Category Archives: Employee Layoffs
Cartoon – Managing the Downturn
Cartoon – Making the Leap
Cartoon – Becoming Redundant
Cartoon – Place Your Bets
Is a ‘white-collar’ recession coming?

The jobs of young professionals in several white-collar industries are particularly vulnerable as companies scale back hiring plans, pull job listings and lay off workers.
Sixty-five percent of employers see a recession coming and many are taking steps to prepare, according to a survey by Principal Financial Group. If there is a recession, white-collar industries are likely the most vulnerable, said William Lee, PhD, chief economist at the Milken Institute, according to Bloomberg.
“The entry-level white-collar guy is going to have to watch out. That’s going to be the surprise in this downturn,” Dr. Lee said, according to Newsweek.
A Challenger, Gray and Christmas survey revealed companies are preparing for a recession by reducing business travel, laying off staff and implementing hiring freezes.
Many industries, including technology, banking and business services, have staffing numbers that are far above pre-pandemic levels, and the layoffs have already begun, according to Bloomberg. Social media platform Snap, Netflix and Re/Max Holdings are a few of the companies that have recently announced staff reductions.
Read the full Bloomberg article here.
Read the full Newsweek article here.
Ohio hospital to lay off 978 employees
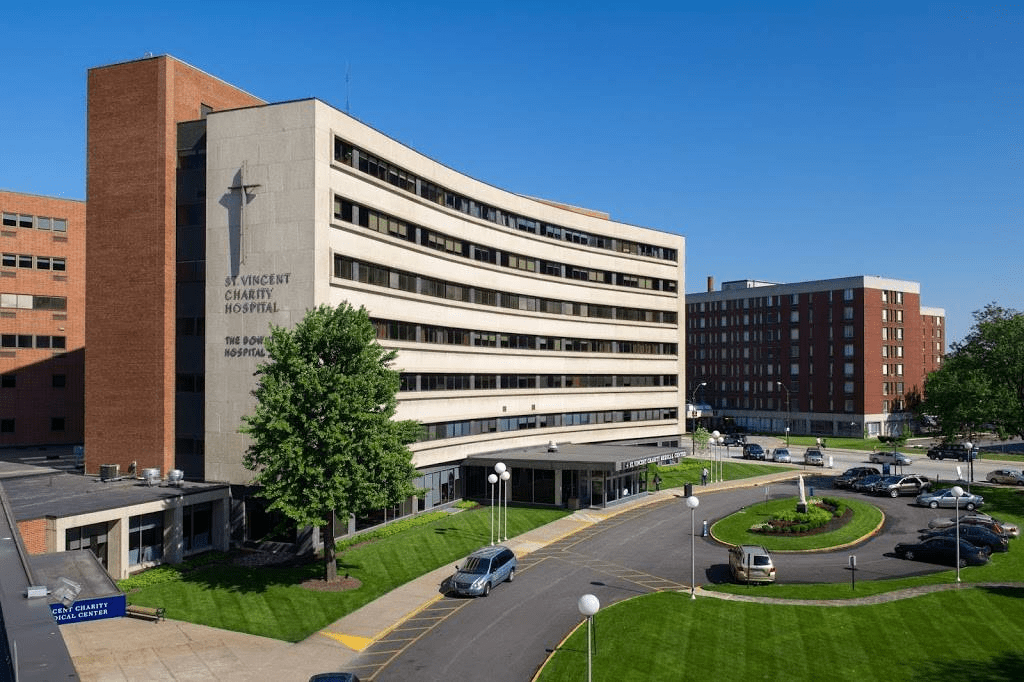
St. Vincent Charity Medical Center in Cleveland will lay off 978 workers when it ends many services in November, according to a notice filed with state regulators.
The hospital, part of Sisters of Charity Health System, is ending inpatient care and most other services in November. After the transition, the facility will offer outpatient behavioral health, urgent care and primary care.
The health system attributed the changes to several factors, including the rise in demand for outpatient care, declining inpatient volume and shifts in the healthcare industry over the last 10 years that have made it challenging to continue operating St. Vincent Charity Medical Center as an acute care hospital.
The changes will result in 978 employees being laid off on Nov. 15, according to the notice filed with state regulators.
“This extremely difficult decision is being made with deep respect and gratitude for our caregivers, and we regret the direct impact this decision will have on those individuals,” reads the layoff notice from the hospital. “Unfortunately, the COVID pandemic, the changing health care landscape, and declining inpatient volumes have led to significant financial challenges that became impossible to overcome.”
The layoffs will affect 446 full-time workers, 264 part-time employees and 268 workers who are called into work as needed, a spokesperson for Sisters of Charity Health System told Becker’s Hospital Review.
How hospitals are cutting back to reduce costs

