https://www.yahoo.com/lifestyle/respiratory-virus-activity-high-rising-192815114.html

As seasonal virus activity surges across the United States, experts stress the importance of preventive measures – such as masking and vaccination – and the value of treatment for those who do get sick.
Tens of thousands of people have been admitted to hospitals for respiratory illness each week this season. During the week ending December 23, there were more than 29,000 patients admitted with Covid-19, about 15,000 admitted with the flu and thousands more with respiratory syncytial virus, or RSV, according to data from the US Centers for Disease Control and Prevention.
Nationally, Covid-19 levels in wastewater, a leading measure of viral transmission, are very high – higher than they were at this time last year in every region, CDC data shows. Weekly emergency department visits rose 12%, and hospitalizations jumped about 17% in the most recent week.
And while Covid-19 remains the leading driver of respiratory virus hospitalizations, flu activity is rising rapidly. The CDC estimates that there have been more than 7 million illnesses, 73,000 hospitalizations and 4,500 deaths related to the flu this season, and multiple indicators are high and rising.
RSV activity is showing signs of slowing in some parts of the US, but many measures, including hospitalization rates, remain elevated. Overall, young children and older adults are most affected.
“It’s a wave of winter respiratory pathogens, especially respiratory viruses. So it’s Covid, it’s flu, and we can’t diminish the importance of RSV,” said Dr. Peter Hotez, dean of the National School of Tropical Medicine at the Baylor College of Medicine. “So it’s a triple threat, and arguably a fourth threat because we also have pneumococcal pneumonia, which complicates a lot of these virus infections.”
Respiratory virus activity has been on the rise for weeks. Now, flu-like activity is high or very high in two-thirds of the United States, including California, New York City and Washington, as well as throughout the South and Northeast, according to the CDC.
“Remember, all of these numbers are before people got together for the holidays,” Hotez said. “So don’t be disappointed or surprised that we even see a bigger bump as we head into January.”
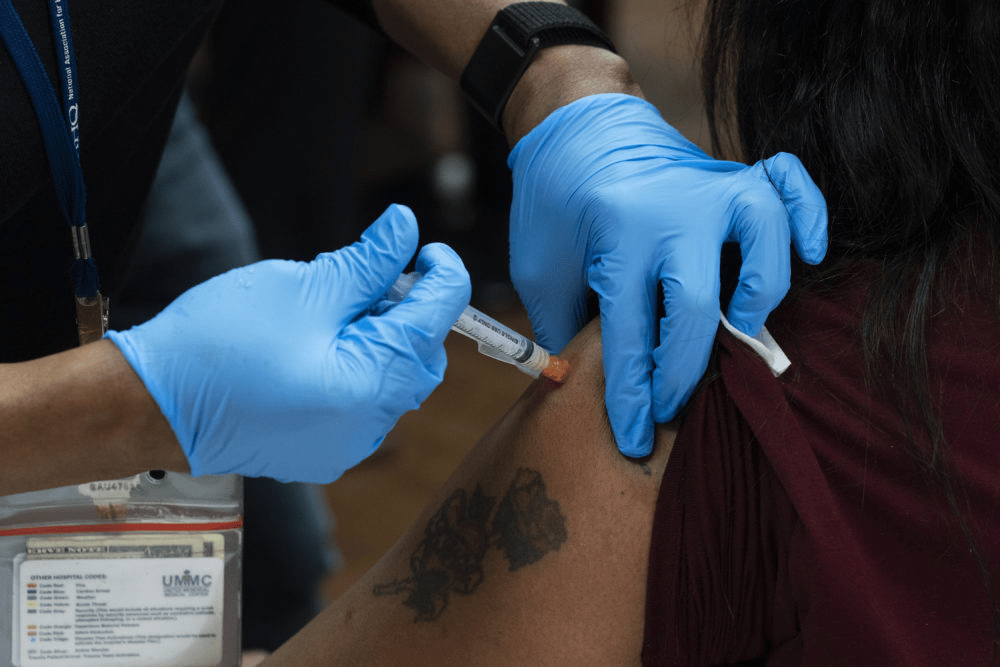
Vaccines can help prevent severe illness and death, but uptake remains low this season – despite a historic first, with vaccines available to protect against each of the three major viruses. Just 19% of adults and 8% of children have gotten the latest Covid-19 vaccine, and 17% of adults 60 and older have gotten the new RSV vaccine, CDC data shows. Less than half of adults and children have gotten the flu vaccine this season.
“We have, as a population, underutilized both influenza and the updated Covid vaccines, unfortunately,” said Dr. William Schaffner, an infectious disease expert at Vanderbilt University. “But it’s not too late to get vaccinated, because these viruses are going to be around for a while yet.”
According to the CDC, hospital bed capacity remains “stable” nationally, including within intensive care units. But with high levels of respiratory viruses, hospitals in at least five states are returning to requiring masks.
Mass General Brigham spokesman Timothy Sullivan said it will require masking for health-care staff who interact directly with patients starting Tuesday, and patients and visitors will be “strongly encouraged to wear a facility-issued mask.”
In Wisconsin, UW Health and UnityPoint Health – Meriter have expanded mask policies to cover more people. UW requires all staff, patients and visitors to wear a mask for patient interactions in clinic settings, including waiting areas and exam rooms.
UnityPoint Health – Meriter says masks continue to be required for team members and visitors in patient rooms.
Bellevue, a public hospital in New York City, said on social media last week that it had reinstated its mandatory masking policy due to an uptick in respiratory illnesses.
In Pennsylvania, the University of Pittsburgh Medical Center has required everyone to wear a mask when entering or inside since December 20. The systemwide masking policies were adjusted to “address the increase of respiratory virus cases” but may change when there is a “marked decrease in respiratory health cases,” according to the health care system.
An order posted last week by the Los Angeles County Health Officer requires all health-care personnel and visitors to mask while in contact with patients or in patient-care areas, based on the CDC’s categorization of Covid-19 hospital admission levels.
During the week ending December 23, more than 230 US counties were considered to have “high” levels of Covid-19 hospital admissions, defined by the CDC by at least 20 new hospital admissions for every 100,000 people. Nearly a thousand other counties, about a third of the country, have “medium” Covid-19 hospital admission levels, with at least 10 admissions for every 100,000 people.
Vaccines and masks can help reduce the risk of severe illness before getting sick, but treatments are also available to help prevent people from getting very sick if they do become infected.
Antiviral treatments for Covid-19, such as Paxlovid, and flu, such as Tamiflu, can be especially helpful for people who are more likely to get very sick, including people who are 50 or older and those with certain underlying conditions, such as a weakened immune system, heart disease, obesity, diabetes or chronic lung disease.
“If more people at higher risk for severe illness get treatment in a timely manner, we will save lives,” the CDC said in a recent blog post. But “not enough people are taking them.”
Seasonal respiratory virus activity can be hard to predict, but CDC forecasts suggest that hospitalization rates will continue at elevated levels for weeks and that this season, overall, will probably result in a similar number of hospitalizations as last season.
“One of the ways to help us all go into a happy new year is for us to be as protected as we can against these viruses,” Schaffner said.
“Of course, I continue to recommend vaccination, prudent use of the mask by high-risk people and, should you become sick, do not go to work and spread the virus further. Call your health care provider, because you may have some treatment available that will get you healthier sooner.”