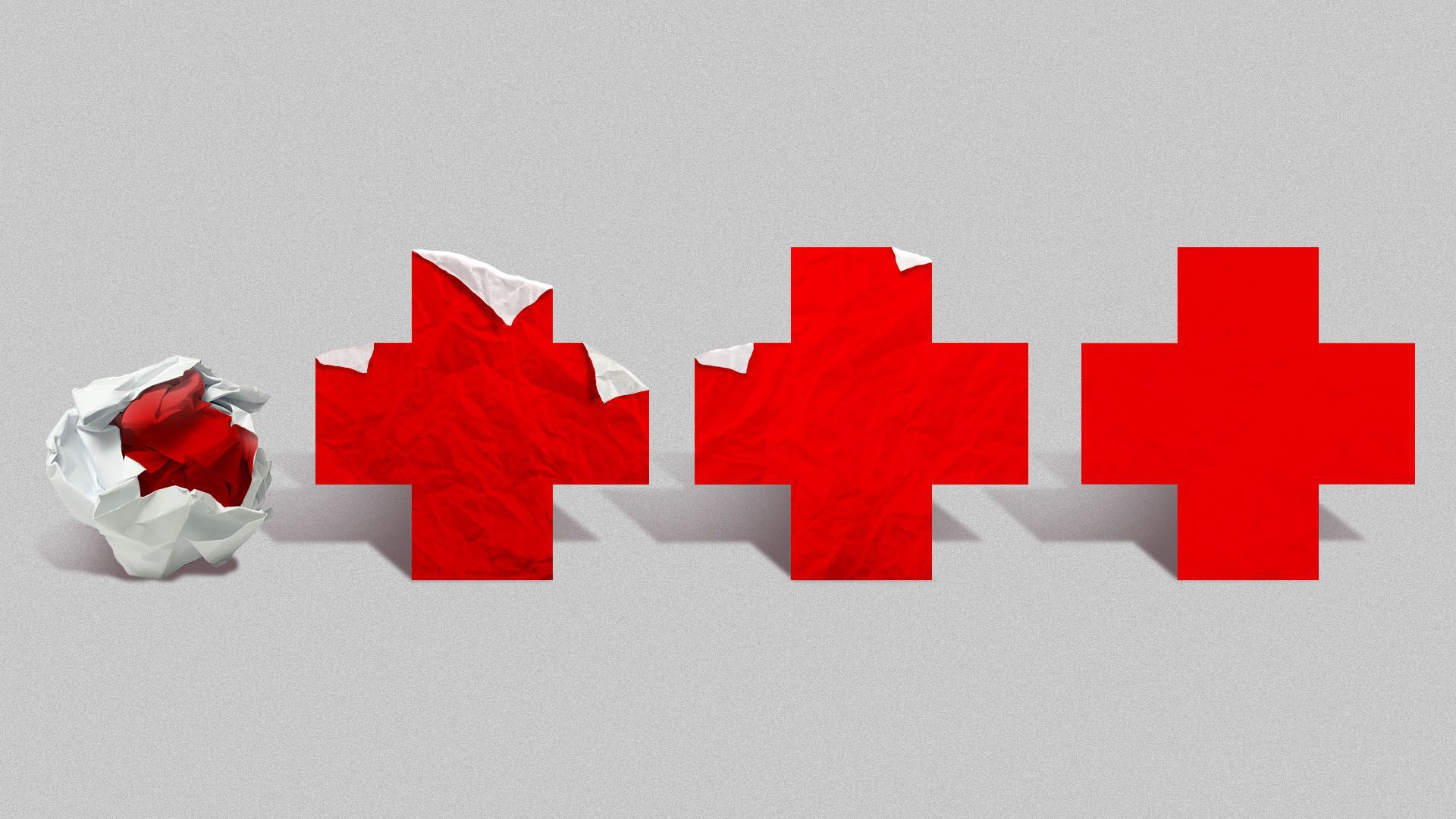
Doctors and hospitals have learned a lot about how best to treat people infected with the coronavirus in the months since the pandemic began.
Why it matters: Better treatment means fewer deaths and less pain for people who are infected, and research into pharmaceutical treatments is advancing at the same time as hospital care.
The big picture: Some of the simplest changes have been the most effective. For example, doctors have learned that flipping patients onto their stomachs instead of their backs can help increase airflow to the lungs.
- Providers also now prefer high-flow oxygen over ventilators, despite the early focus on ventilator supply.
- “If you can avoid ventilation, it is preferred if someone is able to breathe on their own and you just help them out by giving them more oxygenated air to breathe,” said Janis Orlowski, chief health care officer of the Association of American Medical Colleges.
Researchers have also discovered new utility in old drugs.
- Dexamethasone, a cheap steroid used to treat inflammation, has been found to reduce deaths by one-third among patients on ventilators and one-fifth among those on oxygen.
- Preliminary data has shown that remdesivir, an antiviral, probably doesn’t save seriously ill patients’ lives, but can help others get out of the hospital a few days earlier. “Anyone who has evidence of lung injury or needing oxygen, we give it,” said Armond Esmaili, a hospitalist at the University of California San Francisco Medical Center.
- Doctors have also learned to put all COVID patients on drugs to prevent blood clots, Esmaili said.
What they’re saying: There’s still a lot doctors and scientists don’t know about the virus, but they say they’ve come along way since February and March, when they were essentially flying blind.
- “It was very scary, just to give you the subjective feeling, of caring for patients and talking with patients and their families and a lot of the time saying, ‘We don’t know a lot about this disease. We don’t know how you’re going to do,’” Esmaili said.
Between the lines: Hospitals are also able to provide better care when they’re not overwhelmed with patients.
- New York’s hospitals were so overwhelmed in the spring that they brought in employees to work well outside of their specialties. In some hospitals’ emergency rooms, patient-to-nurse ratios rose to more than 20 to 1, the NYT reports — five times the recommended ratio.
- “Really attentive-level care is important,” Esmaili said.“It’s not that hard to imagine that when you have the resources and you’re not overburdened with a massive amount of patients that patients are going to get better care.”
What we’re watching: These advances in treatment protocols will only go so far, especially if hospitals in states like Florida, Arizona and Texas become too full to put them into practice.
- In states with rising case counts, “I think you’re going to see mortality rates increase there because of that phenomenon of hospitals being unable to deliver optimal care, because they don’t have the staffing,” said James Lawler, an infectious disease specialist at the University of Nebraska Medical Center.
- “You don’t want your ICU nurse to have to take care of five or six patients at the same time,” he said.