Despite efforts to curtail high expenses, rising inflation and declining federal aid have led many hospitals to begin laying off workers and cutting certain services, Katheryn Houghton writes for Kaiser Health News.
Hospital costs have skyrocketed during the pandemic
At the beginning of the pandemic, hospitals’ financial challenges were largely related to the costs of responding to Covid-19 and missed revenue due to delayed care. However, hospital leaders now say their financial situations are a result of the omicron surge, rising inflation, and growing staffing challenges.
Many hospitals received millions of dollars in federal aid during the pandemic, but much of that money has since dwindled. For example, Bozeman Health said it received $20 million in aid in 2020, but this decreased to $2.5 million in 2021 and around $100,000 in 2022.
Many health systems say low surgery volumes, high supply costs, higher acuity patients, and languishing investments have all contributed to their declining revenues and growing expenses. In particular, labor costs have increased significantly during the pandemic, particularly as staffing shortages pushed hospitals to use more contract workers.
“If you talk with just about any hospital leader across the country, they would put workforce as their top one, two, and three priorities,” said Akin Demehin, senior director of quality and patient safety policy for the American Hospital Association.
According to Brad Ludford, CFO at Bozeman Health, the system spent less than $100,000 a month on contract workers before the pandemic, but that has now increased to roughly $1.4 million a week. Overall, the health system’s labor costs have increased around 12% from the same time last year, reaching around $20 million a month, during the first half of the year.
John Romley, a health economist and senior fellow at the Schaeffer Center for Health Policy and Economics at the University of Southern California, said some hospitals are likely now losing money, particularly with less federal aid coming in and growing inflation on top of their already high expenses.
For example, Bozeman Health president and CEO John Hill said the health system spent $15 million more than it earned in the first six months of the year. Several other health systems, including Providence, have also reported net operating losses this year.
Hospitals lay off workers, cut services to help reduce expenses
To reduce expenses, many hospitals are beginning to lay off workers and cut certain services, which has forced some patients to travel farther to receive care.
For example, Bay Area Hospital in Oregon recently ended 56 contracts with travel nurses and cut its inpatient behavioral health services due to the high costs of quickly filling vacant positions. Hospitals in California, Mississippi, New York, Oregon, and other states have also had to reduce the sizes of their workforces.
St. Charles Health System, headquartered in Bend, Oregon, laid off 105 workers and eliminated 76 vacant positions in May. The system’s CEO at the time, Joe Sluka, said, “It has taken us two pandemic years to get us into this situation, and it will take at least two years for us to recover.”
Similarly, Bozeman Health has laid off 28 workers in leadership positions and has not been able to provide inpatient dialysis at its largest hospital for months.
According to Hill, Bozeman took several other measures before deciding to cut jobs, including stopping out-of-state business travel, readjusting workloads, and reducing executive compensation. At the same time, it worked to transition contract workers to full-time employees and offered existing staffers a minimum-wage increase.
However, “[i]t still has not been enough,” Hill said. The health system currently has 487 open positions for essential workers.
According to Vicky Byrd, an RN and CEO of the Montana Nurses Association, hospitals should be offering longtime employees the same incentives they use to recruit new workers, such as bonuses for longevity and premium pay for taking extra shifts, to increase retention.
“It’s not just about recruiting — you can get anybody in the door for $20,000 bonuses,” Byrd said. “But how are you going to keep them there for 10 or 20 years?”
Going forward, some hospitals are considering automating more of their services, such as allowing patients to order food through an iPad instead of an employee, and are trying to adjust workloads, including having more flexible schedules, to retain their current workers.
“Now that we’ve adapted to life with covid in many regards in the clinical setting, we are dealing with the repercussions of how the pandemic impacted our staff and our communities as a whole,” said Wade Johnson, CEO of St. Peter’s Health.
Providence restructures leadership team, cuts executive jobs
https://www.healthcaredive.com/news/providence-job-cuts/627660/

Providence said Tuesday it is restructuring and reducing executive roles amid persistent operating challenges spurred by the COVID-19 pandemic.
Providence said it will reduce its regional executive teams to three divisions from seven. The Washington-based nonprofit health system also has plans to consolidate three clinical lines of business — physician enterprise, ambulatory care network and clinical institutes — down to one executive leadership team.
“We began this journey before the pandemic, but it has become even more imperative today as health systems across the country face a new reality,” Providence President and CEO Rod Hochman said in a statement.
The new operating model is aimed at protecting direct patient care staff and other essential roles, Melissa Tizon, vice president of communication, told Healthcare Dive.
It’s unclear how many roles will be eliminated as part of the restructuring. Providence did not provide a specific number of job reductions.
Erik Wexler, former president of strategy and operations in Providence’s southern regions, will step into a new role as chief operating officer and will oversee the three new divisions.
Kevin Manemann will serve as division chief executive of the South region, which includes operations in Southern and Northern California.
Joel Gilbertson, division chief executive for the central region, will oversee operations in Eastern Washington, Montana, Oregon, Texas and New Mexico.
Guy Hudson will lead the North Division, which includes operations in Western Washington and Alaska. Hudson will keep his role as president and CEO of Swedish Health Services in Seattle.
David Kim, an executive vice president, will lead the three clinical business lines that were consolidated under one leadership team.
The shakeup comes after Providence reported in March that its operating loss doubled in 2021, reaching $714 million as operating expenses climbed 8% for the year.
The system said it treated more patients who were sicker and required a higher level of care than in 2020 and, at the same time, struggled with labor shortages.
NorthBay Health plans to eliminate 7% of its workforce

Fairfield, Calif.-based NorthBay Health announced July 11 that it will cut 7 percent of its workforce following continued financial strains, the Daily Republic reported July 12.
“The harsh reality is a number of factors contributed to NorthBay’s economic headwinds, including reduced volumes; skyrocketing prices for supplies, drugs and medical devices; the continuing need to rely on expensive temporary workers; and the rising number of Medicare and Medi-Cal patients whose care is not fully covered by government payments,” B. Konard Jones, president and CEO of NorthBay Health, said in a press release shared with the Daily Republic.
This 7 percent encompasses full-time positions or multiple part-time positions that equate to full-time hours. NorthBay Health said that 190 full-time positions will be cut in total.
Mr. Jones added that the healthcare system has a plan in place to get its budget back on track, but details of that plan have not been revealed at this time.
So far, NorthBay Health has already cut senior management positions by 20 percent. It is likely more positions will be cut in the future, according to the Daily Republic.
NorthBay Health is an independent, nonprofit healthcare system with a medical center in Fairfield, Calif., a hospital in Vacaville, Calif., and multiple specialty care clinics throughout Solano County. It was formerly known as NorthBay Healthcare.